* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download A Practical Guide for the Use of Nutricia`s MSUD Products f
Low-carbohydrate diet wikipedia , lookup
Diet-induced obesity model wikipedia , lookup
Food politics wikipedia , lookup
Gluten-free diet wikipedia , lookup
Raw feeding wikipedia , lookup
Food choice wikipedia , lookup
Childhood obesity in Australia wikipedia , lookup
Human nutrition wikipedia , lookup
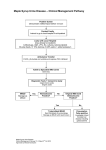
Guidelines for the Nutritional Management of Maple Syrup Urine Disease A Practical Guide for the Use off Nutricia's MSUD Products GUIDELINES FOR THE NUTRITIONAL MANAGEMENT OF MAPLE SYRUP URINE DISEASE A PRACTICAL GUIDE FOR THE USE OF NUTRICIA’S MSUD PRODUCTS Contents Introduction and Background Basic Overview..................................................................04 Diet Principles....................................................................07 Diet Prescription................................................................08 Managing the Diet..............................................................10 Choice of Medical Food.....................................................11 Monitoring.........................................................................13 Illness, Surgery or Injury......................................................14 Case Studies Case Study 1.....................................................................16 Case Study 2.....................................................................18 Case Study 3.....................................................................20 Appendix Product Information Table...................................................22 03 GUIDELINES FOR THE NUTRITIONAL MANAGEMENT OF MAPLE SYRUP URINE DISEASE Introduction and Background Basic Overview Maple syrup urine disease (MSUD) is the common name of the autosomal recessive disorder branched-chain α- Figure 11 Biochemistry: Metabolism of branched-chain amino acids ketoacid dehydrogenase (BCKD) Valine deficiency. The branched-chain amino acids (BCAA): leucine (LEU); isoleucine (ILE) and valine (VAL), Isoleucine Aminotransferase 2-Oxoisovalerate Leucine Aminotransferase 2-OHisovalerate BCKDH 2-Oxo3-methylvalerate Alloisoleucine BCKDH Aminotransferase 2-Oxoisocaproate 2-Oxoisocaproate 2-OH-isocaproate BCKDH whether from exogenous (dietary) or Isobutyryl-CoA endogenous (body protein) sources, 2-Methylbutyryl-CoA IBD Isovaleryl-CoA MBD 3-OH-isovalerate Isovalerylglycine IVD are first deaminated and the resulting branched-chain α-ketoacids (BCKA) are further catabolized by BCKD as Methylacrylyl-CoA Tiglyl-CoA Hydratase Hydratase seen in Fig 1. Deacylase 3-OH-isovalerate 3-Methylcrotonylglycine 3-Methylcrotonyl-CoA MCC 3-Methylglutarate 3-Methylglutaconyl-CoA 2-Methyl3-OH-butyryl-CoA 3-OH-isobutyryl-CoA In MSUD there is an accumulation of Tiglyl-glycine MHBD Hydratase both the BCAA and BCKA. Another BCAA, allo-isoleucine (allo-ILE), normally not detectable, is a distinctive marker in MSUD. A by- DH Methylmalonate semialdehyde product of accumulated ILE has a 3-OH-propionate Methylcitrate 3-OH-3-methylglutaryl-CoA 3-Oxothiolase HMG-CoA lyase DH Propionyl-CoA distinctive odor similar to maple syrup or burnt sugar that can be 2-Methylacetoacetyl-CoA 3.OH-isobutyrate Acetyl-CoA Acetoacetate Carboxylase (PCC) Methylmalonyl-CoA detected in cerumen (as early as 12-24 hours after birth in an untreated newborn with MSUD) and in urine (by 48-72 hours). Mutase (MCM) Succinyl-CoA Krebs cycle A PRACTICAL GUIDE FOR THE USE OF NUTRICIA’S MSUD PRODUCTS The enzyme, BCKD, is a complex of four protein subunits: E1α, E1β, E2 and E3; and disease-causing mutations have been identified in each of these. The resulting phenotypes have been divided into 5 subtypes of MSUD2,3, as seen in Table 1 (overleaf). The classical form of MSUD is the most common and results from mutations in