* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download A Unique Delivery Vehicle for Topically Applied Formulations
Survey
Document related concepts
Transcript
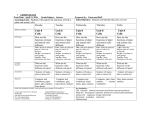
Chapter 9 Foam: A Unique Delivery Vehicle for Topically Applied Formulations Dov Tamarkin, PhD Foamix Ltd. C Key Words: PY O Foam, Hydrophilic Emulsion Foam, Lipophilic Emulsion Foam, Nanoemulsion Foam, Aqueous Foam, Hydroethanolic Foam, Potent-Solvent Foam, Suspension Foam, Ointment Foam, Hydrophilic Ointment Foam, Oil Foam, Saccharide Foam H IG R Introduction T The paramount objective of pharmaceutical and skin care product development is to create effective products based on state-of-the-art active ingredients with improved patient compliance and usability. The vehicle used to deliver topical active ingredients can considerably influence the performance of the active ingredients. The vehicle can have a direct effect on the condition of the skin as a barrier, as it can enhance or retard the delivery of the active agent to the target site of action. In addition it can affect the skin’s physical appearance and sensory properties, attributes that can influence patient compliance. While semi-solid compositions, such as creams, lotions, gels, and ointments are commonly used by consumers, new forms are desirable, in order to achieve improved control of the application, increased skin absorption, and to maintain or bestow the skin promised beneficial properties. Foam is becoming a prominent delivery system for topical active agents in skin treatment. This platform provides an innovative, easy to apply, modern alternative to creams and ointments. A significant advantage of the foam formulation is that it spreads easily on large skin areas, does not leave a greasy or oily film on the skin after application and does not impart a greasy feeling upon and after application. The use of foam in dermatology was first reported in 1977 by Woodward and Berry who studied the therapeutic benefit of Betamethasone benzoate, in hydroalcoholic “quick-break” foam in comparison with a corresponding semisolid dosage form.1 The activity of the foam, as determined by a vasoconstriction ED 233 Source: Tamarkin D. Foam: A Unique Delivery Vehicle for Topically Applied Formulations, in Formulating Topical Applications - a Practical Guide, Dayan N, Ed., Carol Stream, IL: CT Books, Chapter 9 (2013), pp. 233-260. AT_Ch9.indd 233 11/14/13 1:07 PM Foam: A Unique Delivery Vehicle for Topically Applied Formulations test, was similar to the corresponding ointment and better than a cream. In 1995, Deaffontio et al. investigated the anti-inflammatory and analgesic profile of a topical foam formulation of ketoprofen lysine salt, which exhibited anti-inflammatory and analgesic effectiveness and favorable usability properties.2,3 A comprehensive review on foam drug delivery in dermatology was written by Carryn et al. in 2003.4 Tamarkin et al. published a broad review, titled “Emollient foam in topical drug delivery,” in 2006;5 and an additional review, titled “Foam: The Future of Effective Cosmeceuticals,” was published in Cosmetics & Toiletries magazine in 2006.6 More recently, in 2010, Steckel et al. wrote a review on foam technology, titled ”Foams for pharmaceutical and cosmetic application.”7 Overview of the Market: Current Foam Technologies PY O C Currently, only a few dermatological foam products are commercially available. EpiFoam (Alaven Pharmaceutical LLC), which contains hydrocortisone acetate 1% and pramoxine hydrochloride 1%, is based on an aqueous foam vehicle. It is indicated for the relief of the inflammatory and pruritic manifestations of corticosteroid-responsive dermatoses.8 Olux Foam and Luxiq Foam (Stiefel, a Glaxo SmithKline (GSK) company), which contain 0.05% clobetasol propionate and 0.12% betamethasone valerate, respectively, are both thermolabile (temperature-sensitive) steroid hydroethanolic foams (containing about 60% ethanol).9,10 Evoclin (Stiefel) is another hydroethanolic foam, comprising 1% clindamycin, which is indicated for acne.11-12 Stiefel, a GSK company further markets four emollient foams, namely Olux-E (0.05% clobetasol propionate) Foam and Verdeso (0.05% desonide) Foam for corticosteroid-responsive dermatoses, Sorilux (0.005% calcipotriene) Foam for psoriasis, and Fabior (0.1% tazarotene) foam for acne.13-14 Scytera (Promius Pharma, developed by Foamix), is a non-prescription foam containing 2% coal tar for the treatment of psoriasis, which is effective and highly convenient.15 While coal tar preparations in general are associated with poor patient compliance as they cause skin irritation, staining to clothes, hair and skin, and are malodorous,16 Scytera’s color intensity is off-white, and thus does not cause staining; moreover, its fragrance is pleasant. Stiefel and Foamix are both market leaders in foam technology and are engaged in the development of innovative foams in collaboration with several pharmaceutical companies. This chapter will describe what foam is, survey the various types of foam available today commercially along with those presently under development, and exemplify their uses in skin therapy. It will further account for the physiochemical properties of foam products and explain how to evaluate them. Please note that the term “drug” is used extensively throughout this chapter, as the source of much discussion is based on such research; however, the principles of foam delivery systems apply equally well to personal care product types and so for the purposes of this writing, the terms, as regards their methods of application, may be considered synonymous. T H IG R ED 234 AT_Ch9.indd 234 11/14/13 1:07 PM Chapter 9 The Rosetta Stone of Foam PY O C To date, all foams are collectively designated as “Medicated Foams” by the European Pharmacopoeia, and the U.S. Pharmacopoeia simply lists “Foam Aerosol” as a sub-part of its Aerosol section.17 Most foams used in pharmacological and cosmetic applications are aerosol foams, which comprise a semi-solid formulation, packaged in an aerosol can and pressurized by a propellant. It is imperative to understand that while a foam preparation exhibits distinct characteristics that differentiate it from other generically used vehicles, not all foams are similar and they can be tailored to fulfill product properties requirements. While in the past there were just a few types of medicated foam, i.e., aqueous foams, hydroethanolic foams and emulsion-based emollient foams, today there are several new classes of foam formulations under development, mainly by Foamix, which are distinct in their composition and functionality from each other. Examples of new classes of foams are petrolatum-based foam, which is the foam version of an ointment; hydrophilic solvents (such as PEG and propylene glycol) based foam, which is the foam version of a hydrophilic ointment; and oil-based foam, which corresponds to oil solutions or suspensions. Foams that are based on “potent” solvents, such as dimethyl isosorbide and dimethyl sulfoxide (DMSO) contribute to high solubility and enhanced transdermal drug delivery of active agents. Also under development are hydroethanolic foams (containing high levels of ethanol) which are suitable mostly for scalp treatment because they collapse easily and do not impart greasiness to the scalp and hair. Foams can be also used to further stabilize suspensions and there are foams that contain high levels of saccharides and honey for wound and burn therapy. These versatile foam classes have been used to develop a large number of foam products, containing a variety of active ingredients, such as antibiotic agents, antifungals, antiviral agents, immunomodulators, corticosteroids, steroid hormones, anti-acne agents, anti-psoriasis agents, vitamins A, B, C, D and E, a-hydroxy and b-hydroxy acids, and skin barrier-building agents for the treatment dry skin conditions. It is important for the formulation scientist to understand the differences between the above classes of foam formulations, and be able to select the right type of formulation for a given clinical condition. The current review presents the “Rosetta Stone” of foam. It introduces the various types of foam technology platforms and suggests a functional transformation of their respective traditional topical dosage forms. Table 