* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download STROKE: Defined - West Sound Advanced Practice Association
Survey
Document related concepts
Transcript
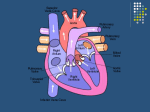
Filissa M Caserta MSN, ACNP-BC, CNRN The Johns Hopkins Hospital Neurosciences Critical Care Unit Baltimore Maryland STROKE: Defined Destruction of a portion of brain tissue as a result of circulatory failure in the distribution of a specific arterial vessel Epidemiology of Stroke • 5,500,000 stroke survivors are alive today • 700,000 each year – 500,000 of these are first attacks – 200,000 are recurrent attacks. • Every 45 seconds, someone in the US has a stroke • Every 3 minutes, someone in the US dies from a stroke • 30% to 50% of stroke survivors do not regain functional independence • 15% to 30% of all stroke survivors are permanently disabled • Public awareness about the signs of stroke should be improved, so that patients and their loved ones realize when a stroke is occurring Incidence of Stroke • • • • • • Increases with age 28% are less than 65 yrs old 80% of strokes are preventable 19% greater in men than women Women > 65 have higher incidence than men African Americans twice as likely to have a stroke than Caucasians Stroke: Classification Two Broad Categories ISCHEMIC HEMORRHAGIC • Too little blood • Too much blood • Intracerebral Hemorrhage • Thrombotic (ICH) • Embolic • Subarachnoid Hemorrhage (SAH) • Intraventricular Hemorrhage (IVH) STROKE TYPES •ISCHEMIC 84% •Thrombotic 53% •Embolic 31% •HEMORRHAGIC 16% •Intracerebral 10% •Subarachnoid 6% Circle of Willis Arteries that supply brain STROKE TREATMENT • Guidelines for Prevention of Stroke in Patients With Ischemic Stroke or Transient Ischemic Attack • Guidelines for the Early Management of Adults With Ischemic Stroke • Guidelines for the Management of Spontaneous Intracerebral Hemorrhage in Adults ISCHEMIC STROKE Risk Factors for Ischemic Stroke AHA/ASA Guidelines Primary Prevention of Ischemic Stroke A Guideline From the American Heart Association/American Stroke Association Stroke Council... Stroke. 2006;37:1583 Risk Factors for Stroke Not Modifiable • Sex • Age • Race/ethnicity • Low birth weight • Genetics Risk Factors for Stroke • Modifiable- well documented – – – – – – – – – – – – Hypertension Heart Disease [Afib] Carotid artery stenosis Sickle cell disease Postmenopausal hormone therapy Cholesterol level Diabetes Exposure to Cigarette Smoke Poor diet Physical Activity Obesity Body fat distribution • Modifiable- Less well documented – – – – – – – – – – – ETOH abuse Drug abuse BCP Sleep disordered breathing Migraines Hyperhomocysteinemia Elevated lipoprotein Elevated lipoprotein-associated lipase Hypercoagulability Inflammation Infection Ischemic Stroke: Types Thrombotic • Cause: Platelet Aggregation/Vessel Occlusion • Onset: During Sleep when BP is lowest • Risk Factors: – Large Vessel Disease • Atherosclerosis • Dissection • Arteritis – Small Vessel Disease • Chronic Hypertension • Lacunar : small subcortical infarcts Embolic • Cause: Fragments formed outside the brain break off and travel to a vessel in the brain • Onset: Abrupt, may occur during exercise • Risk Factors – – – – Afib Endocarditis Valve Disease Patent Foramen Ovale (PFO) Transient Ischemic Attack • A TIA is a rapidly reversible focal neurologic deficit that usually lasts for less than 30 minutes • Within 48 hours of the TIA there is an increased risk of stroke • A TIA workup should be given the same importance as a stroke workup • TIA is a warning sign; find the source, treat, and hopefully prevent a stroke Prevention of Recurrent Ischemic Event • Guidelines for Prevention of Stroke in Patients With Ischemic Stroke or Transient Ischemic Attack – A Statement for Healthcare Professionals From the American Heart Association/American Stroke Association Council on Stroke… Stroke. 