* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Psychiatric medications in pregnancy and
Epidemiology of metabolic syndrome wikipedia , lookup
Birth control wikipedia , lookup
Breastfeeding wikipedia , lookup
Prenatal development wikipedia , lookup
Women's medicine in antiquity wikipedia , lookup
Prenatal nutrition wikipedia , lookup
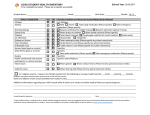
Maternal health wikipedia , lookup
HIV and pregnancy wikipedia , lookup
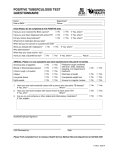
Prenatal testing wikipedia , lookup
Fetal origins hypothesis wikipedia , lookup
Maternal physiological changes in pregnancy wikipedia , lookup
Psychiatric medications in pregnancy and lactation Dr Bavi Vythilingum Division CL Psychiatry, Dept of Psychiatry UCT Rondebosch Medical Centre Psychiatric disorders in pregnancy In SA 30 -40% of women have antenatal depression Decision to treat – benefit to mother vs risk to child More accurate – look at benefit to mother and child vs risk to mother and child “Would a physician tell a pregnant woman with epilepsy, ‘Stop your meds and ride out the seizures until you deliver’? Are the medications of pregnant women with mental illness somehow more “optional”?” Dr Helen Kim, MGH Center for Women’s Mental Health Psychiatric medications in pregnancy and lactation Prescribing principles in pregnancy and lactation Monotherapy Lowest effective dose SSRI’s First line pharmacotherapy Citalopram, sertraline appear best tolerated No long term behavioural effects SSRI and PPHN Six published studies – only three studies adequately powered. 3 studies – increased risk Absolute risk cannot be determined, BUT probably less than 1%. Information does not support discontinuation or lowering the dose of the antidepressant. Antidepressants and teratogenicity Several studies linking SSRI use to – – – Large database studies No face to face interview Multiple confounders – adequate power? Qualitatively different cases vs control – Cardiac defects AHDH Autism Other drug use, higher rates FAS, older No control for effect parenting Tricylic Antidepressants (TCA’s) No increased teratogenic risk More adverse side effect profile – – – particularly postural hypotension constipation lethality in overdose Generally used as second line agents. Other antidepressants Venlafaxine, duloxetine, bupropion – – Less data Probably safe MAOI’s – no data, avoid due to dietary restrictions, risk hypertension Take Home Message Risk of teratogenecity Absolute risk is not clear but appears to be small Psychotherapy treatment of choice for perinatal depression Weigh risk benefit ratio Management of Bipolar Disorder during Pregnancy Should be by a psychiatrist Teratogenic risk – – – – Lithium Ebstein’s anomaly 1-5% (vs 0.5 – 1% risk) Na Valproate NTD, other anomalies, 3x vs other antiepileptics, 4x general population Carbamazepine 1% risk neural tube defects (vs 0.1% risk) Lamotrigine limited evidence, cleft palate Second generation antipsychotics Attractive – – No described teratogenicity Mood stabilisers Metabolic side effects – – – Boden 2012 gestational diabetes adjusted OR, 1.77 [95% CI, 1.04-3.03] Higher risk SGA infant - confounders Medication Summary Lithium – safest Lamotrigine, atypicals – appears safe Individualise for patient Adequate risk counselling Patient falls pregnant on medication DO NOT STOP MEDICATION Minimal decrease in risk of defects vs high risk relapse Continue meds at lowest effective dose Early US and anomaly scan FOLATE Medication through pregnancy Changing maternal blood volumes Increase doses during pregnancy – – Lithium – levels monthly first 2 trimesters, every fortnight thereafter Valproate, CBZ – guided clinically, checking levels every 2 -3 months useful Delivery Liaise closely with obstetrician Hospital Adequate pain control IV line up Stop lithium, benzo’s at onset labour, recommence post delivery after checking level High risk for post natal depression/psychosis Benzodiazepines Small increased risk for cardiac/oral cleft malformations with first-trimester exposure. Neonatal toxicity (“floppy infant syndrome”) /withdrawal Avoid in the first trimester,late in the third trimester Benzodiazepines II To minimize neonatal withdrawal, gradually taper the mother’s benzodiazepine before delivery – – Taper 3 to 4 weeks before the due date and discontinue at least 1 week before delivery. If benzodiazepines cannot be tapered use a short acting agent advise the mother to discontinue benzodiazepine use as soon as she thinks she is going into labour. Medication Generally SSRI’s and TCA’s safe in pregnancy and breastfeeding Antipsychotics – reasonably safe Mood stabilisers – teratogenic risk ECT – option Breastfeeding and Medication MOST WOMEN ON MEDS CAN BREASTFEED!!!!! Risk of child dying from diarrhoea, respiratory disease, malnutrition higher than medication side effects Breastfeeding, bedsharing mothers get more sleep Case by case basis Breastfeeding and Medication Lowest effective maternal dose All meds excreted into breastmilk Watch baby – – Jaundice Excessive sleepiness Pre term – probably best not to breastfeed Breastfeeding and medication II Antidepressants – generally safe Antipsychotics – – Infant sedation Neonatal EPSE Breastfeeding and medication III Mood stabilisers – – Lithium – All present problems Consider risk benefit carefully Maternal hydration important Anticonvulsant class – Rashes Eglonyl? Sulpiride Antipsychotic with theoretical mood elevation properties at low doses Side effect of increasing milk supply Sedating NOT an effective antidepressant Pregnancy and lactation summary All medications present risk – some higher than others Weigh risk benefit ratio PNDSA www.pndsa.org – – 0828820072 [email protected] Otispregnancy.org www.infantrisk.com In general, women do not use psychotropic medications during pregnancy without good reason. They educate themselves, struggle with treatment options, and in many cases stop medication, relapse, and then restart it when they become ill. Being pregnant and giving birth to a child is an exhausting physical and emotional experience. A woman is vulnerable and deserves support, not shaming.