1 lays out a series of foam classes, which correspond to their current topical dosage forms, with a summary of the main features and attributes of each class of foam; and the following sections will provide further features of each of these classes. T H IG R ED 235 AT_Ch9.indd 235 11/14/13 1:07 PM Foam: A Unique Delivery Vehicle for Topically Applied Formulations Table 1. Classification of foam technology platforms, corresponding to traditional topical dosage form designations Foam Class Traditional topical dosage Main form designation formulation (USP and EP, characteristics combined) Attributes Water-containing Foams Emollient, skin conditioning Emulsion, Cream, vehicle Hydrophilic cream Can carry lipophilic and hydrophilic drugs and retain their stability Emulsion, Cream, Lipophilic cream Favorable usability, enhance compliance Oil-in-water Hydrophilic Emulsion Foam emulsion Lipophilic Water-in-oil Emulsion Foam emulsion Emollient, skin conditioning vehicle PY O C Non-greasy T ED Main Hydroethanolic ingredients = Foam ethanol and water Gel H Aqueous Foam Main ingredients = water, gelling agents and surfactants Improved solubility and skin delivery of active agents IG Oil-in-water nanoemulsion R Nanoemulsion Foam Serves to solubilize drugs, thereby increasing their Solution, Tincture bioavailability Suitable for oily skin areas Does not require preservatives Serves to solubilize drugs, thereby increasing their bioavailability Potent-Solvent Foam Water and strong solvents Gel, solution Induces skin penetration Suitable for transdermal drug delivery Does not require preservatives Suspension Foam Suspended drug in a foam formulation Topical suspension Emollient, skin conditioning vehicle Can carry suspended drugs and retain their stability Favorable usability 236 AT_Ch9.indd 236 11/14/13 1:07 PM Chapter 9 Foam Main formulation characteristics Class Traditional topical dosage form designation (USP and EP, combined) Attributes Water-free Foams Ointment Foam Single phase, petrolatum main ingredient (up to 90%) Ointment, White ointment, Hydrophobic ointment Prolongs drug skin residence Compatible with watersensitive drugs Does not require preservatives Greaseless ointment base PY O C Single phase, PEG, propylene glycol, glycerin or other hydrophilic solvents main ingredients Polyethylene glycol ointment, Hydrophilic ointment T H IG R Hydrophilic Ointment Foam Occlusive, builds up skin barrier Humectant, provides skin moisturization Serves to solubilize drugs, thus rendering them more bioavailable Compatible with watersensitive drugs ED Does not require preservatives Builds up skin barrier Oil Foam Single phase, liquid oil main ingredient Nourishes and lubricates the skin Oil solution or suspension Prolongs drug skin residence Compatible with watersensitive drugs Does not require preservatives Saccharide Foam Monosaccharides, disaccharides, honey main ingredients (up to 90%) Hygroscopic, absorbs exudates Antibacterial Useful for wounds and burns treatment Water-containing Foams The early generation of medicated foams included the aqueous foam, the hydroethanolic foam and the newer platform of emulsion-based foam, also termed 237 AT_Ch9.indd 237 11/14/13 1:07 PM Foam: A Unique Delivery Vehicle for Topically Applied Formulations PY O C “emollient foam,” which was initially introduced by Stiefel and is now also being extensively developed by Foamix. Water-containing foams have several general advantages: (1) Usability. Foam formulations containing water offer cosmetically pleasing advantages over traditional topical vehicles such as ointments and creams. These include easy application, minimal residue after application, and quick absorption into the skin. Studies have revealed that patients using foam preparations spent less time applying medication when compared with other topical medications.18 (2) Stability. The pressurized aerosol container is an impermeable packaging system, which prevents formulation contact with air, light, and contaminants during storage, as well as during the use period. This differentiates foam packaging from tubes, which, although minimally, are exposed to the environment once they are opened. Hence, drugs prone to oxygenation or sensitive to light can have longer shelf life and in-use life when formulated in a foam. (3) Skin hydration and conditioning. In emulsion-based foams, the hydrophobic components, which are primarily liquid oils, act to mitigate skin dryness through their emollient properties. The mechanism is thought to involve increased skin hydration (water content) and reduction in water evaporation (transepidermal water loss, or TEWL) a process which contributes to the softening and pliability of the external layer of the skin (epidermis). Humectants, such as alpha hydroxy acids, propylene glycol, hexylene glycol, glycerol and urea, can be added to the aqueous phase of the emulsion. The following sections will review the compositions of the various watercontaining foam platforms. T H IG R ED Cream Foam (Emollient Foam) The term emollient foam relates to foams that exert soothing and moisturizing effects when applied to the skin. Emollient foams are emulsions, comprised of water and oil, and as such possess vehicular properties similar to traditional creams and lotions. The emulsions can be oil-in-water (o/w) or inverted (water-in-oil; w/o) emulsions, which correspond to “hydrophilic creams” and “hydrophobic creams,” respectively. The oil components of the foam contribute to improved skin condition and provide symptomatic relief of dry skin and associated skin diseases such as psoriasis and atopic dermatitis. 19,20 Emollient Foam Composition: The primary components of emollient foams are water and oil, which are present in the formulation as the form of emulsion. The composition of the oil phase can be selected from all cosmetically and pharmaceutically acceptable oils, including mineral oil; plant-derived oils and esters, such as capric/caprylic triglycerideisopropyl myristate, isopropyl palmitate and diisopropyl adipate; and silicone oils, which are known for their emolliency, wetting and spreading characteristics and ability to provide unique aesthetics. Petrolatum is a less desirable hydrophobic component, due to its greasy nature.21 238 AT_Ch9.indd 238 11/14/13 1:07 PM Chapter 9 PY O C Formulations that include high concentrations of petrolatum leave a greasy and sticky feeling after application and occasionally stain clothing. The foaming agents that are required to stabilize the emulsion and produce foam with desirable texture include surfactants, polymers, and foam adjuvants. The surfactants should be carefully selected. Ionic surfactants are effective as foaming agents but they are generally known as irritants, and therefore, nonionic surfactants are preferred, especially when the target area of treatment is inflamed or infected or is a mucosal surface or body cavity. A gelling agent is a useful component for the creation of foam with desirable texture and spreading properties. A variety of gelling agents also possess film-forming properties, which serve to maintain drugs at the site of application. Another group of components that contribute to the stability and sensory properties of the foam are the aforementioned foam adjuvants, which assist the surfactants in stabilizing the emulsion and forming stable foam. The adjuvants are selected from the variety of fatty alcohols and fatty acids.22,23 Optionally, polar solvents such as glycerol, propylene glycol, hexylene glycol, dimethyl isosorbide, and DMSO are added to the foam composition, in order to increase the solubility of the active agents and to enhance skin penetration.24 The propellant can be a hydrocarbon propellant (mix of butane, propane, and isobutene) or a fluorocarbon gas. A pharmaceutical or cosmetic emollient foam product may include a single active agent or a combination of active agents, which can be dissolved in the water phase or the hydrophobic phase of the carrier composition. Yet, in certain cases, the foam as a vehicle can still allow the dispersion of the drug even when it is not fully soluble in either the water or oil phases. Examples of drugs that have been successfully incorporated in emollient foam formulations include antibiotics, antifungals, antivirals, corticosteroids, non-steroidal anti-inflammatory