2006;37:577 Prevention of Recurrent Ischemic Event • Includes all strategies listed in primary prevention document for BP, Smoking, Lipids, DM, weight etc.. • ETOH; eliminate/reduce • Medical and/or surgical intervention for: – Arterial dissection – Patent Foramen Ovale Prevention of Recurrent Ischemic Event • Medical management for the following: – – – – – – – – – – – – Vertebrobasilar disease Intracranial atherosclerosis Atrial fibrillation Acute MI and LV thrombus Cardiomegaly Valvular disease “Cryptogenic” Infarcts Lacunar Infarcts Hypercoagulable states Hyperhomocysteinemia Cerebral venous thrombosis Pregnancy Ischemic Penumbra • Definition: – the area surrounding the infarcted tissues that is potentially reversible – The main goal of stroke therapy is to preserve the ischemic penumbra!!! Management of Ischemic Stroke Guidelines for the Early Management of Adults With Ischemic Stroke A Guideline From the American Heart Association/ American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: The American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists (Stroke. 2007; 38:1655.) Classification of Recommendations Class I: • Conditions for which there is evidence for and/or general agreement that the procedure or treatment is useful and effective Class II: – Conditions for which there is conflicting evidence and/or a DO’s divergence of opinion about the usefulness/efficacy of a procedure or treatment • Class IIa The weight of evidence or opinion is in favor of the procedure or treatment. • Class IIb Usefulness/efficacy is less well established by evidence or opinion. D O – Conditions for which there is evidence and/or general agreement that the procedure or treatment is NOT useful/effective and in N Ts some cases may be HARMFUL Class III I. Pre-Hospital Management Class I • EMS • Assessment – Cincinnati Prehospital Stroke Scale – Los Angeles Prehospital Stroke Screen • Management EMS Management • • • • • • • • DO’s Manage ABCs Cardiac monitoring Intravenous access Oxygen (as required O2 saturation <92%) Assess for hypoglycemia NPO Alert receiving ED Rapid transport to closest appropriate facility capable of treating acute stroke DON’T’S • Dextrose-containing fluids in nonhypoglycemic patients • Hypotension/excessive blood pressure reduction • Excessive intravenous fluids II. Designation of A Stroke Center Class I • Brain Attack Coalition recommended that stroke centers be established • Goal: to improve the organization and delivery of care to stroke patients • Certification through JCAHO began in 2004 – Standard measures for stroke (see end) – Primary Stroke Center (PSC) • Comprehensive Stroke Center (CPS) II. Designation of A Stroke Center PSC CSC • Have personnel, • All for PSC PLUS programs, expertise and – Treat complicated strokes including ICH/IVH / SAH infrastructure to care for – Have endovascular uncomplicated strokes capabilities • Use many acute therapies – Have ICUs to manage the • Admit patient to a stroke complicated stroke patients unit • JCAHO & ASA are creating a formal process for certification III. Emergency Evaluation and Diagnosis of Acute Ischemic Stroke (AIS) Class I • Organized protocol for emergency evaluation and treatment plan within 60 minutes • Acute stroke team to include MD/RN/ Lab/Radiology • Use of stroke rating scale (preferably NIHSS—see end) • Lab tests • Imaging III. Emergency Evaluation and Diagnosis of Acute Ischemic Stroke (AIS) All Patients Selected patients • Noncontrast brain CT or brain MRI (should not delay tx) • Blood glucose • Serum electrolytes/renal function tests • ECG • Markers of cardiac ischemia • CBC • Coags • Oxygen saturation • • • • • • Hepatic function tests Toxicology screen Blood alcohol level Pregnancy test ABG (if hypoxia is suspected) Chest radiography (if lung disease is suspected) • Lumbar puncture (if subarachnoid hemorrhage is suspected and CT scan is