* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Streptococcal Pharyngitis - Intermountain Healthcare
Survey
Document related concepts
Transcript
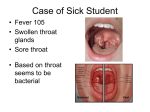
Care Process Model JANUARY 2014 DIAGNOSIS AND MANAGEMENT OF Streptococcal Pharyngitis This care process model (CPM) was developed by Intermountain Healthcare’s Antibiotic Stewardship team and Primary Care Clinical Program. Based on expert opinion and the Infectious Disease Society of America IDSA Clinical Practice Guidelines, it provides best-practice recommendations for diagnosis and management of group A streptococcal pharyngitis (strep) including guidance for when and which antibiotics should be used. KEY POINTS • Accurate diagnosis can prevent serious complications. When strep is present, appropriate antibiotics can prevent acute rheumatic fever, peritonsillar abscess, and other invasive infections. IDSA Treatment also prevents spread of infection and improves clinical symptoms and signs for the patient. GOALS • Select appropriate antibiotics for patients who meet the diagnostic criteria for a group A strep throat infection. • Reduce the unnecessary use of antibiotics for an unclear diagnosis of strep and for strep carriers. • Differentiating between a patient with an active strep infection and a patient who is a strep carrier with a viral illness (that prompts a strep culture) is challenging. Treating patients for active strep infection when they are only carriers can result in overuse of antibiotics. Approximately 20% of asymptomatic school-aged children may be strep carriers, and a throat culture during a viral illness may be positive but not need treatment. IDSA Prescribing repeat antibiotics will not help these patients and can contribute to antibiotic resistance. • For adult patients, routine overnight cultures after a negative rapid strep test are unnecessary in usual circumstances because the risk for acute rheumatic fever is exceptionally low in adults. IDSA Physicians may continue to use overnight throat cultures when the patient’s risk score is high or if the patient is at high risk due to contact or employment (e.g., teachers, family member with strep, etc.). Why Focus ON STREPTOCOCCAL PHARYNGITIS? • Antibiotic prescribing for sore throat has dropped, but not enough. Only about 10% of patients seeking care for sore throat have strep, but antibiotics are still prescribed about 60% of the time. Prescription rates dropped from 80% to 70% around 1993 and to 60% around 2000, and have remained stable since then. JAMA • Unnecessary antibiotic prescribing is costly and dangerous. From 1997 to 2010, the financial cost of unnecessary antibiotic prescribing to adults with sore throat was about $500 million in the United States. Antibiotics can also be expensive for patients and can have negative side effects. Between 5% and 25% of patients on antibiotics develop diarrhea, and 1 in 1,000 visit an emergency department for a serious adverse drug event. JAMA GermWatch is Intermountain’s source for up-to-date information about infectious diseases currently circulating in Utah communities. For physicians: intermountainphysician.org/gw For parents and patients: germwatch.org The inside pages of this tool provide algorithms and associated notes for adult and pediatric patients, and can be folded open and posted in your office or clinic. The back page summarizes identification and treatment of streptococcal pharyngitis carriers. DIAGNOSIS AND MANAGEMENT OF Streptococcal Pharyngitis – Pediatric ALGORITHM: PEDIATRIC DIAGNOSIS AND TREATMENT Recommend symptomatic relief to all patients. IMPORTANT: Do not prescribe antibiotics for strep without a strep test. TEST: Obtain rapid strep test (b) (+) (-) TEST: Obtain throat culture (c) END. (-) Discontinue antibiotic if prescribed. A T R I C Signs and Symptoms of Streptococcal Pharyngitis (a) Streptococcal pharyngitis Viral pharyngitis •• Sudden onset of sore throat •• Age 5–15 years (most common) •• Fever •• Headache •• Nausea, vomiting, abdominal pain •• Tonsillopharyngeal inflammation •• Patchy tonsillopharyngeal exudates •• Palatal petechiae •• Tender nodes •• Winter and early spring presentation •• History of exposure to strep pharyngitis •• Scarlatiniform rash •• Edematous uvula •• Conjunctivitis •• Coryza •• Cough •• Diarrhea •• Hoarseness •• Discrete ulcerative stomatitis •• Viral exanthema For a child under 3, obtain an RADT only when the child has symptoms of strep/when the clinical picture is strongly suggestive of strep. • RADTs are highly specific; positive RADTs do not necessitate a back-up culture. • Testing is not recommended for patients with overt viral features (see table above).IDSA • Do not test asymptomatic contacts (e.g., close family). • If a parent calls with a positive rapid strep from a takehome kit, confirm in the office with