* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Joanie - stjpap 2011
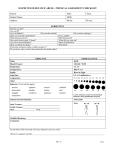
Survey
Document related concepts
Transcript
BEHAVIORAL MEDICINE REVIEW Question 1 Ethics a) Discuss the Tuskegee Experiment. Be sure to answer the following questions in your analysis; b) Who were the subjects? c) How were these subjects recruited? d) What ethical principles were violated in this famous case? e) How might the results of this medical experimentation been different if these patients were asked to sign an “Informed Consent Form” or if the physicians had to submit their research design to an Institutional Review Board? a) The Tuskegee experiment was a U.S. Public Health Service Study that is one of the most horrendous examples of research carried out in disregard of basic ethical principles of conduct. It took place from 1932-1972 and is considered “the longest non-therapeutic experiment on human beings in medical history.” This experiment took away the right of persons to govern self and was one of several experiments that lead to the formation of The National Research Act. The National Research Act’s Fundamental Principles: Protection of those with diminished autonomy Do No harm Maximize possible benefits and minimize harm b) The subjects were 399 poor illiterate Black sharecroppers from rural Alabama who were not aware that they had syphilis or that is was treatable. Instead they were told they had "bad blood" and could receive free medical treatment, rides to the clinic, meals and burial insurance in case of death in return for participating. c) They were recruited via a false premise of free medical care and since almost none of them had ever seen a doctor before they were very pleased to be given this opportunity. The researchers felt that the true nature of the experiment had to be kept from the subjects to ensure their cooperation. d) Violated….LONG ANSWER VERSION…….. The Hippocratic Oath “Do No Harm” and several aspects of the Nuremberg Code 1. The voluntary consent of the individual is absolutely essential 2. The experiment should be such as to yield fruitful results for the good of the society, unprocurable by other methods…..blah..blah… 4. The experiment should be so conducted as to avoid all unnecessary physical and mental suffering and injury. 5. No experiment should be conducted where there is a prior reason to believe that death or disabling injury will occur…….. 6. The degree of risk to be taken should never exceed that determined by the humanitarian importance of the problem to be solved by the experiment 7. Proper preparations should be made and adequate facilities provided to protect the experimental subject against even remote possibilities of injury, disability or even death. 1 9. During the course of the experiment the human subject should be at liberty to bring the experiment to an end if he has reached the physical or mental state where continuation of experiment seems to him to be impossible. 10. During the course of the experiment the scientist in charge should must be prepared to terminate the experiment at any stage, if he has probable to believe ……..blah….blah…..that continuation of experiment is likely to result in injury, disability or death to subj. d)Violated…SHORT ANSWER VERSION…….. The Hippocratic Oath “Do No Harm” and several aspects of the Nuremberg Code. The initial reasons were not inherently wrong and they did not provide “subjects” with proper treatment. They were too interested in studying progress of the disease and too fixated on goal they excluded reasonable judgment . e)The results of this medical experimentation would’ve been extremely different if these patients were asked to sign an “Informed Consent Form” because if informed consent was done with legal capacity prior knowledge, w/o force, fraud, deceit, duress, coercion and w/ sufficient knowledge and comprehension. The subjects would have known the potential consequences of the disease that they had and that it was possible to spread syphilis to their family (partners & children). And taken proper steps to avoid the spread and progression of the disease. Question 2 Child Abuse a) Define the 4 types of child abuse b) What behavioral changes and/or medical indications in a child can suggest sexual abuse? c) Explain the function and role of a “mandated reporter”. d) List some techniques you might use to elicit information from a child without being accused of leading the witness A) The four types of child abuse are as follows: Physical- excessive intentional physical injury to a child or excessive corporal punishment of a child. Torture, beatings, and assault of children are obvious forms of physical abuse. Sexual-includes any activity that uses a child to create sexual gratification either in you or in others. Neglect-failure of caretakers to provide adequate emotional and physical care for a child. Emotional- is a condition in which children do not get adequate attention from their parents or guardians. B) Behavioral changes that would indicate child abuse are discipline problems, trouble sleeping, nightmares, depression, bedwetting, and/or soiling their pants. The child might also refuse to change for gym or participate in physical activities, and they might have inappropriate sexual knowledge. Running away from home is a sign of child abuse for a child less than 14 years old Physical signs of child abuse include difficulty in walking or sitting, a female child that becomes pregnant, or a child that contracts a venereal disease. Parents should know the normal appearance of their child’s genitalia so they can identify any changes which might be the result of child abuse. C) A mandated reporter is any professional who is required by law to report suspected child abuse or cause a report to be made when in their professional roles they have reason to believe that child abuse or maltreatment has taken place. For example physician assistants, police officers, and teachers are considered mandated reporters. 