agents, retinoids, keratolytic agents, immunomodulators, anesthetic drugs, anti-allergic agents, and anti-proliferative drugs.25-26 Emollient Foam Properties: Emollient foams possess several advantages, when compared with hydroethanolic foams: (1) Breakability. The emollient foam is thermally stable. Unlike hydroethanolic foams, it does not readily collapse upon exposure to skin temperature. Shearforce breakability of the foam is clearly advantageous, since it allows comfortable application and well directed administration to the target area. (2) Skin hydration and skin barrier function. The oil components of the foam provide skin conditioning and enhance the skin barrier function, thereby improving the condition of damaged skin. (3) Reduction in adverse effects. Due to the lack of alcohol and improvement in skin barrier function, skin irritability is reduced. (4) Usability. Foam provides significant usability advantages. When the foam is released from its container, it expands and allows easy spreading on the target area, and is absorbed into the skin without any extensive rubbing. This feature is particularly important with regard to the treatment of large skin surfaces. The fact T H IG R ED 239 AT_Ch9.indd 239 11/14/13 1:07 PM Foam: A Unique Delivery Vehicle for Topically Applied Formulations that when applied to skin the foam remains on the applied area and does not leak or drip is an additional usability advantage. The following examples demonstrate the implications of the above mentioned advantages. PY O C Betamethasone Valerate Emollient Foam An emollient foam composition, containing 0.12% of betamethasone valerate, was developed with the aim of treating patients with psoriasis and atopic dermatitis. The composition includes delicate oils and nonionic surfactants, in order to minimize skin irritation. A Phase II, randomized, blinded, right-left comparison within patient clinical trial was carried out with 30 patients with mild to moderate psoriasis. Two similar plaque areas of psoriasis, i.e. both knees or both elbows, were selected for treatment for each patient. Foam was administered on one side and a commercially available betamethasone valerate 0.12% cream was administered on the other side for a period of six weeks. The following results were recorded: Efficacy: Both treatments were equally effective in the treatment of the psoriatic lesions. After three weeks of treatment, there was a statistically significant improvement from baseline in all parameters, including thickness (4243% improvement), redness (3644%), scaling (4956%), itch (7778%) and global score (4244%). These clinical improvements persisted following an additional three weeks of treatment (Figure 1). Usability: Patients rated the foam as better than the cream in skin absorption, oily residue, shiny look, stickiness, and odor (Figure 2). The favorable usability of the foam is a major advantage, which contributes to enhanced patient compliance and better clinical outcome of treatment. Safety: No drug-related adverse effects were recorded in both treatments. In conclusion, the emollient foam offers an attractive alternative to mid-potency steroid cream. As such, it is more likely that psoriasis patients will use their medication as frequently as prescribed and will gain the desirable therapeutic benefits. T H IG R ED Figure 1. Betamethasone Emollient Foam—clinical improvement of psoriasis lesions following three weeks of treatment 240 AT_Ch9.indd 240 11/14/13 1:07 PM Chapter 9 PY O C Figure 2. Usability preference–Foam vs. Cream T H IG R Metronidazole 1% Emollient Foam – Demonstration of Efficient Drug Solubilization and Favorable Skin Bioavailability Metronidazole, the leading topical drug for rosacea, is currently available in gel, cream, and lotion at 0.75% and 1% concentrations. Since the saturation solubility of metronidazole in water is relatively low (≤ 0.75%), 1% metronidazole is not expected to fully dissolve in an aqueous vehicle. Emollient foam compositions, including delicate emollient oils and nonionic surfactants, were designed with the aim of dissolving 1% metronidazole. Surprisingly, the foam fully solubilized the active ingredient, as shown in Figure 3. An in vitro skin penetration study was conducted using excised human skin, aiming to evaluate the penetration profile of 1% metronidazole from two types of emollient foams. Two foam compositions were tested–one with 2.5% propylene glycol as a penetration enhancer and the other without propylene glycol (MZPG and MZ, respectively). These were compared to a commercial 1% metronidazole cream. As shown in Figure 4, the total cutaneous penetration of metronidazole following 16 hours’ exposure was two- to threefold higher for the two foams when compared to the commercial product. Propylene glycol increased significantly the delivery of metronidazole through the skin. The full solubility of the active agent in the foam formulation, as shown in Figure 3, is conceivably the explanation for the better penetration from the foam products. Particles will obviously not penetrate the stratum corneum. Thus, the enhanced solubility of the drug in the emollient foam is useful in enhancing the effectiveness of topical metronidazole. ED 241 AT_Ch9.indd 241 11/14/13 1:07 PM Foam: A Unique Delivery Vehicle for Topically Applied Formulations Figure 3. Metronidazole 1% emollient foam versus commerical cream (a) No crystals in the 1% emollient foam (b). Metronidazole crystals in commercial product PY O C T H IG R ED Figure 4. The skin penetration profile of Metronidazole 1% emollient foam with 2.5% propylene glycol as a penetration enhancer (MZPG) and without propylene glycol (MZ) vs. cream. 242 AT_Ch9.indd 242 11/14/13 1:07 PM Chapter 9 (a) enhanced intradermal delivery and controllable transdermal delivery by both foams; and further, induction of transdermal delivery by propylene glycol (b) delivery of metronidazole to all skin layers Numerous cosmetic and over-the-counter (OTC) products have been conceived as suitable for a foam delivery format. Several such products are at various stages of development. Table 2 describes some of these cosmetic foams, their active ingredients and their properties. PY O C T H IG R ED 243 AT_Ch9.indd 243 11/14/13 1:07 PM Foam: A Unique Delivery Vehicle for Topically Applied Formulations Table 2. Examples of Cosmetic and Nonprescription Emollient Foams Product Active Agent Salicylic Acid Acne Foam 2% Salicylic Acid BPO Anti-acne Foam 5% Benzoyl Peroxide Scytera 2% Coal Tar PY O C 3% Mg Ascorbyl Phosphate (MAP) T H IG R Skin Whitening Foam ED “Instant” Skin Whitening Foam MAP + Titanium Oxide Anti-cellulite and Body Firming Foam 5% Caffeine Sunscreen Foams Type II: Type I: chemical Micronized zinc oxide & Titanium dioxide Type II: physical Type III: combination chemical and physical 244 AT_Ch9.indd 244 11/14/13 1:07 PM Chapter 9 Properties Comments Non-greasy o/w emulsion Salicylic acid is listed as an anti-acne agent under the FDA OTC monograph. Alcohol-free (no skin drying or irritation) Moisturizing effect, to mitigate the drying effect of the active agent Non-greasy o/w emulsion Contains the Natural Moisturizing Factor (NMF) , to mitigate the drying effect of the active agent Benzoyl peroxide is a highly effective anti-acne agent, approved by FDA for OTC use. Alcohol-free Preservative-free Non-greasy o/w emulsion The foam presentation decreases color intensity of coal tar from dark brown to off-white, making it stain-free C PY O The unique formulation neutralizes the typical smell of coal tar. Suitable for the treatment of scalp and whole body psoriasis. Coal Tar is a highly effective anti-psoriasis and antiseborrheic agent, approved by FDA for OTC use. The product is currently marketed in the United States and will become available worldwide. O/W emulsion Alcohol-free Proprietary product. Drip-free Cosmetically elegant Active approved in Japan for skin whitening. ED Skin lubricating and conditioning effect Based on the emollient foam technology platform. T Moisturizing effect H IG R Suitable for the treatment of dandruff and seborrheic dermatitis. As above with instant “cosmetic” whitening provided by titanium oxide Based on the emollient foam technology platform. Sun protection as an added benefit Proprietary product. Unique combination product. Alcohol-free (no skin drying or irritation) Based