* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download OB Competency (Word 2003)
Survey
Document related concepts
Transcript
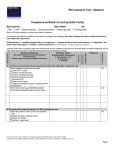
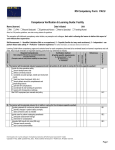
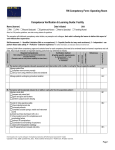
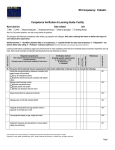
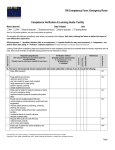
RN Competency Form: Obstetrics Competence Verification & Learning Guide: Facility Name (learner) Date Initiated Unit ☐RN ☐LPN ☐Recent Graduate ☐Experienced Nurse ☐New to Specialty ☐Traveling Nurse Note: for LPN practice guidelines, see state nursing statutes & regulations The preceptor will initial each competency when he/she, as preceptor and colleague, feels safe in allowing the learner to deliver this aspect of care without direct supervision. Self-Assessment: 1 – Identified Limitation (little or no experience); 2 – Capable (familiar but may need assistance); 3 – Independent - can perform these tasks safely; 4 – Proficient - extensive experience *For further information, see instruction sheet at end of this form. IA. The learner will incorporate relevant assessment & intervention (A&I) skills in antepartum care Perform antepartum assessment accurately: check DTR’s / clonus perform non-stress test and perform contraction stress test perform sterile speculum exam auscultate FHR assess uterine activity integrate knowledge of purpose for/expected norms of prenatal labs Perform fetal monitoring per AWHONN standards Complete Intermediate Fetal Monitoring Course IB The learner will incorporate relevant A & I Skills in intrapartum care: Assess labor patient on admit (LPN non-complicated only) identify risk factors (maternal history) collect lab samples performs vaginal exam Learning Guide # Preceptor initials D—Demonstrated; T—Test; M—Module/class; V—Verbalized Learner initials and critical elements. (Preceptor needs to verify learner capability for these items.) Date all met Self-assessment Learning Guide follows competency pages and contains items for each competency that need to be reviewed based on learner’s experience and unit need, they include reminders of important teaching points that may otherwise be missed. Required Competencies Verification method References Main categories followed by associated competencies & facility specific requirements IA 1 IA 2 IB 1 Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 1 References Learning Guide # Preceptor initials D—Demonstrated; T—Test; M—Module/class; V—Verbalized Learner initials Main categories followed by associated competencies and critical elements. (Preceptor needs to verify learner capability for these items.) Verification method & facility specific requirements Date all met Self-assessment RN Competency Form: Obstetrics Required Competencies Assist patient during labor offer comfort measures and coaching during each stage evaluate during each stage ensure emergency equipment standby monitor mom & baby manage changes in fetal well-being assist with placenta delivery monitor patient after placenta delivery Correlate clinical condition with drug indications, desired effects, dosage and contraindications for commonly given medications (IVP RN only) IB 2 Monitor patient and baby receiving anesthesia (local, pudendal, intrathecal, spinal, general) per policy IB 4 Assist with induction/ augmentation of labor per nursing role expectations (RN only) IB 5 Explain role and use of tocolytic meds in pre-term labor patients IB 6 IC. The learner will incorporate relevant A & I skills in OB interventions & complications: Perform amnioinfusion per policy (RN only) IB 3 IC 1 Perform role in assisting with OB procedures per policy IC 2 Provide perioperative care for cesarean section patient prep patient per policy perform L&D role in OR IC 3 Manage care of client with pregnancy complication per protocol IC 4 Provide emergency measures to mom and fetus as needed IC 5 Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 2 ID The learner will incorporate relevant A & I skills in postpartum care: Provide care for post-partum patient identify abnormal findings during complete postpartum assessment respond correctly to abnormal findings in fundus/lochia/ perineal checks teach caregivers per guidelines administer RhoGam, immunizations complete legal documentation Facilitate breast feeding identify community and facility support services identify any maternal problems with breastfeeding identify any infant problems with breastfeeding References Learning Guide # Preceptor initials D—Demonstrated; T—Test; M—Module/class; V—Verbalized Learner initials Main categories followed by associated competencies and critical elements. (Preceptor needs to verify learner capability for these items.) Verification method & facility specific requirements Date all met Self-assessment RN Competency Form: Obstetrics