2 D) In order to elicit information from a child without being accused of leading a witness the interviewer should ask open ended questions and then focus them through the interview. The interviewer should be aware of a person in the room that the child looks to for an answer or makes the child uncomfortable. The interviewer should sit at the level of the child, reassure the child that they are trying to help, but does not promise “not to tell”. Finally, the interviewer should not reveal shock or awe at the child’s answers either with verbal or body language. Question 3 Cultural Diversity Healthcare professionals often encounter patients from diverse cultures. Briefly discuss the importance of demonstrating cultural sensitivity when interfacing with patients from other cultures. Be sure to give specific examples explaining how a patient’s religious belief could affect such issues as gender boundaries, diet, fasting regulations, dress, blood transfusions, and death and dying rituals. Some things to keep in mind when interacting with patient’s from various cultural backgrounds are: Gender boundaries: Some Muslim women would like to be seen by a woman clinician, when possible, and when not in an emergency situation. Diet: Muslims eat only Halal food. The following are considered “Haram” or not Halal: Pork meat (i.e. flesh of swine) Blood Animals slaughtered in the name of anyone but Allah (God). There are debates regarding the permissibility of meat slaughtered by Jews (i.e., kosher meat). The meat of donkeys All insects except for the locust (no reference) Alcohol and other intoxicants Jews eat only Kosher food. No pork and shellfish. Fish is acceptable as long as it has fins and scales. All animals with split hooves and which chew the cud (including sheep and cows) Refrain from eating meat and dairy products at the same meal No wine, unless its kosher wine All meat has to be prepared by a qualified kosher butcher (SHOCHET) If meat was eaten in the same day, one must wait six hours before consuming any dairy products Hindus: Most do not eat meat (strict Hindus are vegetarians) and none eat beef since the cow is sacred to. Sikhs do not have many strict rules regarding food but many are vegetarians. Fasting Regulations: Muslims: Fast from sunrise to sunset during Ramadan Jews: Fast two major days of the year: Yom Kippur and Tisha B’Ava. No fasting permitted on Shabbat. Observant Jews fast up to 6 days a year. Hindu: Some Hindus may require special consideration at times of ritual fasting on certain days like Janmashtami or Ram Navami. There are different types of fasting, and generally the following apply: Some Hindus may abstain from water and food through the entire time of fasting. 3 Other Hindus may not eat grains, lentils and beans, but may have milk, fruits, vegetables (usually underground tubors) or nuts. Others may have only milk or fruit through the time of fasting. On some fasting days some Hindus abstain from eating grains. Sikh: does not promote fasting except for medical reasons Dress Code: Muslims: Modest dress. Women wear either a Hijab (head covering) or the Burqa (entire body covered – only eyes showing). Some men do not wear gold jewelry or silk clothing. Jews: Kippah is a slightly-rounded brimless skullcap worn by many Jewish men while praying, eating, reciting blessings, or studying Jewish religious texts, and at all times by some Jewish men. Tzitzit are special knotted "fringes" or "tassels" found on the four corners of the prayer shawl (tallit). Tefillin are two square leather boxes containing biblical verses, attached to the forehead and wound around the left arm by leather straps. They are worn during weekday morning prayer by observant Jewish men. Kittel, a white knee-length over-garment, is worn by prayer leaders and some observant traditional Jews on the High Holidays. Jewish woman dress Modestly. They often wear skirts that go below the knee and wear wigs or hair coverings, so that they do not expose their own hair Hindu: Hindu women have a red dot (bindi) marking and ordthodox Hindu men usually have a religious makring (tilak) on their foreheads. Married Hindu women usually wear a mangalsutra or a specially consecrated gold chain round their necks and will not remove this. Women may insist on keeping their head covered as it is considered an essential element of modesty. Sikh: Sikh Female - The traditional dress of a Sikh is Salwaar Kameez - loose fitting top and bottoms - with a chunni (a large rectangular piece of cloth) to cover the head and draped around the shoulders. This traditional dress is also worn by others from the Indian subcontinent. Therefore the most obvious sign of a Sikh is unshorn hair kept in a bun or platt's, the other being the Kara ( the steel bracelet which forms part of the five K's) worn on the left wrist. Sikh Man - Wear full beard and turban and a Kara on the right wrist. Older Sikhs may wear the traditional Kurta Pyjama - Loose fitting white cotton clothing and carry around a kirpan, which is a weapon, as a symbol of a Sikhs' commitment to protect the weak and to promote justice. Sikh men DO NOT hide the kirpan in their turban. The kirpan is commonly worn in a cloth holster on the right shoulder under ones clothing. Blood Transfusions: Jehovah’s Witness do not accept Blood transfusions Death and Dying Rituals: Muslim: The deceased will be washed respectfully, with clean and scented water, in a manner similar to how Muslims make ablutions for prayer. The body will then be wrapped in