on the emollient foam technology platform. Moisturizing effect (builds skin barrier) Proprietary product. Refatting effect Uses penetration enhancers, to increase efficacy. O/W emulsion Drip-free Cosmetically elegant–spreads easily on large areas Alcohol-free (no skin drying or irritation) O/W or w/o emulsion foams. Moisturizing effect (builds skin barrier) Proprietary products. Ability to include solids in Cosmetically elegant–spreads easily on large areas foam based on Foamix’s suspension foam technology. Drip-free 245 AT_Ch9.indd 245 11/14/13 1:07 PM Foam: A Unique Delivery Vehicle for Topically Applied Formulations Nanoemulsion Foam Nanoemulsion foam is a thermodynamically stable system with a typical droplet size in the range of 20–200 nm. Nanoemulsions show great promise for the future of topical drug therapies and cosmetics. They enable the solubilization of hard-todissolve active agents and increase their bioavailability, resulting in improved efficacy. The technology is suitable for a variety of actives, including water-soluble and oil-soluble molecules, vitamins, hydroxyl acids, peptides and proteins, retinoids, antimicrobial, antifungal and antiviral agents, NSAIDs and hormones. Hydroethanolic Foam PY O C Hydroethanolic foams are the foam version of alcohol solutions and tinctures. Olux Foam and Luxiq Foam (Stiefel Laboratories), which contain 0.05% clobetasol propionate and 0.12% betamethasone valerate, respectively, were the first commercially available dermatological foams, and they gained high acceptance by physicians and patients. These are thermolabile foams, consisting of ethanol (about 60%), water, propylene glycol, cetyl alcohol, stearyl alcohol, polysorbate 60, citric acid, potassium citrate, and a hydrocarbon propellant. The launch of these products was followed by Extina Foam (ketoconazole foam 2%) and Evoclin Foam (clindamycin foam 1%). Studies conducted in vitro demonstrated that drugs, formulated in hydroethanolic foam exhibit delivery at an increased rate compared with other vehicles. For example, an in vitro skin penetration study, using Franz cells, demonstrated that the hydroethanolic foam vehicle delivered more clobetasol propionate through the skin (5.3%) than the comparator solution, cream and lotion vehicles (2.8%, 2.7%, 2.1% and 1.8% respectively).11 These findings suggest that components within the foam (probably the alcohol) act as penetration enhancers, and alter the barrier properties of the outer stratum corneum, thus driving the delivered drug across the skin membrane via the intracellular route. Since alcohol evaporates quickly from the skin, it also promotes fast drying of the skin and therefore is used to ameliorate the sticky feeling left by many topical formulations after application. However, alcohol extracts stratum corneum and sebum lipids that naturally moisturize the skin and therefore may cause skin to become dry and cracked. Due to this undesirable property, hydroethanolic foams have not been proposed for the treatment of atopic dermatitis, a childhood inflammatory skin disorder that involves dry, itchy skin and rashes on various body areas. Atopic dermatitis is also characterized by impaired skin barrier and enhanced penetration, and the use of ethanol can further promote percutaneous absorption instead of targeted delivery to skin layers. The high incidence of skin irritation (burning, itching and stinging) as noted, for example, in the package insert of Luxiq Foam (54% ethanol content) is probably due to the high content of alcohol content, in combination with surfactants which are known skin irritants. Moreover, an even higher incidence of skin irritation was reportedly caused by this foam vehicle (75%); 27% of the population tested/using T H IG R ED 246 AT_Ch9.indd 246 11/14/13 1:07 PM Chapter 9 PY O C the product reported moderate-to-severe irritation. Furthermore, since alcohol is an irritant to mucosal surfaces, the label of these products states, “Avoid getting the foam in or near your eyes, mouth, lips, or broken skin.” In addition, the current hydroethanolic foams are thermolabile and their usage is hindered by the recommendation not to dispense them directly onto the hands, as the foam melts immediately upon contact with skin temperature. Instead, the foam is to be dispensed onto a cool surface, and then small amounts of foam should be picked up using the fingers and gently massaged into affected area.27 Thus, while alcohol is useful in solubilizing an active agent and enabling effective dermal penetration of drugs, the development of less irritable foam vehicles, which overcome the evident skin drying and irritation caused by the combination of alcohol and surfactants, was warranted. One of the means to achieve this goal is adding emollient oils to the foam composition. Such emollients provide skin conditioning effects, build up the skin barrier properties, and reduce skin irritation. An example of such commercially available foam is Scytera (Promius Pharma, developed by Foamix), a product containing 2% coal tar for the treatment of psoriasis. Scytera contains alcohol, but it also contains emollients. This novel foam vehicle is versatile and may be used to treat psoriasis even in areas of the body where the application is challenging, such as the scalp, palms, and soles.28,29 An additional way to overcome the usability limitations of the traditional hydroethanolic foams, which was developed by Foamix, is to omit the surfactants or to replace them by polymeric agents, resulting in foams which are thermally stable.30,31 The absence of surfactants in the formulation further decreases the irritation potential of such formulations. T H IG R ED Potent Solvent Foam A new platform of foam formulation is intended to promote transdermal skin delivery of drugs via the addition of high concentrations of skin penetration enhancers. Following the recent FDA approval of products containing up to 40% DMSO, an aqueous foam comprising 40% DMSO was developed by Foamix, which is suitable as a carrier for non-steroidal anti-inflammatory drugs that are intended to treat osteoarthritis, as well as other drugs that can be administered transdermally.32 Water-free Foams The creation of foam formulations without water is counterintuitive. It is known in the art that foams can easily be formulated based on high amounts of water, in combination with surface active agents, foam adjuvants, and polymeric agents. As described in the literature, hydrophobic excipients, such as petrolatum, oils, and hydrophilic solvents, can have a de-foaming effect which makes the formulation of foams based on such solvents challenging. To overcome this challenge, substantial levels of surfactants that act as foaming agents have been used in the past; however, many surface active agents are known to be irritating to skin, especially ionic surface 247 AT_Ch9.indd 247 11/14/13 1:07 PM Foam: A Unique Delivery Vehicle for Topically Applied Formulations PY O C active agents, and repeated application to the skin or mucosa in high concentrations can damage the integrity of the skin barrier and cause dryness and irritation. Newly-developed water-free foams, which contain limited amounts of surfactants or no surfactants at all, are currently under development. While water-free foams are as-yet unavailable commercially, several products based on such foams that are under development are described in following sections. Water-free foams have several advantages: (1) Stability. The first and foremost advantage is that water-free foams are perfect vehicles for drugs and cosmetic active agents that undergo decomposition or are unstable in water. Many active agents, including corticosteroids, steroid hormones, immunomodulators, antibiotics, and water-soluble vitamins such as vitamin C, as well as other actives that contain ester groups, tend to degrade in the presence of water, so a vehicle that does not contain water is preferred. Moreover, the pressurized aerosol container is an impermeable packaging system, and as such, it prevents contact of the formulation with ambient moisture even during the use period, unlike tubes which are exposed to the environment once they are opened. (2) Self-preservation. Microorganisms require water to grow and reproduce. A water-free foam formulation prevents the growth of bacteria, molds and fungi