* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Adverse Event Assessing, Recording, and Reporting
Survey
Document related concepts
Transcript
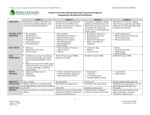
PREP Course #10: Adverse Event Assessing, Recording, and Reporting Presented by: Sharon Hochman CME Disclosure Statement • • • The North Shore LIJ Health System adheres to the ACCME’s new Standards for Commercial Support. Any individuals in a position to control the content of a CME activity, including faculty, planners, and managers, are required to disclose all financial relationships with commercial interests. All identified potential conflicts of interest are thoroughly vetted by the North Shore-LIJ for fair balance and scientific objectivity and to ensure appropriateness of patient care recommendations. Course Director and Course Planner, Kevin Tracey, MD and Tina Chuck, MPH have nothing to disclose. Sharon Hochman has nothing to disclose Objectives • Definitions and terminologies • How to identify and access the safety events • How to record the safety events • How to report the safety events • Case study FDA Safety Reporting: AE & SAE Definitions Adverse Event Serious Adverse Event • An adverse event is any undesirable experience associated with the use of a medical product in a patient • Reported on the source documents, CRFs. • Defined as death; or a life threatening experience; • hospitalization (for a person not already hospitalized); prolongation of hospitalization (for a patient already hospitalized); • persistent or significant disability or incapacity; congenital anomaly and/or birth defects; • or an event that jeopardizes the subject and may require medical or surgical treatment to prevent one of the preceding outcomes. • Reported on the source documents, SAE report What is an adverse event • Any change in the subject health, a new symptom, an accident or new diagnosis after the subject has received a drug or device or during a medical procedure • These are documented for all device or drug trials while subjects on study • They are classified by grade 1-5, or mild, moderate or severe and death. Relationship to the experimental drug or device must be included FDA definitions • FDA regulations use different terms when referring to an adverse event. For example, adverse effect is used in 21 CFR 312.64; adverse experience is used in § 312.32; and unanticipated problems is used in § 312.66. For the purposes of this guidance, the term adverse event is used, except when quoting specific regulations. For device studies, part 812 uses the term unanticipated adverse device effect, which is defined in 21 CFR 812.3(s). FDA Inspection • “Failure to prepare and submit complete and accurate and timely reports of unanticipated adverse device effects” Expected Vs. Unexpected • Expected – Known to Occur and is Listed in the Investigational Brochure, Informed Consent, or General Investigational Plan • Unexpected – Not listed in Investigational Brochure, Informed Consent, or General Investigational Plan – Also not listed in a drug package insert Unanticipated problems • Report as an unexpected problem • Related to participation in research • Placed subject at a greater risk of physical harm than was previously known Examples would be: • A single occurrence of a serious, unexpected event that is uncommon and strongly associated with drug exposure • A single occurrence, or a small number of occurrences, of a serious, unexpected event that is not commonly associated with drug exposure, but uncommon in the study population • An AE that is described or addressed in the investigator’s brochure, protocol, or informed consent documents, but occurs at a specificity or severity that is inconsistent with prior observations. Identifying and assessing safety events • AEs can be directly observed by research staff or reported by research subjects. • If a subject experiences a change in condition during the course of participation, the change may constitute an AE. Changes can take two forms: 1) The appearance of a new symptom or sign or 2) The increased severity or frequency of an existing symptom or sign Examples : Examples of observed AEs include • A rash noted during a physical examination • An abnormal laboratory result • A headache that the subject mentions during a study visit Examples of Adverse Events which are not related to [or caused by] the study drug but if they occur while the subject is on study, would have to be collected, reviewed by PI and tracked: • Transfusion reactions • Accidental injuries • Surgery Attribution • What should the investigator consider prior to assigning attribution? – Individual medical history – Known effects of concomitant medications – Trends in adverse events for their study. Attribution • • • • • Definite – Clearly related to study agent Probable – Likely related to study agent Possible – May be related to study agent Unlikely – Doubtfully related to study agent Unrelated – Clearly not related to study agent • Classifying AE’s •On the Common Terminology Criteria for Adverse Events (CTCAE ) scale, AE’s are assigned a grade based on their severity. •Grade 1- Mild •Grade 2-Moderate •Grade 3-Severe •Grade 4-life threatening or disabling Monitoring studies • Monitoring is done to ensure safety of the subjects in the clinical studies. Separate safety and clinical study conduct monitoring is done. Data Safety Monitoring board (DSMB) • A DSMB is an independent group of people that reviews on a regular basis accumulating data from a clinical study. • They must have no involvement with the conduct of the study DSMB • The DSMB should review each protocol for any major concern prior to implementation. During the trial, the DSMB should review cumulative study data to evaluate safety, study conduct, and scientific validity and integrity of the trial. • There are 3-7 members and one must be a biostatistician. None of them should have direct involvement with the conduct of the study. Most common monitoring findings • not recording ALL AEs regardless of causality or severity to look for trends over time • ignoring reports of minor seemingly unrelated events like stomach aches or dizziness • not having appropriate CRFs to document AE assessments - we always try to suggest using the Common Terminology Criteria for Adverse Events (CTCAE): • not having delegation or appropriate clinician to assess AEs - AE CRFs signed off by coordinators lacking source documentation for assessment of severity or significance • Lab results outside of normal range are often not assessed by clinician • inadequate documentation in the protocol to define AE severity and SAE reporting criteria When do you start communicating about the AE? • AE’s should be captured starting at the baseline visit • PI should always be notified as soon as an AE is identified regardless of the casuality or type. • Discussions should occur with the sponsor and study team . • PI determines need to Update informed consent, or protocol if multiple similar events happen • Patients can be educated to be aware of symptoms that may be associated with an adverse reaction. Subject diary Monitoring tips • • • • • • Reviewing AEs is a priority for monitors All AEs must have source documentation (e.g. clinic note, medical record) It is essential to have the patient’s medical record available for review by the monitor (to make sure none are missed) The monitor can provide advice on completing the AE case report form properly When in doubt, ask your monitor or the sponsor about how to complete the AE Case Report Form The monitor can also connect you with the sponsor’s medical director if requested. Serious & Life-Threat Case Report Forms Completion Participating Sites • Case Report Forms will be completed by the local PI and/or his/her designee at each subject visit. For Multi center studies, Case Report forms will be sent to the Coordinating Center, where they will perform data integrity monitoring through cross-checking and source documentation. GCP CRF Tips • The investigator should ensure the accuracy, completeness, legibility, and timeliness of the data reported to the sponsor in the CRFs and in all required reports (GCP E6 4.9.1). • Data reported on the CRF, that are derived from source documents, should be consistent with the source documents or the discrepancies should be explained (GCP E6 4.9.2). • Any change or correction to a CRF should be dated, initialed, and explained (if necessary) and should not obscure the original entry; this applies to both written and electronic changes or corrections. The investigator should retain records of the changes and corrections (GCP E6 4.9.3). • Ink should be used when completing paper CRFs. Pencil and correction fluid should not be used. Source Documentation • Source Documentation of adverse events include documentation in the medical records of: – Event – Date it occurred – Grade as determined by CTCAE – Expected or Unexpected – Attribution as assigned by PI – Date resolved – Treatment patient received specifically related to event Source Documents The foundation of study data: • Where information was first recorded - Original documents, data, and records to supports subject eligibility, enrollment, and protocol required data • Monitors will need to view Source and compare to completed CRFS and Eligibility determinations Medical records Clinical & office charts X-rays, ECGs, scans Progress notes Labs Rx Notes to file 27 Fundamental Elements of Data Quality A • Attributable – Does the documentation clearly demonstrate who created the record and when,, what happened, and when it occurred? L • Legible – Can the information be easily read and understood? C • Contemporaneous - Was the information documented with timeliness? • Complete – Does the documentation include all of the necessary information? O • Original – Did you maintain the “source” of the information (see GCP Glossary, Sections 1.51 and 1.52)? A • Accurate – Does the information represent what actually happened? Adapted from - FDA - GUIDANCE FOR INDUSTRY - COMPUTERIZED SYSTEMS USED IN CLINICAL TRIALS - ALCOA http//www.fda.gov/downloads/ICECI/EnforcementActions/BioresearchMonitoring/UCM133749.pdf Sample Adverse Event Recording Form The following are required when completing an AE form • Date of onset • Description • Grading • Relatedness • Expected/unexpected • Treatment • Resolution date/outcome Reporting Reporting Serious Events • An investigator must promptly report to the sponsor any adverse effect that may reasonably be regarded as caused by or probably caused by the drug. If the adverse effect is alarming, the investigator shall report the adverse effect immediately. – 21CFR312.64 Reporting Criteria • Routine Reporting – Know which events can be reported at interim analysis or annual reviews • Expedited Reporting – Know which events require immediate reporting Safety Reporting Requirements . This is the responsibility of the sponsor not each investigator • Investigator must immediately report all unanticipated problems and deviations involving risk to subjects or others, serious adverse events related to participation in the study and subject deaths related to participation in the study • Major protocol/consent modifications related to change of safety information Reporting timelines example What Event is Reported When is Event Reported Fatal or life-threatening unexpected, suspected serious adverse reactions Within 7 calendar days of initial receipt of information Non-fatal, non-life-threatening unexpected, suspected serious adverse reactions Within 15 calendar days of initial receipt of information Unanticipated adverse device effects Within 10 working days of investigator first learning of effect Unanticipated Problem that is not an SAE Within 14 days of the investigator becoming aware of the problem All Unanticipated Problems2 Within 30 days of the IRB’s receipt of the report of the UP from the investigator. Reporting Criteria • Know which type of expedited reports each regulatory body requires – FDA – Sponsor – Co-Sponsor – IRB FDA IND Safety Report Criteria Three Criteria: 1. Suspected adverse reaction 2. Serious 3. Unexpected Issues in reporting • Often times, patients are admitted with one diagnosis such as this one. Following admission, secondary events are found. • All of these can be reported using one form Consequences of Improper Reporting • • • • • • Protocol Violations IRB may suspend protocol FDA Hold Sponsor Hold Research Privileges Revoked Patient Safety Multi center trial rules • Sponsors are specifically required to notify all participating investigators (and FDA) in a written IND safety report of “any adverse experience associated with the use of the drug or device that is both serious and unexpected” and “any finding from tests in laboratory animals that suggests a significant risk for human subjects” (§ 312.32(c)(1)(i)(A),(B)). And, more generally, sponsors are required to “keep each participating investigator informed of new observations discovered by or reported to the sponsor on the drug, particularly with respect to adverse effects and safe use” (§ 312.55(b)). Possible Adverse event??? • Phase 2 study of an antihypertensive agent •3/10 subjects develop GERD within a week of starting the drug Take home points… • Record all AEs and report as appropriate and according to guidelines • Report to FDA annual safety reports when applicable • Protocol should include appropriate safety language and reporting criteria and timeframes and safety monitoring process