* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Ulcerative colitis - Developing Anaesthesia
Survey
Document related concepts
Transcript
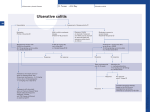
ULCERATIVE COLITIS Introduction Ulcerative colitis (UC) is a mucosal disease of the GIT, which is confined to the colon. It is a chronic relapsing disease of presumed autoimmune aetiology. Pathophysiology Inflammatory changes are continuous and extend from the rectum for a variable distance towards the caecum. The diagnosis is made by demonstrating: ● The endoscopic features of colitis at colonoscopy And ● The histological features of colitis on examination of tissue biopsy samples. And ● Excluding known infectious causes of colitis by stool examination. Complications: Recognized complications of ulcerative colitis include: Acute complications: 1. Fluid and electrolyte loss. 2. Blood loss with anaemia. 3. Sepsis, including: 4. ● Local abscess formation. ● Perforation of the GIT with consequent peritonitis ● Septicemia Toxic megacolon. Long term complications: 5. Stricture formation. 6. Fistula formation. 7. Malignant change in the long term. Clinical Assessment The aims of clinical assessment in the ED will be: ● Establish how unwell the patient is. ● Look for possible serious complications. ● Rule out alternative diagnoses. ● Decide on the need for admission. Important points of history 1. Establish the patient’s normal pattern of disease. 2. Establish the patient’s usual maintenance drug regime. 3. Enquire as to who the patients usual specialist is, (liaison will often be necessary when planning treatment) 4. Establish the nature of the symptoms that has caused the patient to present to hospital. Important points of examination: 1. Vital signs. 2. Hydrations status. 3. Look for signs of sepsis. 5. Check for signs and degree of GIT bleeding. 4. Abdominal examination: ● Look for signs of a surgical complication such as perforation or peritonitis. Assessment of Severity: It is important to detect the patient with severe exacerbation of disease as these patients require hospital admission and specialist consultation. Patients with septic or surgical complications also need to be detected. Severe exacerbation of disease is defined by the presence of: 1 ● More than 8 bloody stools per day Plus at least one of: ● Temperature greater than 37.5oC ● Pulse rate greater than 100/minute ● Haemoglobin less than 100 g/L ● Serum albumin less than 35 g/L. Investigations On ED presentation the investigations that will be needed will be guided by: ● How unwell the patient is. ● The index of suspicion for any given complication. ● The need to rule out alternative diagnoses. Blood tests: 1. FBE: ● 2. CRP: ● 3. This is important to assess disease activity or secondary infective complications. U&Es / glucose: ● 4. White cell count will be elevated in increased activity or secondary infective complications. LFTs: In particular check for hypokalemia. ● 5. Albumin levels in particular, which can be an indicator of severity. Others as clinically indicated: ● Blood cultures. ● Coagulation screens. ● ABGs Plain radiography: CXR/ AXR, erect and supine looking for: ● Obstruction. ● Perforation. ● Toxic megacolon. CT imaging: This is the best investigation when: ● The patient is very unwell. ● Severe secondary complications are suspected ● The diagnosis is unclear. Management The aims of drug therapy are to induce remission in active disease and to maintain remission and prevent relapse with maintenance therapy. The severity of the disease and the site(s) of the affected colon are used to determine which agents may be used and their route of administration. In general terms, if the disease is: Mild: Topical therapy is often sufficient for left-sided disease or proctitis or oral aminosalicylates and sulfasalazine agents. Moderate: Oral steroid therapy is used. Severe or extensive: Oral or intravenous steroid or immunosuppressive therapy or surgical intervention may be necessary. Agents currently used in the treatment of ulcerative colitis include: 1. Aminosalicylates and sulfasalazine: ● Combination preparations of these two agents are used in mild disease ● Aminosalicylates preparations without the sulfa agent are also available for those intolerant of sulfa agents. ● These agents are effective in inducing remission in active colitis or proctitis. The response to oral aminosalicylates is dose-related and some patients respond to high doses of oral aminosalicylates alone, although the response may be delayed. Patients who are on maintenance doses of aminosalicylates may benefit if the dose is increased during a flare 2. 3. Steroids: ● Oral and local preparations are available for the treatment of mild to moderate disease. ● Steroids are also effective in inducing remission but have no role as maintenance therapy because they do not prevent relapse and they have unacceptable long-term adverse effects Immunosuppressive agents (azathioprine and mercaptopurine) ● These are effective for both remission induction and maintenance therapy, but are associated with significant adverse effects and take up to 3 to 6 months to achieve their maximal benefit. Severe Ulcerative Colitis Exacerbation: Management of severe exacerbations of ulcerative colitis includes: 1. 2. IV fluid resuscitation: ● The immediate priority will be fluid resuscitation. ● With IV access takes bloods and do an ECG, (look for hypokalemia) Antibiotics: IV antibiotics should be given urgently in patients who are: 3. ● Toxic/ septicemic ● Have suspected toxic megacolon, (see separate guidelines) ● Have suspected surgical complications, such as peritonitis or gut perforation. Correct electrolyte disturbance: ● Hypokalemia in particular, and hypoglycaemia. 4. Nil orally. 5. Antidiarrhoeal agents. ● 6. Loperamide, other antidiarrhoeal and anticholinergic agents, (such as buscopan) should be avoided in severe disease as they may precipitate toxic megacolon. Analgesia: ● Narcotic analgesics should be used with caution. 7. Other supportive care as indicated. 8. Surgical referral: ● 9. Early surgical review is important in all unwell patients in order to rule out a surgical complication. Medical management: This will need to be guided by specialist gastroenterologist advice. Medical treatment options include: ● IV hydrocortisone or IV methylprednisolone are used ● IV cyclospsorin may be considered in specialist centres.