during storage, and, as mentioned, the entry of moisture into the aerosol pressurized can is prevented during the use period, so water-free foams do not require the inclusion of preservatives. (3) Usability. Today’s water-free topical formulations are primarily ointments, which are characterized by being thick and greasy, and they require extensive rubbing for efficient topical application. In contrast, foams are structurally soft and their application is facile. They spread easily onto the skin and absorb quickly. (4) Skin hydration & conditioning. Hydrophobic excipients such as petrolatum and liquid oils act to mitigate skin dryness and ameliorate inflammation through their emollient and humectant properties. They make the external layers of the skin (epidermis) softer and more pliable, thereby increasing the skin’s hydration (water content) by reducing water evaporation. Hydrophilic excipients, such as polyethylene glycol, propylene glycol, and glycerin are hygroscopic—they attract ambient water and retain skin moisture. Water-free foams are rich with such emollients and humectants, so they maximize skin hydration and conditioning. T H IG R ED Ointment Foam – Petrolatum-based Foam Ointment foam is the foam version of traditional petrolatum-based ointments.33 When applied to skin, petrolatum can generate an occlusive layer and lower TEWL. Petrolatum-based foam formulations may be complicated to make, especially due to the high viscosity of the hydrocarbon; however, there are now under development ointment foams that contain up to 90% petrolatum. The foaming agents in such formulations include small amounts of foam adjuvants and nonionic surfactants. The propellant is typically hydrocarbon. Due to the unique texture of the foam, it instantly liquefies and spreads easily 248 AT_Ch9.indd 248 11/14/13 1:07 PM Chapter 9 PY O C onto the skin upon application, and no extensive rubbing is required. Thus, the benefit of petrolatum’s occlusive shield is retained without the thick texture and greasy feel of traditional ointments. This usability feature is especially valuable in the treatment of infants and children who suffer from dry skin conditions like atopic dermatitis. In such cases, the effect of the drug is accompanied by the synergistic skin barrier buildup, and lubricating and protective properties of the vehicle. Examples of drugs that can benefit from this type of formulation include corticosteroids, which are typically applied to large areas of dry, inflamed and damaged skin, anti-infective agents (antibacterial, antifungal, and antiviral drugs) and immunomodulators (such as pimecrolimus and tacrolimus) which are used to treat atopic dermatitis. An illustrative example is a unique petrolatum-zinc oxide foam (petrolatum and natural oils, 91%; zinc oxide, 15%). Petrolatum is approved by FDA as an OTC active ingredient that helps treat and prevent diaper dermatitis, seal out wetness, and temporarily protect against and provide relief from chapped or cracked skin, as well as minor cuts, scrapes, and burns. Likewise, zinc oxide, the active ingredient in many diaper dermatitis products, is a skin protectant and an antimicrobial agent. It protects by forming a protective barrier on the skin, preventing wetness and other irritants from reaching the skin underneath. Unlike traditional petrolatum-based pastes for diaper dermatitis, which are very thick and hard to apply to the baby’s sensitive skin, the petrolatum-zinc oxide foam is easy to apply, and still provides the same protective and healing effects. This synergistic composition can be further enhanced by the addition of an antimycotic agent (such as miconazole, ketoconazole, clotrimazole, or nystatin) to eradicate yeast infections. T H IG R ED Oil Foam Oil foam is the foam version of traditional oil-based solutions and suspensions.34 Oil foam is one of the most promising foam platforms for use in dermatology, as it can utilize a broad range of pharmaceutical liquid oils, including mineral oil, plantderived oils (e.g., olive oil, soybean oil, and castor oil), emollient esters and alcohols (e.g., isopropyl myristate, isopropyl palmitate, diisopropyl adipate, isostearic acid, and oleyl alcohol), and silicone oils. Despite the fact that oils are generally known as de-foaming agents and their incorporation in foam formulations is challenging, studies have shown that use of a unique proprietary technique can yield a foamable composition containing more than 90% oil content. Such a composition contains very small amounts of foaming agents and no water whatsoever. The foaming agents include lipophilic surfactants with low HLB, foam adjuvants (fatty acids and fatty alcohols), waxes, and polymers. In certain cases, when a drug is to be included in the vehicle that is incompatible with surfactants, the aforementioned technique even allows the creation of foam compositions with no surfactants at all. 35-36 The most suitable propellants for such foams are hydrocarbon propellants. Oil foams have a very soft and airy texture; they spread effortlessly on the target surface and quickly absorb into the skin, leaving no greasiness at all. In fact, oil 249 AT_Ch9.indd 249 11/14/13 Figure 1. Typical Mixer Power Curve 1:07 PM Foam: A Unique Delivery Vehicle for Topically Applied Formulations PY O C foams are so cosmetically elegant that they can be used for the treatment of facial conditions, even if those conditions are associated with oily or sensitive skin, as in the cases of acne and rosacea. Oil foam is the most suitable form to accommodate unstable drugs. For example, it has been used as a vehicle for calcipotriene and calcitriene, two vitamin D3 analogs to treat psoriasis and atopic dermatitis, resulting in stable drugs with more than two years of shelf life. The most advanced oil foam product in private development is Minocycline Foam (1% and 4%).37,38 Minocycline is an antibiotic known to be very unstable, since it is degraded by a wide range of commonly used pharmaceutical excipients. For example, it degrades readily in the presence of hydrophilic solvents (such as water, glycerin, sodium PCA, propylene glycol and polyethylene glycols), polymers (such as xanthan gum, poloxamers, carbomers, and methocel), and surfactants (such as polysorbates, sorbitan esters, polyoxyalkyl esters, and lanolinbased surfactants). Hence, the development challenge was to attain a stable foam composition without the hydrophilic compounds, which are usually used as foaming agents. A series of development efforts resulted in a water-free, alcohol-free, and surfactant-free formulation which contains more than 80% liquid oils, where the foaming agents are fatty alcohols, fatty acids, and waxes. The Minocycline foam has the following features: Stability: Minocycline Foam 1% and 4% exhibit high stability. They remain within the designated specifications following 12 months’ storage at 40 ºC and over 24 months at 25ºC. Antibacterial effects: In vitro studies have demonstrated that Minocycline Foam 1% and 4% effectively inhibited the growth of Streptococcus pyogenes, Pseudomonas aeruginosa, Staphylococcus aureus, a methicillin-resistant strain of Staphylococcus aureus (MRSA), and Propionbacterium acnes, the causative microorganism in acne. Inhibition of inflammation and apoptosis: UVB irradiation of the skin is known to decrease cell viability and total antioxidant capacity, while increasing the levels of inflammation (pro-inflammatory cytokines secretion) and epidermal cell apoptosis. Exploratory studies have revealed the beneficial effects of Minocycline foam on cell viability and apoptosis of skin cells: treatment prior to irradiation results in more than 50% inhibition of apoptosis, as measured by caspase 3 activity; and treatment after irradiation results in 60% inhibition of apoptosis, as measured by caspase 3 activity. Capsase 3 is a cytokine that plays a key role in apoptosis, defined as programmed cell death that is accelerated in inflamed tissues.44 Targeted delivery of Minocycline into the skin: The transdermal penetration of Minocycline was tested using the Franz cell in vitro diffusion system, with porcine ear skin. Approximately 500 mg of product was placed in each cell; the receiver compartments were sampled at baseline and 3, 6, 9 and 24 hours following application, respectively. After 24 hours the amounts of