the E1 subunits that cause the BCKD to have less than 3% normal enzyme activity. Without the ability to breakdown the BCAA and the accumulation of intermediates, the clinical signs and symptoms may appear within hours of birth. • Elevated plasma concentrations BCAA, as well as a generalized disturbance of plasma amino acid concentration ratios are present by 12-24 hours of age. • Elevated branched chain α-ketoacids (BCKA) and generalized ketonuria, irritability, and poor feeding by 24-72 hours. • Deepening encephalopathy manifesting as lethargy, intermittent apnea, opisthotonus ( a spasm of extreme hyperextension), and stereotypical movements such as "fencing" and "bicycling" by 4-5 days. • Coma and central respiratory failure that may occur by 7-10 days. Other phenotypes with various degrees of partial enzyme activity include the intermediate, thiamin-responsive, and intermittent forms of MSUD that can experience severe metabolic intoxication and encephalopathy during periods of serious catabolic stress. The fifth type, resulting from mutations in the E3 subunit is a complex disorder that affects not only the activity of BCKD but also α-ketoglutarate and pyruvate dehydrogenase. 1. Zschocke J et al. Vademecum Metabolicum. 3rd ed. Friedrichsdorf, Germany: Milupa GmbH & Co. KG/Schattauer; 2011:60 2. Strauss KA, et al. Maple Syrup Urine Disease in GeneReviewsTM (internet), updated 2009 at http://www.ncbi.nlm.nih.gov/books/NBK1319 3. Nutrition Management Guidelines for Maple Syrup Urine Disease (2013), a collaborative project between Southeastern Region Collaborative (SERC) and Genetic Metabolic Dietitians International (GMDI) see at: www.GMDI.org 05 GUIDELINES FOR THE NUTRITIONAL MANAGEMENT OF MAPLE SYRUP URINE DISEASE Table 1: MSUD Phenotypes2,3 Phenotype Clinical Symptoms (prior to treatment) Biochemical % BCKD activity Classical Neonatal onset, poor feeding, lethargy, altered tone, ketoacidosis, seizures. Symptoms often present prior to learning NBS results. Prenatal testing in at-risk siblings can allow dietary intervention at birth. Nearly all due to mutations in the E1 BCKD subunits ↑↑ allo-ILE, BCAA, BCKA 0-2 Intermediate Failure to thrive, ± ketoacidosis and developmental delay; classical symptoms can occur during catabolic illness/stress ↑ allo-ILE, BCAA, BCKA 3 - 30 Intermittent Normal early development, episodic ataxia/ketoacidosis, severe symptoms may be precipitated by catabolic illness/stress. May be missed by MS/MS NBS Normal BCAA, BCKA when asymptomatic 5 - 20 Thiamin (B1) Similar to intermediate. Often due to responsive mutations in E2 BCKD subunit ↑ allo-ILE, BCAA, BCKA ↓BCKA and/or BCAA with thiamin therapy 2 – 40 Lipamide dehydrogenase deficiency Normal neonatal period, failure to thrive, hypotonia, lactic acidosis, developmental delay, movement disorder. Due to mutations in the E3 BCKD subunit - a component of both pyruvate dehydrogenase and α-ketoglutarate dehydrogenase Moderate BCAA and BCKA, ↑ α-ketoglutarate, pyruvate 0 – 25 A PRACTICAL GUIDE FOR THE USE OF NUTRICIA’S MSUD PRODUCTS Diet Principles3 The BCAA are essential amino acids and must be consumed in the diet as substrates for protein synthesis. Human skeletal muscle is composed of approximately 40% BCAA residues. At times when energy needs exceed energy input, endogenous protein can be broken down and the BCAA become a viable energy source. In MSUD, the ability to use the BCAA as an energy source is inhibited and the BCAA and BCKA accumulate to toxic levels. The BCAA competitively inhibit transport of other large neutral amino acids, and the BCKA affect acid-base balance and neurotransmitter synthesis. The goals of dietary intervention in MSUD are:3 • Rapidly reduce toxic metabolites by restricting dietary BCAA to amounts allowing patients to achieve and maintain appropriate plasma BCAA amino acid concentrations for growth and health maintenance. The goals for