sheets of clean, white cloth. There is no embalming. The deceased is laid in the grave (without a coffin if permitted by local law) on his or her right side, facing Mecca. At the gravesite, it is discouraged for people to erect tombstones, elaborate markers, or put flowers or other momentos. Rather, one should humbly remember Allah and His mercy, and pray for the 4 deceased. Loved ones and relatives are to observe a 3-day mourning period. Mourning is observed in Islam by increased devotion, receiving visitors and condolences, and avoiding decorative clothing and jewelry. Jews: After a person dies, the eyes are closed, the body is laid on the floor and covered, and candles are lit next to the body. The body is never left alone until after burial, as a sign of respect. Autopsies in general are discouraged as desecration of the body. They are permitted, however, where it may save a life or where local law requires it. When autopsies must be performed, they should be minimally intrusive. The body must not be cremated. It must be buried in the earth. Coffins are not required, but if they are used, they must have holes drilled in them so the body comes in contact with the earth. The body is not embalmed, and no organs or fluids may be removed. Both the dress of the body and the coffin should be simple. The body is never displayed at funerals; open casket ceremonies are forbidden by Jewish law. From the time of death to the burial, the mourner's sole responsibility is caring for the deceased and preparing for the burial. This period is known as aninut (2-3days) - condolence calls or visits should not be made during this time. The next period of mourning is known as shiva (seven, because it lasts seven days). Shiva begins on the day of burial and continues until the morning of the seventh day after burial. Mirrors in the house are covered. Prayer services are held where the shiva is held. Hindu: After death, Hindus are not buried, but cremated. When a person dies, the body is given a final bath, carried on a wooden stretcher by his kith and kin and cremated on the community cremation grounds generally by the eldest son. Sikh: Cremation is the preferred method of disposal, although if this is not possible any other methods such as burial or submergence at sea are acceptable. Worship of the dead with gravestones, etc. is discouraged, because the body is considered to be only the shell and the person's soul is their real essence. Question 4 Health Disparity Health Disparity can be defined in many ways. I will define it in terms of differences in the presence of a disease to an individual, a person’s outcome, and a person access to medical treatment. Poverty, Medical Insurance, Low education and literacy, and diet can influence health disparity. Poverty is one of the contributors to Health Disparity. A person who is poor will not be able to afford the same treatment as someone who has money. Also a poor person will not be able to seek the best doctors for certain medical condition and this could be detrimental, because certain disease require more special treatment than others. People will lower incomes tend to go to health clinics where it is overcrowded and the clinicians don’t have enough time to proper treat these patient and certain disease might be overlooked or not diagnosed properly. Low education and literacy is the second contributor of Health Disparity. When an individual doesn’t understand their clinician’s language, they are least likely to follow their clinicians guidelines or recommendations. This leads to a worsen medical condition and its overall outcome. These people are not aware of screening tests, and ways reduce their illness and mitigating their risk factors. Educated people and individuals who speak the same language as their provider, have better outcomes in every aspect of health care in comparison to those who don’t. Disease is very complicated subjects with in itself and not understanding the language will just exacerbate its outcome. Diet is the third contributor to health disparity. Low income individual can’t afford to cook gourmet meals. McDonalds, Can foods, TV dinners, and already made frozen foods and other fast foods becomes their major source of food. It is inexpensive and easy to prepare. Geographically, families with low incomes and are minority fall into this category. The problem is these foods lack nutrition and contain high amount of Sodium, low fiber and other chemicals. These factors lead to poor health. Medical Insurance is the last factor in Health Disparity. The type of insurance a person has, affects their treatment to a disease as well as their access to a disease. People with no medical insurance will most likely not receive the proper treatment they need until it too late. Also people with free or inexpensive insurance will not 5 have assess to best health care providers in comparison to someone with more expensive health insurance. Clinics available for inexpensive insurance might not offer update equipment or Name brand prescription medication. Question 5 Death and Dying Death and dying 5) One of the most difficult tasks facing members of the health care team is to assist both the patient and his or her family with a plethora of emotional issues that arise when the patient is facing a terminal illness. Briefly discuss the paradigm developed by Dr. Elizabeth Kubler-Ross delineating the stages that a patient goes through when they are told that they have a terminal illness. Dr. Elizabeth Kubler Ross advocate hospice care for patients who were dying; she was appalled by the way doctors treated terminally ill patients She began giving a series of lectures on terminally ill patients, teaching medical students on how to confront terminally ill patients. She proposed the 5 stages of grief; a pattern of phases, most or all of which people tend to go through, not always in sequence, when faced with the tragedy of their own approaching death or their loved ones: 5 stages of grief- a cycle a person goes through in terms of death and grief; help the patient understand and cope with the reality of the emotional trauma and personal loss. The stages entail emotional, psychological, and spiritual aspects the person experiences. 