RADT before treating. • I D E (a) Signs and symptoms of streptococcal and viral pharyngitis. IDSA (b) Rapid antigen detection test (RADT) notes. (+) P NOTES PRESCRIBE antibiotics No penicillin allergy Penicillin allergy If the child can swallow pills: <60 lbs (<27 kg): •• Penicillin VK 250 mg orally twice daily for 10 days OR •• Benzathine penicillin 600,000 IU IM x 1 dose >60 lbs (>27 kg): •• Penicillin VK 500 mg orally twice daily for 10 days OR •• Benzathine penicillin 1,200,000 IU IM x 1 dose •• Cephalexin 20 mg/kg twice daily (MAX 1,000 mg daily) for 10 days OR •• Azithromycin 12 mg/kg once daily (MAX 500 mg daily) for 5 days OR •• Clindamycin 7 mg/kg 3 times daily (MAX 900 mg daily) for 10 days If the child cannot swallow pills: Amoxicillin suspension 50 mg/kg once daily for 10 days (MAX 1,000 mg daily) (c) Prescribing antibiotics before throat culture. There may be compelling situations that will lead to a 24- to 48-hour prescription of antibiotics until the results of the throat culture are available, but this is the exception. (d) Follow-up. • • If no improvement after 48 to 72 hours, reevaluate patient for possible complications (peritonsillar abscess, retropharyngeal abscess, etc.). (d) Follow-up cultures are unnecessary to assess cure. See back page for treatment of recurrent streptococcal pharyngitis. Intermountain measures the number of strep diagnoses, RADTs, and which antibiotics are prescribed. DIAGNOSIS AND MANAGEMENT OF ALGORITHM: ADULT DIAGNOSIS AND TREATMENT Streptococcal Pharyngitis – Adult ALGORITHM: ADULT DIAGNOSIS AND TREATMENT Signs and Symptoms of Streptococcal Pharyngitis (a) Recommend symptomatic relief to all patients. TEST: Obtain rapid strep test (b) (-) (+) A D U L T ASSESS risk of strep Risk score: Assign 1 point for each of the following: NEJM •• Fever >38°C •• Absence of cough •• Swollen, tender anterior cervical nodes •• Tonsillar swelling or exudate Other high-risk indicators: Contact or employment (-) risk (e.g., teachers family member with strep, etc.) IMPORTANT: Do not prescribe antibiotics for strep without a strep test. Low risk (score <4 AND no other high-risk indicator) High risk (score ≥4 OR high-risk indicator) TEST: Obtain throat culture NOTES (a) Signs and symptoms of streptococcal and viral pharyngitis. IDSA Streptococcal pharyngitis Viral pharyngitis •• Sudden onset of sore throat •• Fever •• Headache •• Nausea, vomiting, abdominal pain •• Tonsillopharyngeal inflammation •• Patchy tonsillopharyngeal exudates •• Palatal petechiae •• Tender nodes •• Winter and early spring presentation •• History of exposure to strep pharyngitis •• Scarlatiniform rash •• Conjunctivitis •• Coryza •• Cough •• Diarrhea •• Hoarseness •• Discrete ulcerative stomatitis •• Viral exanthema (b) Rapid antigen detection test (RADT). do not necessitate a back-up culture for adults unless risk score is high or the patient is at high risk due to contact or employment (e.g., teachers, family member with strep, etc.). • RADTs are highly specific and • Testing is not recommended for patients with overt viral features (see table above).IDSA (-) END. (+) throat culture is not necessary in the case of a negative RADT in low-risk patients because the low risk of acute rheumatic fever in adults with acute pharyngitis. IDSA • Do not test asymptomatic contacts (e.g., close family). PRESCRIBE antibiotics No penicillin allergy Penicillin allergy •• Penicillin V 250 mg orally 4 times daily or 500 mg 2 •• Clindamycin 300 mg 3 times daily for 10 days OR times daily for 10 days OR •• Amoxicillin 1,000 mg once daily or 500 mg twice daily for 10 days • In adults, a back-up •• Cephalexin 500 mg twice daily for 10 days OR • If a patient calls with a positive rapid strep from a take-home kit, confirm in the office with RADT before treating. (c) Follow-up cultures are unnecessary to assess cure. •• Azithromycin 500 mg once daily for 5 days If no improvement after 48 to 72 hours, reevaluate patient for possible complications (peritonsillar abscess, retropharyngeal abscess, etc.). (c) Intermountain measures the number of strep diagnoses, RADTs, and which antibiotics are prescribed. Pharyngeal Carriers Pharyngeal carriers are unlikely to spread streptococcal pharyngitis to close contacts, are at little or no risk of suppurative or nonsuppurative complications, and usually don’t require antibiotic treatment. For these reasons, routine treatment of strep carriers is not recommended. IDSA • Reasons for recurrent streptococcal pharyngitis can include: –– Chronic pharyngeal carriage masquerading as an acute strep infection due to a culture done during an intercurrent viral infection –– Noncompliance with prescribed antibiotic therapy –– A new streptococcal pharyngitis infection –– Recrudescence of infection with the original infecting strain (less common) • Information to help determine if