plasma BCAA levels are:3 LEU VAL and ILE 50 -200 µM for those ≤5 years of age within or slightly above the normal range for individuals of the same age without MSUD 50 -300 µM for those >5 years of age • Reduce catabolism • Promote anabolism • Monitor nutritional status and alter intake to promote normal growth, development and health maintenance • Evaluate thiamin responsiveness if patient has residual BCKD activity; supplement if responsive 07 GUIDELINES FOR THE NUTRITIONAL MANAGEMENT OF MAPLE SYRUP URINE DISEASE Diet Prescription3 The dietary prescription for individuals with MSUD must be tailored for each patient. It is dependent on such factors as: the amount of residual BCKD activity; age and size; and clinical and nutritional status. Diet calculations for a newly diagnosed infant begin with the recommended intakes (Table 2) of BCAA, protein (PRO), calories (KCAL) and fluids for individuals with MSUD. However, establishing the prescription can be done in the same stepwise manner for all individuals with MSUD. Step 1: Meet the LEU requirement through the use of measured quantities of intact protein from breast milk, regular infant formula, or complete amino acid mixtures (all with known BCAA content per g PRO). Beyond infancy, the LEU requirement is met by foods of known LEU content. Although there are age- and size- specific recommended LEU intakes, the fine tuning of the requirement for a given patient is dictated by plasma LEU levels. Step 2: Calculate the ILE and VAL content of the intact PRO, and add additional ILE and VAL, if needed, to meet the requirement and to adjust plasma BCAA levels. Typically, these supplemental BCAA are prepared as 1% solutions and added to the medical food preparation in 1 mL increments. Step 3: Complete the protein (PRO) requirement by adding the medical food (metabolic formula) that provides a BCAA-free mixture of amino acids (as well as other nutrients). Step 4: Complete the energy requirement by adding non-protein calorie sources as needed. Energy needs should be based on ideal body weight whenever possible. Step 5: Adjust fluid volume and calculate the vitamin, mineral and micronutrient content of the final mixture; adjust or supplement as needed. A PRACTICAL GUIDE FOR THE USE OF NUTRICIA’S MSUD PRODUCTS Table 2: Recommended Daily Intakes for Individuals with MSUD3,4 AGE LEU mg/kg ILE mg/kg VAL mg/kg PROTEIN g/kg ENERGY kcal/kg FLUID mL/kg 0 to 6 mo 40-100 30-90 40-95 2.5-3.5 95-145 125-160 6 to 12 mo 40-75 30-70 30-80 2.5-3.0 80-135 125-145 1-3 yr 40-70 20-70 30-70 1.5-2.5 80-130 115-135 4-8 yr 35-65 20-30 30-50 1.3-2.0 50-120 90-115 9-13 yr 30-60 20-30 25-40 1.2-1.8 40-90 70-90 14-18 yr 15-50 10-30 15-30 1.2-1.8 35-70 40-60 19 yr + 15-50 10-30 15-30 1.1-1.7 35-45 40-50 4. Marriage B. Nutrition Management of Patients with Inherited Disorders of Branched-Chain Amino Acid Metabolism. In: Acosta PB, ed. Nutrition Management of Patients with Inherited Metabolic Disorders. Sudbury, MA: Jones and Bartlett Publishers; 2010:175-236 09 GUIDELINES FOR THE NUTRITIONAL MANAGEMENT OF MAPLE SYRUP URINE DISEASE Managing The Diet3 • Day-to-day diet management by the individual or his/her caregiver nearly always requires the use of a BCAA-free medical food. Only those with the mildest forms of MSUD can meet their PRO requirement and avoid excessive BCAA intake without using medical food. During catabolic illness, even these individuals may need to consume medical food. • Weighing powdered medical foods (and, for infants, regular infant formula as the intact PRO/BCAA source) gives the most accurate and consistent product. Calculations for the amount of intact PRO needed are based on LEU requirements, and are modified by monitoring blood/plasma LEU levels. If additional ILE and/or VAL are required, these should be added at this point. Depending on the individual’s age, water should be added to provide a final