* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Definition
Survey
Document related concepts
Transcript
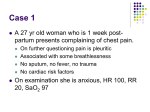
د .ميريانا البيضة Asthma 1 DIAGNOSIS 2 Definition of asthma 3 Definition The guidelines define asthma as: a chronic inflammatory disease of the airways many cells play a role (mast cells, eosinophils, and T lymphocytes) Definition recurrent episodes of: • • • • Wheezing Breathlessness chest tightness Cough particularly at night and/or in the early morning Definition widespread but variable airflow limitation at least partially reversible either spontaneously or with treatment Definition increase in airway hyperresponsiveness to a variety of stimuli Definition • Chronic Inflammation • Bronchial Hyperresponsivenes s • Reversible Airway Obstruction Confirmation of the diagnosis of asthma is based on two key elements: The history or presence of respiratory symptoms consistent with asthma The demonstration of variable expiratory airflow obstruction The variation in expiratory airflow may be demonstrated with measurements made at different points in time The variation in expiratory airflow or in response to administration of anti-asthmatic therapy The diagnosis of asthma can be confirmed using several approaches depending on the patient's clinical presentation and clinical course The 2007 asthma guidelines of the National Asthma Education and Prevention Program (NAEPP) recommend that spirometry, before and after administration of a bronchodilator be performed in all adolescents and adults in whom the diagnosis of asthma is being considered The use of spirometry or bronchoprovocation testing to demonstrate reversible airflow obstruction is particularly important when the patient's symptoms or response to therapy are not typical Use of pulmonary function testing in this manner helps to prevent both over- and under-diagnosis of asthma persons without asthma may have recurrent cough and chest congestion due to repeated bouts of bronchitis, episodic chest heaviness due to gastroesophageal reflux, or chronic cough due to post-nasal drip syndrome In each of these conditions repeatedly normal spirometry or peak flow measurements would help to exclude the diagnosis of asthma. Conversely reversible airflow obstruction in the patient with chronic cough but without other chest symptoms or wheezing on examination could assist in making the correct diagnosis of asthma Diagnosis when initial PFTs are normal Patients with asthma may have normal lung function at the time of evaluation. If the diagnosis is not apparent based on history alone then the following strategies are useful: Repeat evaluation by the clinician when the patient is symptomatic Repeated patient-based measurements of PEFR over time, possibly with a therapeutic trial of bronchodilator Bronchoprovocative testing, such as with a methacholine or exercise challenge Serial measurements of lung function over time As previously noted, asthma is characterized by variable expiratory airflow obstruction. Normal individuals without asthma experience little variability (less than 20 percent) even when respiratory symptoms are present. One useful strategy to diagnose asthma in patients with normal lung function at their medical visit is to provide them with a handheld peak flow meter for home use and ask that they keep a diary of their peak flow recordings, as described previously. The diagnosis of asthma is confirmed by a reliable series of recordings that document more than 20 percent variability in PEFR over time (especially when PEFR reductions are associated with asthmatic symptoms) Similar data collection can take place in the clinician's office by recording PEFR or spirometry at each patient visit. This method is less dependent on the reliability of the patient independently making selfmeasurements, although multiple visits may be required Serial patient-recorded measurements of PEFR over time can be combined with a "therapeutic trial" of a bronchodilator. Significant decreases in PEFR that reverse within minutes of use of an inhaled beta-adrenergic agonist typify asthma. In individuals without asthma the increase in PEFR following bronchodilator administration would be expected to be less than 20 percent Bronchoprovocation Bronchoprovocation testing 33 the diagnosis of asthma can be confirmed with bronchoprovocation testing, usually in the form of methacholine challenge. A provocative stimulus “indirect” “direct” • methacholine and histamine exercise, eucapnic voluntary hyperventilation, cold air hyperventilation, hypertonic saline, mannitol, adenosine monophosphate [AMP] 35 This diagnostic strategy is particularly useful for patients with atypical symptoms such as isolated chronic cough. Standardized protocols for methacholine testing The test consists of performing spirometry at baseline and then after each dose of nebulized methacholine 37 Diagnosis based on history and clinical course In some instances, the diagnosis is clear because of a characteristic history and clinical course. As an example the diagnosis is readily made in a patient who describes repeated episodes over time of typical symptoms triggered by typical stimuli (especially allergic triggers) and responding to antiasthmatic medications. in patients presenting to an urgent care setting or emergency department the diagnosis can be rapidly made when asthmatic symptoms and musical wheezes on auscultation resolve over the course of minutes to hours in response to bronchodilators and glucocorticoids If spirometry is not available, a diagnosis of probable asthma can be made based upon history and response to therapy alone among patients with classic symptoms who respond promptly and completely to therapy. In patients with less typical or persistent symptoms, further evaluation and a more formal approach to diagnosis is indicated Consultation with an asthma specialist, either a pulmonologist or an allergist is warranted when the diagnosis of asthma is uncertain, when the asthma is difficult to control, or when a patient has frequent exacerbations