Minocycline in the upper and lower stratum corneum layers (SC1 and SC2) and viable skin were analyzed. As shown in Table 3, the drug was delivered exclusively into the skin. The mean amount of T H IG R ED 250 AT_Ch9.indd 250 11/14/13 1:07 PM Chapter 9 Minocycline in the skin following 24 hours of exposure was 9.5 g/cm2 for the 1% formulation and 43 g/cm2 for the 4% formulation. The weight of skin at the delivery area is about 100 mg, which implies that the concentration of Minocycline in the skin following 24 hours of exposure is about 168 g/gr of skin for the 1% formulation and about 760 g/gr for the 4% formulation. This amount is an effective dose for the treatment of bacterial skin infections. No transdermal passage of Minocycline was observed, indicating that Minocycline foam should not generate any systemic adverse effects.44 Table 3. Minocycline Foam 1% and 4%; Measure Skin Delivery Comparison Minocycline Foam 1% (n=5) Minocycline Foam 4% (n=6) Minocycline g/cm2 STD Minocycline g/cm2 STD C Stratum Corneum SC1 7.77 4.32 33.63 20.41 0.93 0.77 7.49 8.67 8.70 4.97 41.12 16.89 Receiving Compartment (Transdermal Delivery) 0.79 0.19 2.00 0.81 9.49 4.99 43.12 17.48 - 0.00 - R Total Intradermal Delivery IG Viable Skin PY O Stratum Corneum SC2 Total Stratum Corneum 0.00 T H ED Figure 5. Percent reduction of inflammatory, non-inflammatory and total count of acne lesions Minocycline foam is safe and effective in the treatment of acne:39 A randomized double-blind dose-ranging Phase II clinical study was conducted to assess the efficacy and safety of Minocycline foam in 150 patients with moderate to severe acne who received placebo or one of two Minocycline foams (1% or 4%) once daily. 251 AT_Ch9.indd 251 11/14/13 1:07 PM Foam: A Unique Delivery Vehicle for Topically Applied Formulations As shown in Figure 5, six weeks’ treatment was enough to reach more than 70% reduction in the inflammatory lesions. Even after three weeks of treatment the reduction of inflammatory lesions was 53% and statistically significant. The effects were dose-dependent, as demonstrated by the higher effects of the 4% foam and the placebo. Figure 6 exemplifies an acne patient who had 49 lesions at baseline (23 inflammatory lesions, 26 non-inflammatory lesions) and who improved dramatically after nine weeks of treatment. PY O C IG R Figure 6. Photographic documentation of the effect of Minocycline foam in a severe acne patient. Dramatic improvement is observed after 9 weeks of treatment. T H Minocycline foam is safe and effective in the treatment of impetigo39: A randomized double blind dose-ranging Phase II clinical study was designed to assess the efficacy, safety, and tolerability of two strengths of the Minocycline foam in pediatric patients with impetigo. Impetigo is a highly contagious bacterial skin infection. The study enrolled 32 pediatric patients ages 2 to 15 with at least two impetigo lesions. Patients applied the foam twice daily for 7 days; and they were checked again on day 14. Strong efficacy was demonstrated in both 1% and 4% levels. Clinical effectiveness was defined as the absence of treated lesions, or treated lesions that had become dry without crusts with or without erythema compared to baseline, or had improved (defined as a decline in the size of the affected area, number of lesions, or both) such that no further antimicrobial therapy was required. Notably, about 80% of the patients in both groups saw improvement, or disappearance of the lesions, and met the efficacy criteria after 3 days of treatment. Clinical response at the end of the treatment was 92% and 100% respectively for the low or high doses; and all patients (100%) demonstrated improvement on day 14 (Table 4 and Figure7). Eleven of the study patients had methicillin-resistant Staphylococcus aureus (MRSA) infection at baseline, and in all cases the infection was eradicated on day 7. Minocycline foam was well-tolerated and no drug related side effects were recorded in any of the patients throughout the study. Questionnaires, filled by the patients’ caregivers revealed high satisfaction from treatment. ED 252 AT_Ch9.indd 252 11/14/13 1:07 PM Chapter 9 Table 4. Minocycline Foam 1% and 4%: Success rate at Day 3, Day 7 (End of Treatment) and Day 14 (Follow-up) 1% 4% All Day 3 81.3% 78.6% 80.0% Day 7 (EOT) 92.3% 100.0% 95.8% Day 14 (FU) 100.0% 100.0% 100.0% PY O C T H IG R ED Figure 7. Photographic documentation of the effect of Minocycline foam in pediatric patients with impetigo, demonstrating visible improvement or clearance of lesions within 3 to 7 days of treatment. Hydrophilic Waterless Foam Hydrophilic waterless foam is the foam version of traditional hydrophilic ointments. This foam can contain up to 98% polar hydrophilic solvent, which may be selected from the following groups of compounds: (1) polyols (organic solvents that contain at least two hydroxy groups in their molecular structure); and (2) polyethylene glycols (PEGs). The polyols can be selected from the group of di-alcohols, such as propylene glycol, butanediol and diethylene glycol, and tri-alcohols, such as glycerin. The PEGs can be primarily low-molecular weight liquid PEGs, such as PEG 200, PEG 400, PEG 600 and PEG 1000; however, mixes of the liquid PEGs with higher molecular weight such as PEG 4000, PEG 6000, and PEG 8000 may be used as long as the viscosity, prior to filling of the composition into aerosol canisters, is less than about 10,000 CPs. The addition of secondary polar solvents, such as dimethyl isosorbide, ethoxydiglycol, DMSO, and alpha hydroxy acids, such as lactic acid and glycolic acid, is sometimes warranted in order to enhance solubilization and skin 253 AT_Ch9.indd 253 11/14/13 1:07 PM Foam: A Unique Delivery Vehicle for Topically Applied Formulations permeation of the drug.40 These properties enable increased permeability across the skin, resulting in an enhanced therapeutic effect. The foaming agents include up to 5% surfactants and small amounts of polymers, and the propellants can be hydrocarbon propellants and fluorocarbons. Polyols, PEGs, and other polar solvents have a great affinity for water; as such, they exhibit hygroscopic properties. Microorganisms require water to grow and reproduce, thus the high concentration of polar solvents that absorb and hold free water in order that it be unavailable for bacterial population, the result being an inhibition of the growth of bacteria and fungi. Consequently, waterless hydrophilic foams do not require preservatives in their composition; furthermore, their application onto an infected skin surface can be used as a topical treatment for superficial infectious conditions. It is further possible to add an anti-infective (antibacterial or antifungal) element that may enhance the formulation’s effect and, consequently, render higher treatment success.41,42 PY O C Saccharide Foam Saccharide foam, which contains up to 90% monosaccharides, disaccharides, or honey was developed for the treatment of wounds and burns.43 The foam is soft and easy to apply on the target site of treatment, with no need for extensive rubbing. It is hygroscopic, and thus it has anti-infective attributes and absorbs exudates. In addition, high percentages of sugars in the formulation are known to generate a high-osmolality environment that is hostile to microbial proliferation. H IG R T How to Formulate Foam Products ED Most foams used in pharmacological and cosmetic applications are aerosol foams, which comprise a semi-solid formulation, packaged in an aerosol can and pressurized by a propellant. An aerosol is made up of several basic components: •An aerosol can •The bulk product (semi-solid formulation) •The propellant •A valve •An actuator •A dust cap The preparation of the semi-solid bulk (termed pre-foam formulation or PFF) depends on the type of composition used. For example, emollient (emulsion-based) foams are produced in the following sequence: 1. PFF production (a) Aqueous Phase preparation: Gelling agents and surface-active agents are dissolved in water with agitation. The solution is warmed to 50–70°C. Water-soluble cosmetic or pharmaceutical active ingredients and optional water-soluble ingredients are added with agitation to the aqueous phase mixture. 