the positive culture is from a carrier state or an active infection: Frequent recurrence (recurrent signs and symptoms within weeks or months of initial therapy with mostly viral symptoms); presenting signs and symptoms; season of the year; patient age. • Treatment: –– When antibiotics might be needed. Carriers do not ordinarily require antibiotic therapy. Situations in which antibiotic treatment may be indicated: –– –– –– –– Community outbreak of acute rheumatic fever, acute poststreptococcal glomerulonephritis, or invasive streptococcal pharyngitis Outbreak of streptococcal pharyngitis in a closed or partially closed community History of acute rheumatic fever (family or personal) Tonsillectomy being considered only because of carriage –– Criteria for tonsillectomy. ≥7 sore throat episodes in the past year OR ≥5 episodes in each of preceding 2 years OR years. AAO ≥3 episodes in each of preceding 3 –– Definition of episode: Sore throat plus 1 of the following: Temperature >38.3°C, cervical lymphadenopathy (tender lymph nodes or >2 cm), tonsillar exudate, positive culture for group A ß-hemolytic streptococcus –– Treatment: Antibiotics administered in conventional dosage for proved or suspected streptococcal episodes Antibiotics for Suspected Streptococcal Carrier IDSA No penicillin allergy Penicillin allergy •• Penicillin V 50 mg/kg daily in 4 doses (MAX 2,000 mg daily*) for 10 days PLUS rifampin 20 •• Clindamycin 20–30 mg/kg daily mg/kg daily in 1 dose (MAX 600 mg daily) for the last 4 days of treatment for 10 days •• Amoxicillin-clavulanic 40 mg/kg daily in 3 doses for 10 days (MAX 2,000 mg daily*) •• Benzathine penicillin G (intramuscular) 600,000 IU for <27 kg and 1,200,000 IU for ≥27 kg PLUS rifampin (oral) 20 mg/kg daily in 2 doses for 4 days (MAX 600 mg daily*) References AAO Baugh RF, Archer SM, Mitchell RB, et al; American Academy of Otolaryngology-Head and Neck Surgery Foundation. Clinical practice guideline: tonsillectomy in children. Otolaryngol Head Neck Surg. 2011;144(1 Suppl):S1-S30. IDSA Shulman ST, Bisno AL, Clegg HW, et al. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis. 2012;55(101):1279-1282. JAMA Barnett ML, Linder JA. Antibiotic prescribing to adults with sore throat in the United States, 1997-2010. JAMA Intern Med. 2013. doi: 10.1001/ jamainternmed.2013.11673 NEJM Wessels MR. Clinical practice. Streptococcal pharyngitis. N Engl J Med. 2011;364(7):648-655. Intermountain patient tools To order copies, go to i-printstore.com. • Colds and Coughs in Adults: Managing Viral Infections • Colds and Coughs in Children and Adolescents: Managing Viral Infections • Viral Infection Rx • Pediatric Dosing Guide: Acetaminophen and Ibuprofen Viral Infection Name: Date: You have been diagnosed with an infection caused by a virus. Most colds, coughs, and sore throats are caused by viruses. Fever is also a normal symptom of a viral infection. Antibiotics kill bacteria, not viruses, and they will not help you feel better faster. Follow this prescription to feel better. Diagnosis: Cold/cough Bronchitis Sore throat Other: General Instructions: Get plenty of rest Drink plenty of fluid Use a humidifier or saline nasal spray to relieve congestion Stay away from smoke Other: Medications: For pain: For cough: For other symptoms: Follow-up: If you don’t improve in ______ days, if you have new symptoms, or if you have other concerns, call or return to the office. If you received a SNAP (safety net antibiotic prescription), start taking it in ______ days if you don’t improve or ______ days if you get worse. (Don’t fill the prescription until you know you need it.) Other: Doctor’s signature: Date: *50280* Pt Inst 50280 © 2013 Intermountain Healthcare. All rights reserved. Patient and Provider Publications 801-442-2963 CLD002 - 10/13 Intermountain provider tools Available from the Primary Care Clinical Program page of intermountain.net and intermountainphysician.org: • Pediatric Strep Throat Flash Card • Adult Strep Throat Flash Card • Antibiotic Best Practices web page Antibiotic Stewardship Team in 3 doses (MAX 900 mg daily*) for 10 days *Prescribe MAX dose for adults. •Sylvie Backman, MD •Kim Brunisholz, MST •Whitney Buckel, PharmD •Wayne Cannon, MD •Jenna DenBleyker, MD •Missy Duke, PharmD •Per Gesteland, MD •Sharon Hamilton, MS, APRN •Jeremy Meier, MD •Jared Olson, PharmD •Ken Schaecher, MD •Douglas Smith, MD •Eddie Stenehjem, MD •Emily Thorell, MD •Anthony Wallin, MD •Matthew Walton, MD This CPM is based on best evidence at the time of publication. It is not meant to be a prescription for every patient. Clinical judgment based on each patient’s unique situation remains vital. ©2014 Intermountain Healthcare. All rights reserved. Patient and Provider Publications 801-442-2963 CPM067 - 01/14 Not intended to replace physician judgment with respect to individual variations and needs.