negative for blood) • Electroencephalogram (if seizures are suspected) IV. Early Diagnosis: Brain and Vascular Imaging Class I • Imaging recommended prior to therapy: CT provides the info you need • Multi-modal CT and MRI can be helpful but should not delay treatment Class II • For intra-arterial rtPA, surgery and endovascular procedures, need vascular imaging Ischemic stroke on HCT V. General Supportive Care and Treatment of Acute Complications Class I • ABCs • Normothermia • CV Monitoring and Treatment • BP control –HTN • BP control– Hypotension – Avoid it – Find and tx cause • Glycemic control V. General Supportive Care and Treatment of Acute Complications • HTN Management – Controversial because data is ambiguous, however, it is true that rapidly lowering BP does cause harm. – Not eligible for tPA • SBP< 220mmHg /or DBP < 120mmHg non-tPA – Eligible for tPA • Pre Rx: SBP <185 or DBP <110 • Post Rx: SBP < 180 or DBP <105 VI. Intravenous Thrombolytics Class I • IV tPA is the only FDA approved medical therapy for patients with AIS • Other thrombolytics are NOT recommended outside of clinical trials VI. Intravenous Thrombolytics Intravenous rtPA (0.9 mg/kg, maximum dose 90 mg) is strongly recommended for carefully selected patients who can be treated within 3 hours of onset of ischemic stroke Agent • Tissue Plasminogen Activator [t-PA] Timeframe: • 3 hours for IntraVenous Goals: • Open the occluded vessel • Re-establish blood flow • Limit injury/Improve Outcome VII. Intra-arterial tPA Class I • < 6 hours for selected patients who are NOT eligible for IV tPA. • Must be at an experienced stroke center with immediate access to angio and interventionalists Class II • IA tPA is reasonable for pts who have contraindications to IV tPA (recent surgery, age, time frame) • Class III • Availability of IA tPA should NOT preclude IV tPA in eligible patients VIII. Anticoagulants Class III • VIII. Anticoagulation – Urgent anticoagulation is NOT recommended for treatment of AIS – Should not be used in lieu of IV thrombolysis in eligible patients – Can cause hemorrhagic transformation IX. Antiplatelets Class I • Aspirin : initial dose 325 mg • Given within 24- 48 hours of stroke onset Class III • Aspirin should NOT be used as a substitute for other acute interventions, especially intravenous administration of rtPA • ASA as an adjunctive therapy within 24 hours of rtPA is NOT recommended • Clopidogrel alone or in conjunction with ASA is NOT recommended for AIS X. Volume expansion/Vasodilators and Induced Hypertension Class I • Induced HTN: In “exceptional” cases, an MD may prescribe vasopressors to improve cerebral blood flow • Need close CV and neuro monitoring Class III • No hemodilution • No vasodilators (methylxanthine derivatives) XI. Surgical Intervention • Immediate intervention – Carotid Endarterectomy (CEA) – Extracranial-intracranial arterial bypass (EC-IC bypass) • Insufficient data exists to make a recommendation XII. Endovascular Intervention Class II • MERCI retrieval device is reasonable in carefully selected patients although the utility of the device in improving outcomes is unclear • Other mechanical endovascular treatments should be used in the setting of clinical trials. XII. Endovascular Intervention • Mechanical removal of clot – Clinical trials have shown that thrombectomy with mechanical thrombolysis devices is indeed feasible in the treatment of acute stroke. – Many devices have been discontinued – MERCI Retriever has received FDA clearance. XIII. Combination Reperfusion Therapies in AIS Class III • Combo interventions to restore perfusion are NOT recommended outside of clinical trials **Combo =Using thromolysis combined with antiplatlets/neuroprotection XIV. Neuroprotective Agents Class III • No neuroprotection agents can be recommended ** Neuroprotective agents= nimodipine, NMDA, magnesium and others XV. Admission