1.) Shock denial or numbness In this stage the patient is in a conscious or unconscious refusal to accept facts, information, reality, relating to the situation. It's is a perfectly natural defense mechanism. Patient may appear without reaction to the news; they may nod and accept the news without appearing to be troubled by it. To get the news through, they may need to be told several times; it hasn’t sunk into them yet. This is followed by a more external shock, where there may be physical reactions such as paling of the skin, sob and physical freezing. Prior to this the patient goes into denial and pretends that this didn’t occur. Try to be sympathetic and supportive to the patient. Example - "I feel fine."; "This can't be happening, not to me!" 2.) Anger-at physicians, PA’s, medical staff, God Anger can manifest in different ways. People dealing with emotional upset can be angry with themselves, or with others, especially those close to them. They have an out pour of emotions and feelings that were bottled-up. Whoever is in the way is likely to be blamed. The phrase 'Why me?' may be repeated. A part of this anger thus is 'Why not you?’ which fuel their anger at those who are not affected. Let the patient vent even if it’s at you, the PA. Example - "Why me? It's not fair!" "NO! NO! How can this happen!" 3.) Bargaining- in this stage the patient makes promises to God Traditionally the bargaining stage for people facing death can involve attempting to bargain with whatever God the person believes in. People facing less serious trauma can bargain or seek to negotiate a compromise. Bargaining provides a false sense of hope, that there is a solution. Example - "Just let me live to see my children graduate."; "I'll do anything, can't you stretch it out? A few more years." 4.) Depression- loss of personal identity and interest in life 6 This stage is a preparation for death or loss. It shows that the patient has begun to accept the reality. They turn away from any solution and any help that others can give them. Depression may be seen in a number of passive behaviors. In the workplace, this includes physical absenteeism, long lunch breaks and mediocre work performance. It can also appear in tearful and morose episodes where the person's main concern is focused on their own world. They isolate themselves, as a PA show them support and encouragement even though it may seem that they may not want your help, it is likely to be welcomed. Example - "I'm so sad, why bother with anything?"; "I'm going to die . . . What's the point?" 5.) Acceptance The patient has come to a realization and has moved on. The patient will be putting their life in order, sorting out wills and helping others to accept the inevitability. They are usually more stable and content in this stage. They officially gave up. Comfort them throughout this stage and respect their last wishes. Example - "It's going to be OK."; "I can't fight it, I may as well prepare for it." ?/??The stages of death not only represents physical death, but psychological death which is why people (like myself) die every day because of their egos, anger, and selfishness.//?/ http://changingminds.org/disciplines/change_management/kubler_ross/acceptance_stage.htm http://en.wikipedia.org/wiki/Elisabeth_K%C3%BCbler-Ross http://www.businessballs.com/elisabeth_kubler_ross_five_stages_of_grief.htm Question 6 Communication Skills Briefly discuss the ethical, social, and legal concerns involved in using a non-professional translator ie. Family member and/or translator who’s not a skilled medical professional. Cross Cultural Communication: - understand illness from the perspective of the patient - assist patient in understanding disease & treatment from the perspective of biomedicine - help patients & family navigate, express themselves, & feel comfortable w/ large, complex, & often impersonal health care organizations Communication involves exchange, processing & interpretation of messages both verbal & nonverbal. *many opportunities for miscommunications* Language barrier causes an interference with the receipt & relay of info Ex: A Puerto Rican patient who only speaks Spanish says to the Dr. “ataque de nervios”. The Dr. (knowing a little conversational Spanish) thinks he understands the patients’ problem as being a nervous breakdown or perhaps something attacking his nerve fibers”. In reality, the patient is speaking of a very culturally specific syndrome with specific symptoms & precipitants having nothing to do w/ his nerves. Problems w/ untrained people acting as interpreters: 1. Family members- may not give full details b/c they “already know” the patients problems & therefore might omit important symptoms inadvertently. 