Required Competencies ID 1 ID 2 Provide support to non-breast feeding mothers ID 3 Comments/alternative learning plans: All preceptors are to sign & initial below. Ideally new graduates should have only one to two preceptors for the entire orientation. Preceptor Signature Initials Preceptor Signature Initials Signatures at completion of preceptorship/orientation: Preceptee/orientee Date Primary Preceptor Date Manager Date Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 3 RN Competency Form: Obstetrics LEARNER GUIDE: Reference content in the right-hand column that needs review. IA. The learner will incorporate relevant assessment & intervention (A&I) skills in antepartum care IA 1 . Perform antepartum assessment accurately: Review policies and procedures, required notifications and charting, standing - check DTR’s / clonus orders - perform non-stress test and Review the following: GBS, Rh rubella status, HSV, etc. - perform contraction stress test Review maternal history risk factors - perform sterile speculum exam - auscultate FHR - assess uterine activity - integrate knowledge of purpose for/expected norms of prenatal labs IA 2 Perform fetal monitoring per AWHONN standards Practice with ultrasound and EFM equipment, review manuals/policy - Complete Intermediate Fetal Monitoring Course Review s/s of fetal distress IB. The learner will incorporate relevant A & I Skills in intrapartum care: IB 1 Assess labor patient on admit (LPN non-complicated Review policy, procedure and admission forms only) Review vaginal culture process - identify risk factors (maternal history) - collect lab samples - performs vaginal exam IB 2 Assist patient during labor Review guidelines for laboring patient - offer comfort measures and coaching during each stage Review high risk labor factors and specific interventions to anticipate: - evaluate during each stage hemorrhage, shoulder dystocia, breech delivery, use of vacuum/forceps, etc. - ensure emergency equipment standby - monitor mom & baby - manage changes in fetal well-being - assist with placenta delivery - monitor patient after placenta delivery IB 3 Correlate clinical condition with drug indications, desired Review the following commonly used medications: oxytocin, magnesium effects, dosage and contraindications for commonly sulfate, terbutaline, hemabate, methergine, betamethasone, rhogam, given medications (IVP RN only) ephedrine, procardia, misoprostil, prostin gel and others as applicable IB 4 Monitor patient and baby receiving anesthesia (local, Review procedure, equipment, troubleshooting, anesthesiology role pudendal, intrathecal, spinal, general) per policy Review nurses role for telemetry monitoring of infant IB 5 Assist with induction/ augmentation of labor per nursing Review special precautions with pitocin (set up, safety issues, etc.) and other role expectations (RN only) High risk medications IB 6 Explain role and use of tocolytic meds in pre-term labor Review commonly used tocolytics, policies, expected response patients IC. The learner will incorporate relevant A & I skills in OB interventions & complications: IC 1 Perform amnioinfusion per policy (RN only) Review procedure and patient teaching IC 2 Perform role in assisting with OB procedures per policy Review policy and role of nurse with the following: placement of IUPC, AORM, use of vacuum and forceps, episiotomy, amniocentesis, fetal scalp electrode placement IC 3 Provide perioperative care for cesarean section patient Review pre-op prep procedures and patient/family teaching - prep patient per policy Scrub in to OR with C Section patient or simulate - perform L&D role in OR IC 4 Manage care of client with pregnancy complication per Review the following complications and local policies for caring for patients with protocol them: hyperemesis gravidarum, bleeding, fetal demise, multiple gestation, pre-eclampsia, eclampsia, HELLP syndrome, preterm labor, diabetes, placenta previa/ abruption/ accrete, trauma, malpresentation, substance abuse, PROM, prolapsed cord. IC 5 Provide emergency measures to mom and fetus as Review policies on precipitous childbirth, hemorrhage, fetal distress, etc. needed Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 4 RN Competency Form: Obstetrics LEARNER GUIDE: Reference content in the right-hand column that needs review. ID. The learner will incorporate relevant A & I skills in postpartum care:: ID 1 Provide care for post-partum patient Review all policies and procedures related to postpartum care. - identify abnormal findings during complete postpartum Review postpartum assessment normal findings including physical, assessment psychological, emotional and spiritual aspects - respond correctly to abnormal findings in fundus/lochia/ Review teaching needed: breast & bottle feeding, lactation program, care of perineal checks mom, care