to Hospital & General Acute Treatment after Hospitalization Class I • • • • • • Use of comprehensive, specialized stroke care Use of standardized stroke ordersets Early mobilization Swallow eval BEFORE eat/drink Treat UTI/pneumo with abx DVT prophylaxis with SQ anticoagulation ( as well as early mobilization and external compression devices) • Treatment of concomitant medical disease • Early intervention to prevent recurrent stroke XV. Admission to Hospital & General Acute Treatment after Hospitalization Class II • If cannot swallow, provide NG/OG/PEG nutrition • ASA is potential intervention for DVT prophylaxis, but less effective than anticoagulation. • If cannot receive anticoagulation for DVT, use external compression devices Class III • No nutritional supplements are needed for patients who can swallow • If possible, avoid using a foley due to high rosk of UTI XVI. Treatment of Acute Neurological Complications Class I • Treat increased ICP as using standard interventions to decrease ICP • For risk of malignant cerebral edema, transfer to medical center with neurosurgical expertise • EVD if hydro • Decompressive surgical evacuation of spaceoccupying cerebellar infarctions • Treat recurrent seizures XVI. Treatment of Acute Neurological Complications Class II • Although measure to decrease ICP are used, they are unproven with AIS • Decompressive Surgery for cerebral hemisphere infarct – Can be a life-saving measure – Age, side of infarct – Surgery may be recommended for seriously affected patients – If surgery is recommended, in-depth discussion with families re: potential outcomes/disability should occur. XVI. Treatment of Acute Neurological Complications Class III • NO steroids • NO prophylactic anticonvulsants Palliative Care • Ensure dialogue is occurring re: patient wishes • Advanced directives • Withdrawal of Life Support Other Diagnostic Work-Up • Additional work up • LABS: TSH, RPR, Homocysteine, cholesterol, LDL, HDL, triglycerides – TESTS • Transthoracic Echo • Carotid Dopplers HEMORRHAGIC STROKE Hemorrhagic Strokes: Types • SAH (Subarachnoid Hemorrhage) – Ruptured Aneurysm • ICH (Intracerebral Hemorrhage) – Hypertension – Cocaine – Many other • IVH (Intraventricular Hemorrhage) – Usually an extension of ICH – Rarely isolated Risk Factors for Hemorrhagic Stroke Modifiable • HTN!!! • IVDA- cocaine/amphetamines • Chronic hypertension ICH CAUSES • Coagulopathy – Thrombocytopenia • Neoplasm – Malignant primary CNS – Metastatic CNS tumor – Hepatic failure • Postendarterectomy reperfusion – Factor deficiency • Sinus thrombosis/venous – Anticoagulant therapy • Trauma – Thrombolytic therapy • Vascular anomalies • Drugs – Cocaine – Sympathomimetics • Hemorrhagic transformation of cerebral infarct • Infection – Aneurysms/ Arteriovenous malformations – Vasculitis/Vasculopathy – Amyloid angiopathy – Moyamoya disease Intracerbral Hemorrhages Location A) Intracerebral hemorrhages most commonly involve cerebral lobes, originating from penetrating cortical branches of the anterior, middle, or posterior cerebral arteries B) Basal ganglia, originating from ascending lenticulostriate branches of the middle cerebral artery C) Thalamus, originating from ascending thalmogeniculate branches of the posterior cerebral artery D) Pons, originating from paramedian branches of the basilar artery E) Cerebellum, originating from penetrating branches of the posterior inferior, anterior inferior, or superior cerebellar arteries Spontaneous Intracerebral Hemorrhage Adnan I. Qureshi, M.D., Stanley Tuhrim, M.D., Joseph P. Broderick, M.D., H. Hunt Batjer, M.D Hidek Hondo, M.D., and Daniel F. Hanley, M.D. NEJM.Volume 344:1450-1460 May 10, 2001 Number 19 ICH Management Guidelines for the Management of Spontaneous Intracerebral Hemorrhage in Adults 2007 Update: A Guideline From the American Heart Stroke Association Stroke Council, High Blood Pressure Research Council, and the Quality of Care and Outcomes in Research Interdisciplinary Working Group: The American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists (Stroke. 