2. Child/Adolescent- insufficient knowledge of the subtleties in translation, issues of relationships & status 7 Trained interpreters provide more than literal paraphrasing. They interpret patients illness “labels” & idioms, translate biomedical concepts & instructions in patients’ native language. Unfortunately, trained interpreters are underused in primary care settings (probably b/c of financial reasons). This has a negative consequence on patient care. Question 7 Conducing A Psycho-Social History Question 8 Facets of the Healthcare Delivery Team Within the healthcare delivery system, there exists a plethora of professionals who comprise the “psychosocial intervention team”. Briefly explain the role of each of the following professionals and give examples of why you might seek their assistance when dealing with a patient. Psychiatrist – a medical professional who specializes in diagnosing and treating mental disorders. Psychiatrists are one of few people who can prescribe psychiatric drugs, order and interpret electroencephalograms as well as CT scans and MRIs. The major distinction between psychiatrists and other mental health professionals is their medical training. That is why visits to the psychiatrist are noted in the patient’s medical record as opposed to a psychologist, which is not required to be included in the chart. Psychiatrists utilize the biomedical approach to diagnose patients. The biomedical method examines signs and symptoms and compares them with standardized diagnostic criteria. Psychiatric illness can also be assessed through a narrative which tries to understand symptoms as a part of a detailed life history and as responses to external conditions. Both approaches are important in the field of psychiatry. One might need the expertise of a psychiatrist when his/her patient needs to be evaluated for or is suffering from serious mental disorders such as bipolar disorder, Munchausen disorder, schizophrenia, anxiety, psychotic disorders, bulimia or anorexia. A psychiatrist is capable of helping a patient with these kinds of ailments. Psychologist – a mental health professional that is licensed to assess a patient’s mental status and behavior and to conduct psychotherapy. Psychiatrists generally spend shorter periods of contact time with clients/patients, and the principal method of treatment is psychopharmacology. On the other hand, clinical and counseling psychologists generally rely upon psychological assessment and the use of psychotherapy to relieve psychological distress. It is not uncommon for people suffering from mental illness to combine these services to maximize their impact. Many psychologists conduct research-based, standardized cognitive and projective testing to guide the diagnosis of intellectual disabilities, behavioral/mood disorders, and personality disorders. These test results also inform treatment approaches. The services of a psychologist can be called upon to help a patient in emotional distress whether it is regarding post-traumatic stress disorder, domestic abuse, relationship issues, marital problems, emotional disturbances or bereavement. Social worker – social work is a profession committed to the pursuit of social justice, to the enhancement of the quality of life, and to the development of the full potential of each individual, group and community in society. It seeks to simultaneously address and resolve social issues at every level of society and economic status, but especially among the poor and sick. Social workers are concerned with social problems, their causes, their solutions and their human impacts. The main tasks of professional social workers can include case management (linking clients with agencies and programs that will meet their psychosocial needs), medical social work, counseling (psychotherapy), human services management, social welfare policy analysis, community organizing, advocacy, teaching, and social science research. Professional social workers work in a variety of settings, including: non-profit or public social service agencies, grassroots advocacy organizations, hospitals, hospices, community health agencies, schools or faith-based organizations. Physician assistants can refer their patients to social workers for resources regarding housing, food banks, family planning, domestic violence, disability and job placement. 8 Chemical Dependence Counselor – is a licensed mental health professional who often works closely with other specialists, such as psychiatrists, psychologists, clinical social workers to treat individuals with addictions to alcohol or other drugs. A physician assistant can refer their patients who suffer from alcoholism, prescription or illicit drug addicitons. Chaplain/Pastoral Care – a chaplain is typically a priest, pastor, ordained deacon, rabbi, imam or other member of the clergy serving a group of people who are not organized as a mission or church, or who are unable to attend church for various reasons; such as health, confinement, or military or civil duties. Many hospitals and hospices employ chaplains to assist with the spiritual needs of patients, families and staff. A physician assistant can seek the assistance of a chaplain to comfort patients who are terminally or acutely ill as well as their families. Patient Advocate – a patient advocate acts as a liaison between patient and Healthcare Provider. The Patient Advocate is a vital instrument to both patient and physician in the optimal delivery of healthcare. The Patient Advocate often assists with family communication and issues arising from illness and injury. This may include further referral for care and support for both patients and families, which includes ongoing communication and coordination with all practitioners according to each practitioner's preferred protocol. The Patient Advocate has a responsibility to keep a keen awareness for continuity of care, with initial oversight for potentially conflicting treatment modalities and medications, which should be promptly discussed with Patient and Primary Care Provider and all treatments entered into the healthcare record, which should be provided to the patient on an annual basis or more often if the treatment is intensive, prolonged or with several healthcare providers. A Physician Assistant can refer a patient advocate to a patient