254 AT_Ch9.indd 254 11/14/13 1:07 PM Chapter 9 PY O C (b) Hydrophobic phase preparation: The hydrophobic solvent is heated to 50–70°C. Foam adjuvants (e.g., fatty alcohols and/or fatty acids) are added to the hydrophobic solvent with agitation; followed by the addition of oil-soluble cosmetic or pharmaceutical active ingredients and other optional oil-soluble formulation ingredients. (c) The warm hydrophobic phase is gradually poured into the warm aqueous phase, with agitation, followed by homogenization. The mixture is allowed to cool down to ambient temperature. In case of heat-sensitive active ingredients, they can be added with agitation to the mixture after cooling to ambient temperature. 2. Packaging and pressurization The mixture, at ambient temperature, is added to an aerosol container, the container is sealed with a valve and an appropriate amount of propellant (typically 6–12% of the composition) is added under pressure into the container. The most commonly used propellants are hydrocarbon mixtures, which comprise n-butane, isobutane, and n-propane in various ratios. These hydrocarbons are gasses at ambient temperature; however, when stored under pressure, they are liquefied. Alternatively, fluorocarbon propellants, such as 1,1,1,2 tetrafluorethane and 1,1,1,2,3,3,3 heptafluoropropane, can be used. When single-phase foams are prepared, such as aqueous foams and hydroethanolic foams, as well as oil foam and waterless hydrophilic foams, the primary solvents and foaming agents are mixed together to form a uniform bulk PFF, which is in turn added to the aerosol can and pressurized as described above. W hile the preparation of PFFs can be performed in any formulation laboratory, the stages of packaging into the aerosol cans and the pressurization require specialized equipment. The assembly of the valve to the can is carried out using a specialized crimper, which compresses the edges of the valve and secures tight attachment of the valve to the can. This is a very critical operation and the crimping machinery has to be carefully set up to ensure that the can/valve seal does not leak. The preferred crimper for this operation is a “vacuum crimper,” which is capable of drawing the air from the can prior to sealing it with the valve. The pressurization of the product also requires specialized equipment, as the propellant is injected into the can under pressure, through the valve. The propellant may be in the form of a liquefied gas, or a compressed gas. When a liquefied gas is used it will exist as both a liquid, and vapor in the aerosol can head space. A significant part of the propellant will be dissolved in the PFF, resulting in an increase of the volume of the semi-solid bulk. To ensure product integrity, each can is immersed in a water bath at 50°C to check for any leaks. Any cans that leak are rejected. Once the process of preparing the PFF, packaging it in the aerosol can, and pressurizing it is completed in laboratory scale, it is usually readily scalable to commercial amounts, using industrial manufacturers. T H IG R ED 255 AT_Ch9.indd 255 11/14/13 1:07 PM Foam: A Unique Delivery Vehicle for Topically Applied Formulations Methods of Evaluation of Foam Products The following section provides test methods for the evaluation of foam products. The chemical analysis is important to ensure the compliance of a product with the specified concentration of active ingredients, and to follow-up the stability of the active agents. The physical parameters are also related to the integrity, uniformity, and stability of the product; moreover, they are important properties in terms of the usability of the product. PY O C Chemical Analysis Active ingredients and preservatives are commonly quantified in pharmaceutical and cosmetic preparations as part of the quality control and stability evaluation of such products. Foams are unique in the sense that the composition within the aerosol container includes a propellant, which evaporates immediately upon dispensing. Therefore, it has been accepted that the quantitation should be done in the absence of the propellant to mimic real “in use” conditions. Accordingly, the testing sample preparation includes (1) shaking the canister well and dispensing an initial quantity to waste; (2) transferring to a beaker a sufficient quantity for duplicate preparation; (3) de-aerating the dispensed foam by mixing with a glass rod. Aliquots of the de-aerated sample are then weighed accurately and processed for analysis by chromatography (e.g., GC, HPLC or UPLC) using customary methods. The method of analysis of preservatives in Scytera was recently published by Dr Reddy.44 H IG R T Physical Foam Properties The physical characteristics of the foam are important for ensuring acceptance and facile usability of the product by the consumer. The principal physical properties of foam are presented below, alongside with the methods to quantify them. ED Foam quality: Foam quality can be graded as follows: Grade E (excellent): Very rich and creamy in appearance; does not show any bubble structure or demonstrates a very fine (small) bubble structure; does not rapidly become dull; upon spreading on the skin, the foam retains the creaminess property and does not appear watery. Grade G (good): Rich and creamy in appearance; very small bubble size; “dulls” more rapidly than an excellent foam; retains creaminess upon spreading on the skin and does not become watery. Grade FG (fairly good): A moderate amount of creaminess is noticeable; bubble structure is noticeable; upon spreading on the skin, the product dulls rapidly and becomes somewhat lower in apparent viscosity. Grade F (fair): Very little creaminess is noticeable; larger bubble structure than a FG foam; upon spreading on the skin, it becomes thin in appearance and watery. Grade P (poor): No creaminess is noticeable; large bubble structure; when spread 256 AT_Ch9.indd 256 11/14/13 1:07 PM Chapter 9 on the skin, it becomes very thin and watery in appearance. Grade VP (very poor): Dry foam, large very dull bubbles; difficult to spread on the skin. Topically administrable foams are typically of quality grade E or G, when released from the aerosol container. Smaller bubbles are indicative of more stable foam, which does not collapse spontaneously immediately upon discharge from the container. The finer foam structure looks and feels smoother, thus increasing its usability and appeal. PY O C Foam density: Density is also a distinguishing factor in at the assessment of the quality of foams. The density of a foam product is quantified by dispensing into vessels (including dishes or tubes) a known volume and weight of the foam product, as follows: The foam product is allowed to reach room temperature. The canister is then shaken well to mix the contents and 5–10 g of product are dispensed and discarded thereafter. Then, foam is dispensed into a pre-weighed tube, filling it until excess is extruded from the other side of the tube. The excess of foam at both ends is removed and then the tube, filled with foam, is weighed on an analytical balance. The density is calculated by dividing the net weight of the foam by the volume of the tube. Replicate measurements are recommended. The density of the foam is related to the foam class, as provided above. Watercontaining foams are less dense and their density is typically less than 0.1 g/mL. Frequently, the density of hydroethanolic foams and emollient foams is in the range of 0.03–0.06 g/mL, which makes their application very easy. Water-free foams are “heavier” when applied and their density can range from 0.1–0.25 g/mL. Even such dense foams spread very easily and absorb quickly into the skin. T H IG R ED Breakability and collapse time: An important property of foams is breakability, i.e., the way the foam breaks down or collapses upon release from the aerosol can. Foams can be classified into three classes: stable, quick breaking foam, and breakable. A typical example of stable foam is shaving foam. Shaving foams possess remarkable stability upon release from the aerosol can, and they do not break down even upon extensive rubbing onto the skin. Such stable foams are not suitable for topical therapy of skin conditions as they do not absorb into the skin upon application. By contrast, quick breaking foams are inherently unstable and thermolabile, i.e., they readily collapse or melt upon exposure to body temperature.45 The quick breaking property is usually