2007; 38:2001.) Emergency Diagnosis and Assessment of ICH Class I • ICH is a medical emergency, with frequent early, ongoing bleeding and progressive deterioration, severe clinical deficits, and subsequent high mortality and morbidity rates, and it should be promptly recognized and diagnosed • CT and magnetic resonance are each first-choice initial imaging options; in patients with contraindications to magnetic resonance, CT should be obtained • ***Angiography- if high suspicion of vascular anomaly ICH IVH Treatment of Acute ICH/IVH Class I • Monitor in an ICU • Antiepileptic drugs (AEDs) to treat seizures • Treat and decrease fever • Early mobilization and rehab Treatment of Acute ICH/IVH Class II • ICP-manage using a variety of medical therapies as well as EVD if hydro; CPP goal > 70 mmHg • Glycemic control (treat > 140mg/dL) • BP control: SBP < 180 and MAP < 130; CPP 6080 • Factor rFVIIa • “Brief” period of prophylactic AEDs soon after ICH may decrease risk of seizures especially in lobar hemorrhage Treatment of Acute ICH/IVH • If SBP is >200 mm Hg or MAP is >150 mm Hg, then consider aggressive reduction of blood pressure with continuous IV meds monitor BP q 5 minutes. • If SBP is >180 mm Hg or MAP is >130 mm Hg and there is suspicion of increased ICP, reducing blood pressure using intermittent or continuous IV meds to keep CPP perfusion pressure >60 to 80 mm Hg • If SBP is >180 mm Hg or MAP is >130 mm Hg and no suspicion of elevated ICP, then consider a modest reduction of blood pressure (eg, MAP of 110 mm Hg or target blood pressure of 160/90 mm Hg) using intermittent or continuous intravenous medications to control blood pressure, and clinically reexamine the patient every 15 minutes. Treatment of Acute ICH/IVH Class II • rFVIIa • Treatment with rFVIIa within the first 3 to 4 hours after onset to slow progression of bleeding has shown promise in one moderate-sized phase II trial • However, the efficacy and safety of this treatment must be confirmed in phase III trials before its use in patients with ICH can be recommended outside of a clinical trial Prevention of DVT and PE Class I • Hemiparesis/hemiplegia ---should have intermittent pneumatic compression Class II • Prophylaxis: – after 3-4 days – once documented bleeding has stopped – low-dose subcutaneous low-molecular-weight heparin or unfractionated heparin • Treatment – Placement of a vena cava filter – Long-term antithrombotic therapy after placement of a vena cava filter must look at risk of rebleed vs risk of thrombus ICH Related to Fibrinolysis Carries a poorer prognosis because bleeds tend to be huge Class I • Heparin---Protamine sulfate (dose depends on time heparin stopped) • Coumadin– Vitamin K IV (10mg) with treatment to replace clotting factors Class II • Replace clotting factors – Prothrombin complex concentrate, factor IX complex concentrate, and rFVIIa; quick and less volume – FFP; large volumes and longer infusion time ICH Related to Fibrinolysis When to restart anticoagulation after ICH?? Class II • Consider: – Risk of subsequent arterial or venous thromboembolism – Risk of recurrent ICH – Overall state of the patient • If low risk of thromboembolic event, may restart antiplatelet instead of warfarin • If warfarin must be restarted, wait 7-10 days after ICH Surgery • Surgical Approaches • Timing of Surgery • Decompressive Craniectomy • International Surgical Trial in Intracerebral Hemorrhage (STICH) • New NIH study: Minimally Invasive Stereotactic Surgery + rtPa for ICH Evacuation (MISTIE) Surgical Approaches Class I • Cerebellar ICH > 3cm with neuro deterioration /herniation or hydro should have removal of hemorrhage Class II • Lobar clots within 1 cm of the surface