that is elderly, chronically ill or when english is not their first language. Question 9 The Family As discussed in the lecture related to the role of families in medicine, define and explain the concept of the Therapeutic Triangle and create a scenario demonstrating the effective use of such a concept. The “Therapeutic triangle” is a concept that consists of three “corners”: the doctor (or PA, nurse practitioner, or any other healthcare provider), the patient, and the patient’s family. The concept implies that when all three of the components of the triangle can identify the patient and successfully contribute to treating the patient without difficulty, there is a “positive” triangle, meaning that the triangle is beneficial to the successful treatment of the patient. However, when there is any interference with family’s, patient’s, and practitioner’s ability to identify and treat the patient, negative problems can occur. An example of such interference would be significant family problems, such as an emotional rift between the family and the patient. Another situation with negative impact on the triangle would be a difference in perspectives, such as a battle of wills between what the practitioner believes is best for the patient, and what the patient’s family believes is best for the patient. For example, if a physician says that a patient is mortally in need of a blood transfusion, but the patient is a Jehovah’s Witness and whose faith states that a blood transfusion is against the patient’s religious belief, the patient may refuse the transfusion, and ultimately, the outcome would not be good, at least in the perspective of the practitioner. Question 10 The Family The Family Life Cycle 1.) Independence 2.) Coupling/Marriage 3.) Parenting (New) – adjusting 4.) Parenting (Adolescence) – flexibility of boundaries to allow independence 9 5.) Launching adult children 6.) Senior Retirement – adjusting to new roles Families must continually adapt as members evolve through the various biological and social stages of development. We develop new norms of behavior and redraw new boundaries. As we grow in life and enter young adulthood, we begin to separate from our family emotionally, whether it is going away for college or moving out of the house as our own decision. In this process, we learn how to support ourselves in many ways such as physically, socially, and financially. We then develop our own qualities and characteristics that contribute to our own identity. It is important that we explore our interests and set career goals for ourselves. In doing this we learn to become emotionally and financially independent. During the independent stage, we begin to see ourselves as a separate person from our family. We develop new relationships outside the family and establish ourselves in our work or career. In doing this we develop qualities such as trust, morals, work ethic, and lastly, our identity. After the independent stage, we learn how to commit to a new family and a new way of life. While being in a committed relationship, we learn to adapt to new ways of life. When you enter marriage, you and your spouse have your own view on a family system. Both you and your spouse’s ideas may differ in ideas, expectations, and values. In marriage, you learn to reshape and change your original ideas and create better ones for you and your spouse, and mostly, your family. In this stage, we must learn to achieve interdependence. We must learn how to put someone else’s needs above our own. In this stage, we develop qualities such as communication and problem solving skills. The next stage is parenting. Parenting may be the most challenging stage of the Life Cycle. Parenting can affect our individual development, identity, and marital relationship. When we become parents, we develop three roles. We have the role of being an individual, a spouse, and a parent. Integrating your child into other relationships, including your marriage is a key process. You will take on the role as an individual as well as becoming a decision maker for your family. It is important that you are able to provide a safe, loving, and organized environment for your child to grow. Parenting teenagers can be a difficult time and it may test your skills as a parent. In most teens, new thoughts, beliefs, and styles may cause a conflict in your family. An important skill to have is flexibility in that you will encourage your child to become independent and creative. You will set boundaries and at the same time encourage exploration in your child. Launching adult children begins when your child leaves home with the “empty nest”. In this stage, you are free from the everyday demands of parenting. With this, you are able to rekindle your own marriage and possibly your career goals. In this stage, you should be able to develop adult relationships with your children. You may need to accept new family members into your own family through your child’s relationships or marriage. In this stage, goals to obtain are refocusing on your own marriage without children, developing adult relationships with your children, and realigning relationships to include in laws and grandchildren when your children have begun their own families. Senior retirement is a stage in your life where many changes can occur. You will be welcoming new family members as well as seeing others leaving your family. In this stage, you can choose to have a great adventure and be free of the responsibilities of raising your own children. You may experience a decline in your physical and mental abilities or changes in your financial and social status. In the senior stage, the quality of life depends on how well you have taken care of yourself in the earlier stages. Goals to obtain