* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Septicemia and Systemic Inflammatory Response Syndrome (SIRS)
Survey
Document related concepts
Transcript
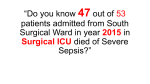
Septicemia and Systemic Inflammatory Response Syndrome (SIRS) Epidemiology The most common cause of mortality in the intensive care unit is septic shock . Even with the best treatment mortality ranges from 15% in patients with sepsis to 40-60% in patients with septic shock. Septic shock develops in about 40% of sepsis patients. Around 750,000 cases of sepsis are diagnosed per year and around 31% of those diagnosed die. The annual health care cost from caring for patients with sepsis is $5-10 billion. Factors contribute to the increasing incidence of sepsis: Widespread us of corticosteroid and immunosuppressive therapies for organ transplants and inflammatory diseases. Aggressive cancer chemotherapy and radiation therapy. Longer lives of patients predisposed to sepsis, the elderly, diabetics, cancer patients, patients with major organ failure, and with granulocytopenia. Increased use of invasive devices such as surgical protheses, inhalation equipment, and intravenous catheters and urinary catheters. Neonates are more likely to develop sepsis. Indiscriminate use of antimicrobial drugs that create conditions of overgrowth, colonization, and subsequent infection by aggressive, antimicrobial-resistant organisms. Microorganisms 1 Although septic shock can be caused by viruses and fungi, most is due to bacterial infections. Common gram-negative bacteria causing septic shock include opportunistic normal flora of the intestines such as Escherichia coli, Klebsiella species, Enterobacter species, and Proteus species. Another opportunistic gram-negative causing septic shock is Pseudomonas aeruginosa. The most common obligate anaerobe to cause sepsis is Bacteroides fragilis. Approximately 45% of the cases of septicemia are due to gram-negative bacteria. Microorganisms 2 Common gram-positive bacteria causing septic shock include Staphylococcus aureus, Streptococcus pneumoniae, Enterococcus species that are normal flora of the intestines, and Streptococcus pyogenes. The most common cause of neonatal sepsis is Group B Streptococcus (GBS). Approximately 45% of the cases of septicemia are due to grampositive bacteria. Approximately 10% of the cases of septicemia are due to fungi, mainly the yeast Candida. The sources for sepsis are infections elsewhere in the body. lung infections: Streptococcus pneumoniae, Haemophilus influenzae, Legionella species, Chlamydia pneumoniae. wound, soft tissue infections: Streptococcus pyogenes, Staphylococcus aureus, Clostridium species, Pseudomonas aeruginosa, anaerobes, coagulase-negative Staphylococcus species. urinary tract infections: Escherichia coli, Klebsiella species, Enterobacter species, Proteus species, Enterococcus species. central nervous system: Streptococcus pneumoniae, Neisseria meningitidis, Listeria monocytogenes, Escherichia coli, Haemophilus influenzae, Pseudomonas aeruginosa, Klebsiella species, Staphylococcus species. Pathogenesis In order to protect against infection, one of the things the body must initially do is detect the presence of microorganisms. The body does this by recognizing molecules unique to microorganisms that are not associated with human cells. These unique molecules are called pathogen-associated molecular patterns. Molecules unique to bacterial cell walls, such as peptidoglycan monomers, teichoic acids, LPS, mycolic acid, formyl peptides, and mannose, bind to pattern-recognition receptors on a variety of defense cells of the body causing them to synthesize and secrete a variety of proteins called cytokines. These cytokines can, in turn promote innate immune defenses such as inflammation, phagocytosis, activation of the complement pathways, and activation of the coagulation pathway. Pathogenesis Cytokines are intercellular regulatory proteins produced by one cell that subsequently bind to other cells in the area and influence their activity in some manner. Cytokines such as tumor necrosis factor-alpha (TNF-alpha), interleukin-1 (IL-1), interleukin-6 (IL-6), and interleukin-8 (IL-8) are known as proinflammatory cytokines because they promote inflammation. Some cytokines, such as IL-8, are also known as chemokines. They promote an inflammatory response by enabling white blood cells to leave the blood vessels and enter the surrounding tissue, by chemotactically attracting these white blood cells to the infection site, and by triggering neutrophils to release killing agents for extracellular killing. In addition to promoting an inflammatory response, these same cytokines activate the complement pathways as well as the coagulation pathway. Pathogenesis Inflammation is the first response to infection and injury and is critical to body defense. Basically, the inflammatory response is an attempt by the body to restore and maintain homeostasis after injury. Most of the body defense elements are located in the blood, and inflammation is the means by which body defense cells and defense chemicals leave the blood and enter the tissue around an injured or infected site. The release of proinflammatory cytokines eventually leads to vasodilation of blood vessels. Vasodilation is a reversible opening of the junctional zones between endothelial cells of the blood vessels and results in increased blood vessel permeability. This enables plasma, the liquid portion of the blood, to enter the surrounding tissue. The plasma contains defense chemicals such as antibody molecules, complement proteins, lysozyme, and defensins. Increased capillary permeability also enables white blood cells to squeeze out of the