may be considered for standard craniotomy • Stereotactic infusion of urokinase into clot – decreases size of clot and risk of death BUT it’s usefulness is UNKNOWN • Minimally invasive clot evacuation via mechanical devices – needs further testing therefore it’s usefulness is UNKNOWN Class III • Evacuation of supratentorial ICH by standard craniotomy within 96 hours is NOT RECOMMENDED except as noted above Decompressive Craniectomy Class II • Too few data currently exist to comment on the potential of decompressive craniectomy to improve outcome in ICH Withdrawal of Life Support • We recommend careful consideration of aggressive full care during the first 24 hours after ICH onset and postponement of NEW DNR orders during that time. • In all cases, physicians and nurses caring for ICH patients who are given DNR status should be reminded that the designation relates only to the circumstance of cardiopulmonary arrest and that patients should receive all other appropriate medical and surgical interventions. Prevention of Recurrent ICH Class I • Treating hypertension in the nonacute setting is the most important step to reduce the risk of ICH and probably recurrent ICH as well • Smoking, heavy alcohol use, and cocaine use are risk factors for ICH, and discontinuation should be recommended for prevention of ICH recurrence • 72 yo white male • PMHx: Case Study – Mild HTN • Meds – Lisinopril 10mg qday • Family Hx – Mom- s/p cva – Dad- s/p cva x 2 • Social – MS in Civil Engineering – Working as tunnel expert FHWA Case Study • • • • • Home alone “Didn’t feel well” Sudden onset right sided weakness Called 911—could he talk?? EMS Arrives---house locked—tic-toc tPA minutes!! • Establish TOSO?? Case Study • Since could not establish TOSO, no thrombolytics • Cause? – Undiagnosed afib with SLOW ventricular response • Rx – Pacemaker – Heparin--- Coumadin – Acute rehab after 72 hours! • Rehab – Acute 30 days – Day Hospital 2 months - Subacute 3 months - Outpatient PRE STROKE HAWAII 1996 POST STROKE HAWAII 2005 THERE IS LIFE AFTER STROKE!! Cincinnati Prehospital Stroke Scale Last time seen normal ________________ Evaluate for Facial Droop Present? Absent? Hold up arms and look for Drift Present? Absent? Repeat “The sky is blue in Cincinnati. Abnormal? Normal? BP__________ Blood sugar___________ History of anticoagulant medications ? Warfarin_____ Heparin ________ Patients with 1 of these 3 findings -as a new event - have a 66% probability of an ischemic stroke. If all 3 findings are present the probability of an acute stroke is more than 88% Los Angeles Prehospital Stroke Screen • Last time patient known to be symptom free • Screening – – – – – Age >45 y No history of seizures or epilepsy Symptoms present <24 h Not previously bedridden or wheelchair bound If unknown or yes • Blood glucose 60 to 400 mg/dL Yes No Examination • Exam – Facial smile grimace – Grip – Arm strength (drift) • Based on examination, patient has unilateral weakness Yes No • If items are yes or unknown, meets criteria for stroke NIHSS • National Institutes of Health Stroke Scale (NIHSS) – The initial NIHSS score provides important prognostic information. – Approximately 60% to 70% of patients with an acute ischemic stroke and a baseline NIHSS score <10 will have a favorable outcome after 1 year as compared with only 4% to 16% of those with a score >20. – The NIHSS score can also help identify those patients at greatest risk for ICH associated with thrombolytic treatment. Designation of A Stroke Center JCAHO Standard Measures • tPA considered • Screen for dysphagia • Deep vein thrombosis prophylaxis • Lipid profile during hospitalization • Smoking cessation • Education about stroke • Plan for rehabilitation considered • Antithrombotic medications started within 48 hours • Antithrombotic medications prescribed at discharge • Anticoagulants prescribed to patients with a-fib