* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download increased or high medial arch of the foot
Survey
Document related concepts
Transcript
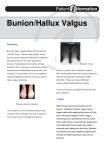
AFTER MID SURGERY DR.Mahmood khdier Orthopaedic Foot and ankle deformity 2 Dr.Mahmood khdier LECTURE 6 Pes cavus (increased or high medial arch of the foot): The medial arch is higher than normal with varus foot and finger clawing the main Causes are: Primary idiopathic, usually familial and bilateral. Neuromuscular conditions like cerebral palsy, peroneal muscle dystrophy or friedreich’s ataxia This deformity of the foot with the clawing of the toes puts the body weight on the metatarsal heads that projects down into the sole of the foot and usually there is an overlying skin callosities due to friction with the shoe. In the mobile flexible early deformity the foot shape can be restored if the metatarsal heads pushed up by the examiner’s finger, as the arch gets normal and the clawing of the toes corrected. Later the deformity if untreated gets fixed and painful. Treatment: In cases of painless mobile deformity no treatment is needed apart from special shoe wear. In severe deformities which is still mobile the foot shape can be improved and weight bearing on metatarsal heads can be decreased by rebalancing surgery correcting the clawing by tendon transfer so the long toe flexors are released and transferred from the planter to the dorsal aspect of the toes and fixed on the extensor expansion so it will correct the hyperextension and put the toes straight. For fixed deformities no much can be done, if special shoe wear is not enough complex bone surgeries and arthrodesis can be done, operations must always delayed after the age of 16 years. Hallux valgus: It’s the commonest foot and musculoskletal deformity seen in practice. There is valgus deviation of the big toe with mild medial rotation where the nail facing slightly to the medial side, there is also overcrowding of the other toes with the 2nd. Toe usually develops the deformity known as hammer toe (extension of the metatarsophalangial joint, flexion of the proximal interphalangial and extension of the distal interphalangial joint). Predisposing factors: The shoe wears: In people who do not wear shoes the forefoot is fan-shaped (splaying) with the big toe in line with the lst. Metatarsal bone (i.e. varus position which is rather normal). While in those who uses the shoes the hallux get deviated laterally at the metatarsophalangial joint especially in females who wear high shoes that are narrow anteriorly. Metatarsus primus varus: there is forefoot splaying with excessive primary varus position of the 1st. metatarsal bone that predispose for lateral deviation of the big toe during shoe wear. Tight and prolonged shoe wear by itself play part in predisposition to the same deformity Inter metatarsal angle less than 9 degree &metatarsophal angel angle less than 15 degree Soft tissue changes that act to maintain and gradually worsen the deformity such as: The adductor hallucis get tight on the lateral side of the hallux. There is lateral capsular contracture and shortening. Lax redundant capsule medially. The long extensors of the hallux gradually subluxate laterally and act to maintain and worsen the deformity by its bow-string effect. Secondary changes occurs usually like: To start with the deformity is mild, with time it get more severe, immobile and cannot be corrected manually, later osteoarthritis occurs with stiff and painful first metatarsophalangial joint. The lst. metatarsal head looks thick and widened, and because of rubbing with shoe wear on its medial side there will be the formation of thick bony exostosis and over it there is a protective synovial bursa (the bunion) that may get swollen, inflamed or infected. Both of the above changes can be a cause of pain. Causes of hallux valgus: Commonest type is the primary idiopathic one that mostly affects older females (above 40) and usually bilateral. It can occur secondary to muscle imbalance in neuromuscular disorders or in older people. It’s very common in cases of rheumatoid arthritis. An uncommon type is the congenital type that affect young adolescent girls due to congenital metatarsus primus varus, this type usually present early because the mother is anxious and afraid that here daughter may get the severer deformity later in life like herself. Clinical features: There is obvious deformity with exostosis and bunion, in the beginning it’s mild and can be corrected manually, later it gets more severe, less mobile and osteoarthritis may develop. The bunion may get swollen infected or inflamed. Pain at the 1st. metatarsophalangial joint may due to: Inflamed or infected bunion. Hammer toe. Secondary osteoarthritis. Painful metatarsal heads on the planter aspect of the foot (painful metatarsalgia) due to forefoot splaying and downward projection of metatarsal heads and abnormality in weight bearing. X-ray: Taken with the patient standing to show the degree of metatarsal and hallux angulations. Also it shows the state of the joint being normal, arthritic or subluxated. Treatment: 1. Adolescent congenital deformity always need surgical correction of the varus position of the 1 st. metatarsal by osteotomy to put it more straight so the big toe will assume more straight position. 