volume with a caloric density of 20 to 30 Kcal/fluid ounce. Preparing a 24 hour supply saves time and avoids errors when measuring small quantities. Prepared medical food mixtures should be refrigerated and used within 24 hours. For infants, only an amount anticipated to be finished in one feeding should be placed in a nursing bottle to avoid wastage. The medical food mixture should be consumed throughout the day. Infants should take this mixture at every feeding. • Breast milk, with a mean LEU concentration of 1 mg/mL, is an option as the source of intact protein in infants with MSUD.2 If expressed breast milk is used, this can be added in the appropriate volume to provide the daily required LEU. Some infants with MSUD have been successfully managed by alternating breast feedings with bottle feedings. This requires very careful and frequent monitoring (including plasma BCAA levels and growth) of the infant. Additional support should be given to the lactating mother to ensure that she is consuming adequate and appropriate food and fluids to maintain milk production. • LEU sources for older children and adults come from the intact PRO in foods. Typically, fruits and vegetables are the mainstay of the diet as the PRO: KCAL ratio is low, hence a larger volume of food will not have excessive LEU or other BCAA. Even these low PRO foods must be measured and the amount of PRO or LEU calculated to meet, but not exceed, the LEU requirement. • Modified low PRO foods are another form of medical foods that add KCAL, variety and some normalcy to the diet. The majority of these foods are baked goods and pastas that are prepared from the starch portion of grains rather than the higher PRO flours. • PRO and LEU composition for appropriate foods and medical foods can be found in resources for both patients5.6 and professionals (see references 5-9 page opposite). A PRACTICAL GUIDE FOR THE USE OF NUTRICIA’S MSUD PRODUCTS Choice Of Medical Foods For nearly all individuals with MSUD, BCAA-free medical foods are the cornerstone of the dietary treatment throughout their entire lives. New medical foods for MSUD have been developed over the years to respond to: the differing nutrient requirements of each life stage, and the challenge of patient compliance by offering choices of taste and consistency. For these reasons, Nutricia offers a wide range of products for the individual with MSUD (see Table 3 overleaf). While each product targets a specific patient population, there can be some flexibility and overlap to achieve optimal compliance, or improve access when cost is a limiting factor. In all cases, frequent clinical and biochemical monitoring (see Monitoring - pg 13) is essential. 5. PKU Food List by Virginia Schuett (2010); www.pkunews.org 6. MSUD Foodlist" available at http://genetics.emory.edu/docs/Nutrition%20Docs/MSUDorderform9-29-05.pdf 7. Bowes and Church’s Food Values of Portions Commonly Used. 19th ed. 8. MetabolicPro diet analysis program at www.GMDI.org 9. USDA food composition tables at http://ndb.nal.usda.gov. 11 GUIDELINES FOR THE NUTRITIONAL MANAGEMENT OF MAPLE SYRUP URINE DISEASE Table 3: Nutricia Medical Food Characteristics MSUD Analog® (per 100 g) MSUD Maxamaid®a (per 100 g) MSUD Maxamum®a (per 100 g) MSUD Lophlex LQ®a (per 125 mL) Form powder powder powder ready-to-drink Availability 400 g (14.1 oz) can 454 g (1lb) can 454 g (1lb) can 125 mL (4.2 fl oz) pouches Recommended age 0-12 months Toddlers and young children Older children, and adults including pregnant women ≥ 4 years Added vitamin/mineralb yes yes yesd yes PRO equiv 13 g 25 g 40 g 20 gc CHO 59 g total 12 g simple 47 g complex 56 g total 43 g simple 13 g complex 34 g total 28 g simple 6 g complex 9.3 g total Simple sugars and sweeteners Fat 20.9 g < 0.1 g - 0.44 g Fiber - - - 0.5 g DHA - - - 150 mg KCAL 475 324 305 120 KCAL: PRO 36.5 13 7.6 6 a. MSUD Lophlex LQ is flavored with