blood vessels and enter the tissue. As can be seen, inflammation is necessary part of body defense. Excessive or prolonged inflammation can, however, cause harm. Pathogenesis At moderate levels, inflammation, products of the complement pathways, and products of the coagulation pathway are essential to body defense. However, these same processes and products when excessive, can cause considerble harm to the body. Systemic Inflammatory Response Syndrome (SIRS): The Shock Cascade Systemic Inflammatory Response Syndrome (SIRS): During a severe systemic infection, an excessive inflammatory response triggered by overproduction of cytokines such as TNF-alpha, IL-1, IL6, IL-8, and PAF often occurs. This leads to the following sequence of cytokine-induced events: Blood vessels dilate During a severe systemic infection, an excessive inflammatory response triggered by overproduction of cytokines such as TNF-alpha, IL-1, IL-6, IL-8, and PAF often occurs. This leads to the following sequence of cytokine-induced events: Blood vessels dilate and phagocytic WBCs called neutrophils adhere to capillary walls in massive amounts. Chemokines such as IL-8 activate neutrophils causing them to release proteases and toxic oxygen radicals while still in the blood vessels. These are the same toxic chemicals neutrophils use to kill microbes, but now they are dumped onto the vascular endothelial cells to which the neutrophils have adhered. This results in damage to the capillary walls and leakage of blood. Prolonged vasodilation Prolonged vasodilation and increased capillary permeability causes plasma to leave the bloodstream and enter the tissue. Prolonged vasodilation also leads to decreased vascular resistance that, in turn, results in a drop in blood pressure (hypotension) and reduced perfusion of blood through tissues and organs. Damage to the capillaries and prolonged vasodilation result in blood and plasma leaving the bloodstream and entering the tissue. This can lead to a decreased volume of circulating blood (hypovolemia) Activation of the blood coagulation pathway and concurrent downregulation of anticoagulation mechanisms cause clots to form within the blood vessels throughout the body. This is called disseminated intravascular coagulation (DIC). This further limits the perfusion of blood and oxygen through tissues and organs. Damage to the capillaries and prolonged vasodilation result in blood and plasma leaving the bloodstream and entering the tissue. This can lead to a decreased volume of circulating blood (hypovolemia) Disseminated intravascular coagulation Activation of the blood coagulation pathway and concurrent downregulation of anticoagulation mechanisms cause clots to form within the blood vessels throughout the body. This is called disseminated intravascular coagulation (DIC). This further limits the perfusion of blood and oxygen through tissues and organs. Acute respiratory distress syndrome (ARDS) The increased capillary permeability and injury to capillaries in the alveoli of the lungs results in acute inflammation, pulmonary edema, and loss of gas exchange. This is called acute respiratory distress syndrome (ARDS). Liver, kidney, bowel Reduced perfusion and capillary damage in the liver results in impaired liver function and a failure to maintain normal blood glucose levels. Reduced perfusion also leads to kidney and bowel injury. Heart failure The combination of hypotension, hypovolemia, DIC, loss of perfusion, and ARDS, leads to acidosis and decreased cardiac output. Cytokineinduced overproduction of nitric oxide (NO) by cardiac muscle cells leads to heart failure. MSOF and Death Collectively, this cascade of events results in irreversible septic shock, multiple system organ failure (MSOF), and death Symptoms Symptoms of sepsis are usually nonspecific and include fever, chills, and constitutional symptoms of fatigue, malaise, anxiety, or confusion. These symptoms are not limited to infection and may be seen in a variety of noninfectious inflammatory conditions. Symptoms 1. temperature > 38°C or < 36°C 2. heart rate > 90 beats/minute 3. respiration > 20/min or PaCO2 < 32mm Hg 4. leukocyte count > 12,000/mm3, < 4,000/mm3 or > 10% immature (band) cells. Definitions Sepsis was defined as the systemic host response to infection with SIRS plus a documented infection. Severe sepsis was defined as sepsis plus end-organ dysfunction or hypoperfusion. Septic shock was defined as sepsis with hypotension, despite fluid resuscitation, and evidence of inadequate tissue perfusion. While SIRS, sepsis, and septic shock commonly are associated with bacterial infection, bacteremia may not be present. MORTALITY The mortality rate in SIRS has been reported to be about 7%, that in sepsis is about 16-20%, and that in septic shock is about 45% TREATMENT The drugs used depends on the source of the sepsis 1. Community acquired pneumonia a 2 drug regimen is usually utilized. Usually a third (ceftriaxone) or fourth (cefepime) generation cephalosporin is given with an aminoglycoside (usually gentamicin). 2. Nosocomial pneumonia: Cefipime or Imipenem-cilastatin and an aminoglycoside. 3. Abdominal infection: Imipenem-cilastatin or Pipercillin-tazobactam and aminoglycoside. 4. Nosocomial abdominal infection: Imipenem-cilastatin and aminoglycoside or Pipercillintazobactam and Amphotericin B. 5. Skin/soft tissue: Vancomycin and Imipenem-cilastatin or Piperacillin-tazobactam 6. Nosocomial skin/soft tissue: Vancomycin and Cefipime 7. Urinary tract infection: Ciprofloxacin and aminoglycoside 8. Nosocomial urinary tract infection: Vancomycin and Cefipime 9. CNS infection: Vancomycin and third generation cephalosporin or Meropenem 10. Nosocomial CNS infection: Meropenem and Vancomycin