2. For adults: a. If the deformity is mild and mobile in a patient below 40 years most of the cases respond well for special attention for footwear, which should be wide anteriorly and soft with special padding for the bunion, hammer toe and metatarsal heads. b. If this is not enough we may use surgical soft tissue procedure where we release the adductor hallucis laterally and do lateral capsulotomy, on the medial side, we excise the bunion and remove the exostosis and tighten the capsule. Postoperatively we may use special pad between the 1st. and 2nd. toes to prevent recurrence. c. For those above 40 years with failure of the previous methods we add to the surgery above an osteotomy of the 1st. metatarsal to correct its alignment. There are different types of osteotomies as Basal osteotomy, Mitchell’s osteotomy and Willson’s osteotomy. d. For elderly or osteoarthritic joint we do excisional arthroplasty by excising the proximal part of the proximal phalanx (Keller’s operation), this will relieve pain and improve shape and movement. Hallux rigidus This is a case of painful rigid stiff 1st. metatarsophalangial joint due to osteoarthritis secondary to one of the followings: Trauma. Ostoechondritis dissicans of the lst. metatarsal head. Gout or pseudogout. The deformity is most common in males in contrast to hallux valgus. Clinically: Patient have painful tender joint that is stiff on examination and disturb the normal walking of the patient because of the lack of hallux extension. The joint is thick and tender with limitation of movement specially extension. In normal walking, the big toe dorsiflexes (extends) considerably. With rigidusThe usual cause is OA of the first MTP joint Rheumatoid arthritis of the ankle and foot: The foot is affected as common as the hand and the disease pass in its three stages, 1st. stage of synovitis that affects ankle, intertarsal and other small joints, also affects synovial tendon sheath of different tendons mainly the tibialis posterior and the peronei. 2nd.stage of erosion of the articular cartilage and tendons that can be torn. 3rd. stage of severe deformity and dysfunction with the characteristic deformities of foot valgus, forefoot splaying, hallux valgus and toe clawing. There will be lot of planter callosities and dorsal corns that may get inflamed or infected and sometimes ulcerate. Clinically: Patient having progressive pain and discomfort with difficulties in shoe wear and walking. There is limitation of movements and gradual development of deformities, callosities and corns. X-ray: May show the joint erosions and foot deformities. Treatment: Special care for shoe wear, rest, and limitation of weight bearing sometimes by special weight relieving calipers. Drug treatment according to the stage of the disease like NSAID, painkillers, disease modifying drugs.. .etc. Local steroid injection of joints or around tendon sheaths whenever indicated. Synovectomy of joints or tendon sheaths. For seriously deformed foot replacement arthroplasty or joint arthrodesis. Ruptured tendo Achillis Probably rupture occurs only if the tendon is degenerated. Consequently most patients are over 40. While pushing off (running or jumping), the calf muscle contracts; but the contraction is resisted by body weight and the tendon ruptures. The patient feels as if he has been struck just above the heel, and he is unable to tiptoe. Soon after the tear occurs, a gap can he seen and felt 5 cm above the insertion of the tendon. Plantar flexion of the foot is weak and is not accompanied by tautening of the tendon. Where doubt exists, Simmonds’ test is helpful: with the patient prone and foot free out of bed, the calf is squeezed; if the tendon is intact, the foot is seen to go into planti-flexion; if the tendon is ruptured the foot is still without any movement. Treatment: If the patient is seen early, the ends of the tendon may be approximate when the foot is passively plantiflexed. If so, plaster is applied with the foot in equinus and is worn for 8 weeks. A shoe with a raised heel is worn for a further 6 weeks. Operative repair is probably safer, but an equinus plaster for 8 weeks and a heel raise for a further 6 weeks are still needed. The diabetic foot Foot disorders are common in diabetes and result from: Peripheral vascular disease causing claudication, trophic changes, ulceration and even gangrene. Neuropathy with sensory and/or motor impairment causing various foot deformities and possibly charcot joints. Osteoporosis, which may be severe enough to lead to fractures. Infection, which is an ever-present danger in diabetes. Treatment The principles of treatment are: Proper control of the diabetes. Constant and careful attention to the skin and toenails to prevent infection. Dry gangrene of the toe can be left to demarcate before amputation; wet gangrene and infection may call for immediate amputation. Charcot joints causing instability may need splintage. Osteoporotic fractures should be immobilized only until pain subsides. Gout arthritis: Swelling, redness, heat and exquisite tenderness of the metatarsophalangial joint of the big toe (‘podagra’) is characteristic of gout. The condition may closely resemble septic arthritis, but the systemic features of infection are absent. The serum uric acid level may be raised. Treatment with anti-inflammatory drugs will abort the attack; until the pain subsides the foot should be rested and protected from injury. Done by : Murtedha Abbas Good luck