real fruit juice (from concentrate), MSUD Maxamaid and Maxamum have artificial orange flavoring. b. Vitamin and mineral content appropriate for the recommended age c. Small amounts (< 1.5 mg/100 mL ) of BCAA from added fruit juices d. Appropriate levels for pregnancy if additional folate is given A PRACTICAL GUIDE FOR THE USE OF NUTRICIA’S MSUD PRODUCTS Monitoring2,3 Monitoring is an essential part of MSUD management as frequent adjustments to the diet are necessary to meet nutritional, growth and health maintenance needs while keeping the individual in metabolic control. Important markers for the MSUD monitoring plan are: • Signs and symptoms of catabolic illness: detection of the maple syrup, or burnt sugar, odor in the cerumen and urine occurs when the BCAA accumulate during catabolism. Nausea and vomiting are common. Neurological signs may include cognitive decline, hallucinations, mood swings, choreoathetosis and ataxia. • Growth parameters: head circumference, weight for height and body mass index (BMI) for those over age 2. Care should be taken when interpreting weight for height and BMI as those with both poor linear growth and weight gain may have normal indices. Growth charts can be found at: www.cdc.gov/growthcharts • Urinary ketones, ketoacids: ketones are a sign of catabolism, and α-ketoacids accumulate in the urine when the BCAA are elevated. • Plasma amino acids: analysis of plasma amino acids are necessary to monitor the BCAA and help assess the adequacy of the protein intake • Protein status: in addition to plasma amino acids, albumin, prealbumin (transthyretin) and total protein are markers to follow to assess protein status. When these indicators suggest a need to increase PRO intake, and BCAA are in the treatment range, PRO from medical food can be increased in 10% increments. If the LEU levels are also low, then more intact PRO can be added. • Nutrition status: diet intake analysis for macro- and micronutrients is recommended. When these analyses suggest suboptimal intake, or there are clinical signs of deficiencies, further biochemical analysis for nutrients is warranted. 13 GUIDELINES FOR THE NUTRITIONAL MANAGEMENT OF MAPLE SYRUP URINE DISEASE Illness, Surgery Or Injury2,3 Any illness, injury or surgical procedure is a potential catabolic event that can result in breakdown of body protein stores, release of BCAA and development of ketoacidosis. These events need to be taken seriously as metabolic decompensation can develop quickly and can be life-threatening. The entire metabolic team needs to work with families and individuals to plan for these events. • Initiating the diet in a newly diagnosed infant: if the infant is symptomatic at the time of diagnosis, the coordinated efforts of the intensive care team may be needed to facilitate the rapid removal of excessive BCAA and α-ketoacids, reversal of catabolism, and the use of parenteral nutrition to provide non-BCAA, lipids, glucose, fluids and possibly insulin. Frequent monitoring of both biochemical markers and clinical symptoms is necessary. As soon as possible, small volumes of enteral feeds (medical food) should be introduced. When the levels of ILE and VAL fall to the upper limit of the accepted treatment range, they should be added to facilitate anabolism of LEU (through PRO synthesis). Although hemodialysis may be necessary when BCAA levels are extremely high, it should be accompanied by aggressive nutritional intervention. • Emergency protocol: every patient with MSUD should be provided with a written emergency protocol/letter. This should be not only for the family’s use but to provide guidance to healthcare providers at the onset of illness. The protocol explains MSUD, its treatment, and emergency procedures. It should be individualized for each patient, give appropriate demographic and identifying information about the patient, be updated as necessary and