during the senior stage are maintaining your own interests and physical functioning, exploring new family and social roles, providing emotional support for your adult children, dealing with the loss of a spouse, siblings, and other peers and preparing for your own death, and reviewing your life and reflecting on all you have learned and experienced during the Life Cycle. Question 11 Substance Abuse Define the meaning, and give examples of the following terms frequently used when working with a patient suffereing from a substance abuse disorder: 10 Abuse: self administration of any drug in an illegal/culturally disapproved manner that leads to adverse effects o Example: It is considered abuse when a patient excessively consumes alcohol every night and morning. It is socially acceptable to drink a glass of wine with dinner however if one were to drink packs of beer every night that would be construed as alcohol abuse. Addiction: a cluster of cognitive, behavioral, and psychological Sx that lead to continued use of substance despite substance related problems o Example: Consider a person that is addicted to cigarettes. They have the psychological want to smoke and if they do not have a cigarette they begin to feel stressed and anxious. Dependence: need for substance use to prevent withdrawal o Example: An alcoholic patient needs to drink in order to function normally on an everyday bases and also to avoid tremors, heart palpitations, headaches and any other symptoms of withdrawal. Tolerance: increasing doses of substance required to achieve desired effect o Example: A patient that is abusing pain killers such as morphine or Vicodin will need a higher dosage to alleviate their pain. They have been abusing the pain killers so much that the dosage used for a regular patient does not work for them any more and they need two or three times the regular dose. Withdrawal: physiological and cognitive Sx when blood levels of substance decline o Example: When a patient undergoes alcohol withdrawal, their symptoms are not only psychological but also physical. They begin to experience nausea, vomiting, headaches, tremors of the hands and convulsions. All of which could hinder everyday activities and cause tremendous pain. Question 12 Substance Abuse The CAGE screening test is used in the health hx to screen for alcoholism and try to get the pt to realize that he/she might have a problem. C: A: G: E: Have you ever thought that you should cut down on your drinking? Do you get annoyed when people criticize you on your drinking? Do you feel guilty about your drinking? Have you ever needed a drink first thing in the morning to function or get rid of a hangover? Question 13 Substance Abuse 13 . Addiction Recovery Stages: a. Pre-Contemplation – little thought about the problem b. Contemplation – Pt evaluates their problem/solutions c. Preparation/Determination – baby steps; deciding to stop and have a plan d. Action – actual steps to change; motivated to change e. Maintenance – new life after recovery f. Relapse – prevented by maintenance Question 14 Human Sexuality Human Sexuality: Define and describe the relationship of gender identity, gender roles, and sexual identity in human sexuality. 1. Gender Identity: what they identify themselves as regardless of their biological or genetic sex. 2. Gender Roles: set of behavioral norms, attitudes, values, beliefs, and responsibilities set by society and what 11 that cultural group considers appropriate. It determines such things as clothes each gender wears, activities of each sex, thoughts, and feelings etc. 3. Sexual Identity: sexual orientation - how one thinks of oneself in terms of whom one is sexually attracted to. For example a bigendered person switches b/w being male and female, the butch is the lesbian who wears masculine dress etc Question 15 Human Sexuality Sexual Practices: a. Self-Stimulation and Use of Objects i. Involves no risk of pregnancy ii. Partners should wash their hands/objects before and after using them on their partners or themselves iii. STDs can be transmitted via manual stimulation especially when objects are shared between partners iv. Objects used to penetrate the vaginal or rectum should be clean and non-breakable, with no sharp edges, and should not be shared with others v. Whenever possible cover the object with a new, lubricated condom each time it is used to penetrate the rectum or vagina, if not using a condom wash the object. b. Anal Sex i. Involves no risk of pregnancy ii. Anal sex has the most risk of STDs because insertion of objects can cause tears and bleeding, there is less lubrication. iii. Objects inserted into the rectum should be cleaned before and after anal sex, should not be shared and should be non-breakable, and a lubricated condom should be used each time. iv. If anal penetration precedes oral or vaginal sex, a new condom should be used, or if having unprotected sex, the penis should be washed thoroughly. c. Oral Sex i. Involves no risk of pregnancy ii. STDs can be transmitted via oral-genital contact. iii. If anal sex precedes oral sex, change condom or wash penis before insertion into the mouth. iv. Protected oral sex with a female partner involves latex dental dam, female condom, cut open unlubricated male condom placing it between the mouth and the vulva v. With male partners, cover the penis with unlubricated condom before oral contact is made vi. During oral-anal contact, use a barrier (thin piece of rubber, latex dental dam, cut open unlubricated condom) between the mouth the and the anus to avoid transmission of infection Question 16 Human Sexuality Define the 2 types of sexual harassment and the policy and protocol for addressing sexual harassment in the workplace. 