caused by the presence of ethanol in the foam composition, and the breaking temperature can be somewhat modulated by changing the alcohol to water ratio in the quick-breaking temperature sensitive foam composition. The usability of quick breaking foams is hindered by the fact that the foam quickly collapses upon dispensing to one’s fingers prior to application to the target area. Breakable foams are thermally stable, yet break under shear force. Shear force 257 AT_Ch9.indd 257 11/14/13 1:07 PM Foam: A Unique Delivery Vehicle for Topically Applied Formulations breakability of the foam is clearly advantageous over thermally induced breakability. The breakable foam does not collapse quickly upon expulsion, and it does not readily collapse or melt upon exposure to skin temperature, allowing for comfortable application and well directed administration of the preparation to the target area. The difference between quick breaking thermolabile foam and breakable foam is illustrated in Figur8. In the figure, the breakable foam is stable, resulting in facile application and spreading, while the hydroethanolic foam instantly melts on the fingers, which makes the application to the target site challenging and difficult spreading over large skin areas. The tendency of a foam to collapse upon exposure to skin temperature is examined by dispensing a given quantity of foam and photographing sequentially its appearance over time at 36°C. This “collapse time” is determined as the time that elapses until the height of the foam is reduced to 50% of its original value. Preferably, to ensure convenient application, the foam should maintain its structural stability at skin temperature for at least 1 minute and, more preferably, more than 2 or 3 minutes. PY O C T H IG R ED Figure 8. Breakable emollient foam vs. quick breaking hydroethanolic foam 258 AT_Ch9.indd 258 11/14/13 1:07 PM Chapter 9 Summary Creams and ointments have been used historically in skin care and dermatology. Foams offer an innovative and more convenient means of topical treatment of the skin. The continuing development of versatile foam technology platforms will facilitate achieving new topical products, including valuable drugs for the treatment of dermatological mucosal and body cavity conditions. The advantages of foam in terms of enhanced usability and compliance, improved clinical safety, tolerability and efficacy, stability, and targeted drug delivery will enhance therapy and the future development of therapeutic and topical treatments and products. References PY O C 1. R Woodford and BW Barry, Bioavailability and activity of topical corticosteroids from a novel drug delivery system, the aerosol quick-break foam, J Pharm Sci, 66 1, 99-103 (1977). 2. M Parrini et al, Efficacy and tolerability of ketoprofen lysine salt foam for topical use in the treatment of traumatic pathologies of the locomotor apparatus, Clin Ter, 141 9, 199-204 (1992). 3. L Daffonchio et al, Effects of a new foam formulation of ketoprofen lysine salt in experimental models of inflammation and hyperalgesia, Arzneimittelforschung, 45 5, 590-4 (1995). 4. CH Purdon et al, Foam drug delivery in dermatology: Beyond the scalp, Am J Drug Deliv, 1 1, 71-75 (2003). 5. D Tamarkin et al, Emollient foam in topical drug delivery, Expert Opin Drug Deliv, 3 6, 799807 (2006). 6. D Tamarkin et al, Foam: The future of effective cosmeceuticals, Cosm &Toil, 121 11, 75-84 (2006). 7. A Arzhavitina and H Steckel, Foams for pharmaceutical and cosmetic application, Int J Pharm, 394 1/2, 1-17 (2010). 8.See EpiFoam Prescribing Information, accessed at: www.medapharma.us/products/pi/ Epifoam_PI.pdf. 9.Prescribing Information, accessed at: www.stiefel.com/content/dam/stiefel/globals/documents/pdf/US_Olux_Foam.pdf. 10.Prescribing Information, accessed at: www.stiefel.com/content/dam/stiefel/globals/documents/pdf/US_Luxiq.pdf. 11.Prescribing Information, accessed at: www.stiefel.com/content/dam/stiefel/globals/documents/pdf/US_Evoclin_Foam.pdf. 12.AR Shalita et al, The safety and efficacy of clindamycin phosphate foam 1% versus clindamycin phosphate topical gel 1% for the treatment of acne vulgaris, J Drugs Dermatol, 4 1, 48-56 (2005). 13.Prescribing Information, accessed at: www.stiefel.com/content/dam/stiefel/globals/documents/pdf/US_Olux-e_Foam.pdf. 14.Prescribing Information, accessed at: www.stiefel.com/content/dam/stiefel/globals/documents/pdf/US_Fabior.pdf. 15. www.scytera.com, accessed Sep 12, 2013. 16. M Lebwohl, A clinician’s paradigm in the treatment of psoriasis, J Am Acad Dermatol, 53 (Suppl. 1), S59–S69 (2005). 17. European Pharmacopoeia 05, pp 604-605 (2005). 18. L Stein, Clinical studies of a new vehicle formulation for topical corticosteroids in the treatment of psoriasis, J Am Acad Dermatol, 53 (1; Suppl 1), S39-49 (2005). 19. I Nola et al, The use of emollients as sophisticated therapy in dermatology, Acta Dermatovenerol Croat, 11, 80-87 (2003) 20. M Loden and AB Aco Hud, Role of topical emollients and moisturizers in the treatment of dry skin barrier disorders, Am J Clin Dermatol, 4, 771-788 (2003) T H IG R ED 259 AT_Ch9.indd 259 11/14/13 1:07 PM Foam: A Unique Delivery Vehicle for Topically Applied Formulations PY O C 21. DS Morrison, Petrolatum: A useful classic, Cosm & Toil, 111, 59-69 (1996) 22.Tamarkin et al, WO 2006/0140984, Cosmetic And Pharmaceutical Foam, assigned to Foamix. 23. Tamarkin et al, WO 2005/0186147, Cosmetic And Pharmaceutical Foam With Solid Matter, assigned to Foamix. 24.Tamarkin et al, US Patent No. 7,700,076, Penetrating pharmaceutical foam, assigned to Foamix. 25. Tamarkin et al, WO 2005/0186142, Kit And Composition Of Imidazole With Enhanced Bioavailability, assigned to Foamix. 26.Tamarkin et al, US Patent No. 8,119,109, Foamable compositions, kits and methods for hyperhidrosis, assigned to Foamix. 27. Use Instructions of Evoclin Foam, accessed at: www.accessdata.fda.gov/drugsatfda_docs/ label/2012/050801s015lbl.pdf. 28. AJ Frankel et al, Coal Tar 2% foam in combination with a superpotent corticosteroid foam for plaque psoriasis: Case report and clinical implications, J Clin Aesthet Dermatol, 3 10, 42-5 (2010). 29. Tamarkin et al, US Pat Appl. No. 20090180970, Foamable Composition Combining A Polar Solvent And A Hydrophobic Carrier, assigned to Foamix. 30. Tamarkin et al, WO/2011/013008, Non-Surface Active Agent Non Polymeric Agent HydroAlcoholic Foamable Compositions, Breakable Foams And Their Uses, assigned to Foamix. 31.WO 2011/013009, Non-Surfactant Hydro-Alcoholic Foamable Compositions, Breakable Foams And Their Uses, assigned to Foamix. 32.Tamarkin et al, WO 2010/125470, Foamable Vehicles and Pharmaceutical Compositions Comprising Aprotic Polar Solvents and Uses Thereof, assigned to Foamix. 33.Tamarkin et al, WO 2008/0260655, Substantially Non-Aqueous Foamable Petrolatum Based Pharmaceutical And Cosmetic Compositions And Their Uses, assigned to Foamix. 34. Tamarkin et al, US Patent No. 7,820,145, Oleaginous Pharmaceutical And Cosmetic Foam, assigned to Foamix. 35.Tamarkin et al, WO 2011/039637, Surfactant-free Water-free Foamable Compositions, Breakable Foams And Their Uses, assigned to Foamix. 36. Tamarkin et al, WO 2011/064631, Surfactant-free, Water-free, Foamable Compositions And Breakable Foams And Their Uses, assigned to Foamix. 37. Acknowledgement: The development of Foamix’s Minocycline Foam was supported by the Bird Foundation (www.birdf.com). 38. Tamarkin et al, WO 2011/039638, Topical Tetracycline Compositions, assigned to Foamix. 39. Unpublished results, privy to author. 40. Tamarkin et al, US Patent No. 8,114,385, Oleaginous pharmaceutical and cosmetic foam, assigned to Foamix. 41. Tamarkin et al, US Patent No. 7,704,518, Foamable vehicle and pharmaceutical compositions thereof, assigned to Foamix. 42. Tamarkin et al, WO2008/0299220: Hydrophilic Non-Aqueous Pharmaceutical Carriers And Compositions And Uses, assigned to Foamix. 43. Tamarkin et al, US Patent No. 7,645,803, Saccharide foamable compositions, assigned to Foamix. 44.A Vairale et al, RP HPLC method for the simultaneous quantification of phenoxyethanol and potassium sorbate in topical foam, Intl J Analytical Bioanalytical Chem, 2 2, 151-159 (2012). 45. AZ Abram and RPJ Tomlinson, Mousses, in Handbook of Cosmetic Science and Technology, A Barel et al, eds, pp 221-239 (2001). T H IG R ED 260 AT_Ch9.indd 260 11/14/13 1:07 PM