* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Conjugation of Bilirubin
Schmerber v. California wikipedia , lookup
Blood sugar level wikipedia , lookup
Plateletpheresis wikipedia , lookup
Blood donation wikipedia , lookup
Jehovah's Witnesses and blood transfusions wikipedia , lookup
Hemorheology wikipedia , lookup
Hemolytic-uremic syndrome wikipedia , lookup
Men who have sex with men blood donor controversy wikipedia , lookup
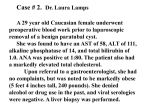
Bilirubin Metabolism & Jaundice Formation of Bilirubin from Heme Heme is degraded in RE system (esp. liver & spleen) 85% from RBCs 15% from turnover of immature RBCs & cytochromes Heme heme oxygenase biliverdin (green) bilirubin (red-orange) bile pigments In Blood with albumin UNCONJUGATED BILIRUBIN (or INDIRECT BILITUBIN) Salicylates & sulfonamides can displace bilirubin from albumin & so bilirubin enters CNS causing neural damage Bilirubin Metabolism in the Liver • Uptake of Bilirubin by hepatocytes: Bilirubin dissociates from its carrier albumin & enters hepatocytes • Conjugation of Bilirubin: In hepatocytes, bilirubin is conjugated with two molecules of glucuronic acid by the enzyme glucuronyl transferase • Excretion of bilirubin into bile: Conjugated bilirubin (bilirubin diglucuronide) is transported into bile canalculi & then into bile. Process is energy dependent & is impaired in liver diseases Bilirubin Metabolism in the Intestine Conjugated bilirubin bacteria in the intestine Urobilinogen Stercobilin in stool (brown) Reabsorbed Kidney Urine Urobilin (yellow) OVERVIEW OF BILIRUBIN METABOLISM Jaundice Yellow color of skin, nail beds & sclera caused by deposition of bilirubin secondary to increased bilirubin levels in blood (hyperbilirubinemia) JAUNDICE IS NOT A DISEASE HOWEVER, IT IS A SIGN OF AN UNDERLYING DISEASE Types of Jaundice 1- Hemolytic Jaundice 2- Obstructive Jaundice 3- Hepatocellular Jaundice Hemolytic Jaundice Massive lysis of RBCs in hemolytic anemia e.g. sickle cell anemia Bilirubin is produced in a rate faster than rate of conjugation by the liver Blood: Increased blood unconjugated (indirect) bilirubin Urine: Urobilinogen is increased No bilirubin in urine (Color of urine is normal) as it is bound to albumin Stool Dark color Increased stercobilin (produced from increased urobilinogen) Obstructive Jaundice In bile duct obstruction: Conjugated bilirubin is prevented from passing to the intestine. Thus, it is regurged to blood increasing conjugated (direct) bilirubin in blood Excessive conjugated bilirubin is excreted in urine giving the yellowish brown color of urine Blood: Increased conjugated (direct) bilirubin GGT & ALP are markedly elevated (ALT is normal or mildly elevated) Urine: Bilirubin appears in urine Thus, color is yellowish brown Urobilinogen is reduced Stool Pale (low stercobilin) Hepatocellular Jaundice First Liver damage (by hepatitis or hepatitis) causes low conjugation efficiency leading to increased unconjugated (indirect) bilirubin in blood Second Conjugated bilirubin is not efficiently secreted into bile. Instead, diffuses to blood increasing conjugated (direct) bilirubin in blood Blood Increased BOTH unconjugated (indirect) & conjugated (direct) bilirubin ALT & AST levels are markedly elevated Urine: Bilirubin is present in urine So, urine color is yellowish brown Stool Pale (low stercobilin) LABORATORY INVESTIGATIONS IN TYPES OF JAUNDICE URINE BLOOD UROBILINOGEN BILIRUBIN UNCONJUGATED BILIRUBIN CONJUGATED BILIRUBIN ALT & AST GGT & ALP NORMAL TRACE NIL N: 0.2 – 1 mg/dl N:0 - 0.2 mg/dl NORMAL NORMAL HEMOLYTIC JAUNDICE INCREASD NIL INCREASED N:0 - 0.2 mg/dl NORMAL NORMAL OBSTRUCT. JAUNDICE Decreased or absent PRESENT N:0 - 0.2 mg/dl INCREASED Normal or mild increase MARKED INCREASE INCREASED MARKED INCREASED HEPATOCEL. JAUNDICE Decreased or absent PRESENT INCREASED Normal or mild increase Jaundice in Newborns • In newborns (especially premature), Bilirubin accumulates as the liver enzyme bilirubin glucuronyl transferase (responsible for conjugation of bilirubin) is low at birth. (The enzymes reaches adult levels in about 4 weeks) • Accordingly, unconjugated bilirubin is increased in blood. Elevated bilirubin in excess of the binding capacity of albumin can diffuse into basal ganglia & cause toxic encephalopathy (kernicterus) • Treatment Exposure of the newborn skin to blue fluorescent light which converts bilirubin to more polar & hence water-soluble isomers These isomers can be excreted into bile without conjugation to glucuronic acid. Congenital hyperbilirubinemia Bilirubin is elevated in blood due to inherited defects in the bilirubin metabolic pathway Crigler-Najjar syndrome Low activity of glucoronyltransferase (conjugating enzyme) Rare Inherited l disease Severe hyperbilirubinemia in neonates (unconjugated bilirubin) Complicated by kernicterus & early death Gilbert`s syndrome Decreased production (expression) of glucoronyltransferase Rare autosomal dominant trait More common men Occurs in 2-3 % of men Usually asymptomatic hyperbilirubinemia Liver function tests are normal Dubin-Johnson syndrome Defect in transfer of conjugated bilirubin into the biliary canalculi Conjugated hyperbilirubinemia.