12 Sexual harassment refers to any verbal or physical interaction that is sexual and unwanted, causes you to be uncomfortable, creates a hostile atmosphere or interferes with job performance. 1. Quid-pro-quo “this for that”- supervisor harasses someone, and this results in a concrete employment action, like firing, demotion, or no promotion. 2. Hostile Environment- unwelcome sexually harassing conduct so severe and persistent it affects performance, or creates an intimidating, threatening, or abusive environment. Policy and Protocol 1. Speak directly at the time the harassment occurs: Make it clear you do not like behavior. 2. Collect Evidence: Keep a diary of events; note what is said and done, the dates, times and places. Write down direct quotes, save any letters, cards, notes or materials sent to you. 3. Write a letter to the harasser- behavior may change, the violator may not have known how you saw the behavior, may fear you making a formal complaint 4. Bring a copy of the letter, evidence and formal complaint to supervisor- there are formal complaint procedures in most offices, human resources, etc Question 17 Death and Dying Issues in a Multi-Cultural Hospital Death is a natural process that we all have to go through eventually, and as a health care professional we have to do our best to respect the wishes of different cultures. Hindu: Reading from the Holy Scriptures the Bhagavad Gita, Family may want to call a Hindu Priest (Pandit) to perform holy rites. The pt should be given Ganges water and the tulsi leaf in the mouth by family. The body is washed by family jewellry should NOT BE REMOVED. CREAMITION ASAP except children under 3 should be buried. Jewish: Rabbi to join the dying pt. Dying pt not to be left alone. Jews present should recite th psalsm and at time of death the Decleration of Faith (Shema). Health Care workers should cover the body with a white sheet. Autopsy not done. BURIAL DONE ASAP. The first week is shiva mourners remain at home 30 days shohlism and one yr family. Buddhist: Needs quiet and peace for metation. A monk should be called to talk to pt with passages of the scriptures. Die fully conscious and calm state of mind. Cremation or Burial is premitted. NO special requirements relationg to the care of the body. Christian: Communion, Burial or Cremation permitted, No specific mourning period Muslim: Other family members join and recite verses from Holy Quran, dying pt may wish to face Mecca. The Decleration of Faith (Shahada) Non Muslim health care workes should ask permission to touch body. Body must be covered. Always burial ASAP mouring is three days and also feed the family. Sikhism: Recite from Guru Granth Sahib. Healt Care workers should not remove turbin or trim hair or beard body should be covered with white cloth. The 5 K’s should remain on body. Cremaion ASAP. Afrer a short 13 ceremony at home the body is taken to the gurdwara (temple) for a service and then to a crematorium for further prayers. Up to 10 days passages from the scriptures are read. At the end the eldest son is give a turbin a sign that he is the head of the family. Question 18 Crisis Intervention and Psychotherapy Discuss the meaning of a critical incident, give examples, and discuss effects on the victim and witnesses. Meaning: A critical incident is defined as any event with sufficient impact to produce significant emotional reactions in people at the time of occurrence or later. These events are considered to be outside the range of ordinary human experience, and can lead to post-traumatic stress disorder if the issues caused by the incident are not resolved by the person effectively and quickly. Examples include: Suicide attempts, multiple casualty situations hostage situations, death of child post abusive behavior, verbally or abusive patients, violent death, etc. Effects: Traumatic events affect the psychological functioning and adaptation of victims to the sequellae of the event. Each individual reacts differently depending on age, experience, expectations, interpretations, perceptions of traumatic event. Normal stress reactions would include: feeling upset, repeated disturbing memories, thoughts, or dreams of what happened, difficulty concentrating, trouble falling asleep or sleeping, feeling irritable or having angry outbursts, but it should not last longer than 30 days (normal grief response) Abnormal stress reactions include: Withdrawal, isolation, uncontrollable crying, sadness, depression, intrusive recollection of event, not going to work, lasts longer than 30 days Question 19 Crisis Intervention and Psychotherapy CRISIS INTERVENTION AND PSYCHOTHERAPY What are 10 signs & symptoms of a psychological crisis 1. Withdrawal from social activity 2. Feeling irritable/having angry outbursts 3. Uncontrollable crying 4. Difficulty sleeping 5. Fear/panic 6. Increased alcohol/drug use 7. Poor memory/concentration 8. Increase or loss of appetite 9. Repeated disturbing memories, thoughts, or dreams of the event triggering the psychological crisis 10. Numbness, helplessness Question 20 Crisis Intervention and Psychotherapy Discuss the management of a suicidal patient Suicide management includes: 1. Determine how likely it is the individual will kill him/herself 2. Make sure not to leave individual alone 3. Hospitalization to ensure the patient’s security, supervision and safety of others 14 3 Goals of Hospitalization for Suicidal Patient: a. Secure Patient until Treatment reduced the risk of suicide b. Therapeutically eliminate or improve modifiable suicide Risk factors c. Isolate Patient from toxic environment 4. Management includes the duty to keep patient alive and to treat the underlying condition. Find out why the patient is suicidal. 5. Suicide can be prevented 6. removing any potentially harmful objects 15