of baby - teach caregivers per guidelines Review legal requirements: birth certificate, footprint sheet, ID bands, photo, - administer RhoGam, immunizations etc. - complete legal documentation ID 2 Facilitate breast feeding Review physiology of lactation - identify community and facility support services Review breastfeeding resources. - identify any maternal problems with breastfeeding Review maternal complications: feelings/concerns, mastitis, yeast infections, - identify any infant problems with breastfeeding engorgement, nipple pain, plugged ducts, adequate nutrition/hydration, relaxation. Review s/s letdown Review infant assessment for effective latch, suck/swallow, hunger and satiety cues, bilirubin, positioning, detaching. ID 3 16. Provide support to non-breast feeding mothers Review comfort measures: wrap, ice, NSAIDS, decreasing breast stimulation, pumping breast for support, etc. Other facility specific items to cover: Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 5 RN Competency Form: Obstetrics REQUIREMENTS: All nurses will complete these competencies upon hire. Some competencies may be reviewed annually. This form follows the Competency Outcomes and Performance Assessment (COPA) model. PRECEPTEE/LEARNER INSTRUCTIONS: Complete self-assessment: Rate your skill in each area to identify the areas where you need additional experience, access to teaching resources, and/or lab practice. Discuss your results with your preceptor to help establish a plan and goals for your learning experience and to aid in choosing patient assignments. Scoring per instructions at the top of page 1. PRECEPTOR INSTRUCTIONS: A. Review self-assessment with preceptee/learner to establish plan. B. Required Competencies: The specialty area competency forms are required for independent practice on this unit. This column represents the Alaska Statewide required competencies per ACE-HC and should not be altered. The preceptor will sign each one off when he/she, as preceptor and colleague, feels safe in allowing the preceptee/learner to deliver this aspect of care without direct supervision. C. Verification Method & Agency Specific. Document comments/check marks for the competency and any agency specific requirements. Verification methods include: 1. Demonstration – Preceptor watches learner perform task/procedure in safe, capable manner in a simulated lab or computer setting or as part of direct care performance. The expectation for new graduates is that they demonstrate as many of the competencies as possible. 2. Test – Learner passes a test provided by the facility to measure competence for this skill. (Minimum passing grade indicated. Initial only after test passed.) 3. Module –Learner has completed a training tool (computerized or written module, class, video, etc.) provided by the facility to measure competence for this skill. 4. Verbalization - Learner explains to the preceptor the process and/or planning that evidences safe, reliable knowledge base. This may include case scenarios, discussion, and/or description of plan. NOTE: some competencies may have the verification method specified per facility guidelines (e.g. “test only”) Record N/A and initials only for items that never apply to this learner’s role or performance. D. Sign-off: Sign and date when all elements of the competency are met. If unable to sign off an area due to patient population issues or learner needs more time, document a plan in the comments section at the end of the form. Discuss alternative ways of meeting the requirement(s) as well as any additional time needed with the nurse manager and/or nurse educator. All preceptors assisting in orientation of a new staff member/intern must sign and initial in the signature chart at the end of this document. E. References: Competencies should be met in accordance with these. Add your facility approved references here. F. Learning Guide: These are memory ticklers. The amount of time spent on each of them depends on the learner’s experience. New graduates will likely need time on almost all of the areas listed. REFERENCES COLUMN: List foundational documents to support the learning experience and to use as the official measure by which the competencies are assessed. The ACE-HC group recognizes the following as sources for evidence based practice that can be included in the reference list along with local policies, procedures and forms: Perry & Potter, Elsevier/Mosby, Lippincott, Kozier & Erb, ANA, nationally recognized hospital related regulatory organizations (CLIA, CDC, CMS, JC, etc.), and specialty nursing organizations’ scope, standards and core curricula. This column’s content may be changed to be facility specific. NOTE: ACE-HC competency forms are intended to be used between facilities within Alaska. Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 6