provide contact information for the usual metabolic dietitian and physician. • At home sick-day diet: minor illnesses can often be handled at home with modifications of the usual diet. Patients and families should be in contact with their metabolic team and be aware of the clinical signs and symptoms to monitor. Again, any “sick day” protocol should be updated frequently and individualized for each patient. The typical protocol is to decrease intact PRO by 50-100% for 24-48 hours, increase medical foods to replace the intact PRO, provide additional non-PRO energy sources, and ensure adequate fluid intake. If the patient normally supplements with ILE and/or VAL, this supplementation should continue during this time. • Illness requiring hospitalization: For ill individuals unable to meet their nutrient requirements orally, hospitalization is essential. This includes any individual who has a severe concurrent illness/injury requiring specialized medical intervention. A PRACTICAL GUIDE FOR THE USE OF NUTRICIA’S MSUD PRODUCTS 15 GUIDELINES FOR THE NUTRITIONAL MANAGEMENT OF MAPLE SYRUP URINE DISEASE Case Studies CASE 1: A newly diagnosed infant boy Usage of MSUD Analog (Case report as an example of diet calculation only.) BB is an 18 day old male infant whose diagnosis was made through newborn screening and confirmatory testing. His plasma BCAA amino acids have been brought under control with careful management including parenteral feeds, transition to enteral feeds, and close clinical and biochemical monitoring in a hospital setting. The infant is ready to begin his “home” diet. Mom has a good breast milk supply and wants to use expressed breast milk as the intact protein source. BB currently weighs 3.8 kg and is in the 50th percentile for both height and weight. He has a good suck and seems satisfied on 20 fl oz per 24 hours. As there is a range in the recommendations for the BCAA, energy, and PRO, the initial recommendation will begin with the midpoint of the recommendations and follow with daily plasma amino acid analyses and weight gain to guide adjustments. GOALS (see Table 2 for recommended intakes) LEU: 266 mg ILE: 228 mg VAL: 255 mg Total PRO: 10 g (can be slightly less than the midpoint of recommendations when breast milk is the source of the intact PRO) KCAL: 456 Fluid: 600 mL OTHER DATA for calculations Breast milk MSUD Analog Amount LEU ILE VAL PRO KCAL 1 mL 1 mg 0.58 mg 0.56 mg 0.9% 0.6-0.75 1g 0 0 0 0.13 4.75 A PRACTICAL GUIDE FOR THE USE OF NUTRICIA’S MSUD PRODUCTS Refer back to the steps outlined in the “DIET PRESCRIPTION” section (pg 8). Always begin with meeting the LEU requirement with intact PRO, then calculate the contribution to the total PRO requirement that is to be met by the medical food. Summary of diet prescription AMT LEU ILE VAL PRO KCAL 266 mL 266 mg 154 mg 149 mg 2.85 g 192 MSUD Analog 55 g - - - 7.15 g 261 Non-PRO NA NA NA NA NA NA Supplemental VALa 10.6 mL - - 106 mg - - Supplemental ILEa 7.4 mL - 74 mg - - - Final volume 600 mL TOTAL 600 mL/ 228 mg 255 mg 10.0 g 453 kcal = Breast milk KCAL source 20 fl oz 22 kcal/fl oz a 1% solutions containing 10 mg/mL As BB gets older, his diet needs adjustment to account for growth and development. Regular monitoring is essential. 17 GUIDELINES FOR THE NUTRITIONAL MANAGEMENT OF MAPLE SYRUP URINE DISEASE The choice of medical food depends on, among others, the nutritional needs of the individual, formula access, taste and form preferences. The following case studies are hence used as examples of diet calculations; other Nutricia products may be suitable as well. Refer to product overview (Table 3) and detailed nutrition information tables (Appendix 1). CASE 2: Four year old girl Usage of MSUD Maxamaid (Case report as an example of diet calculation only.) LG is a four year old girl who was diagnosed with MSUD as an infant but has had a series of illnesses (chicken pox, strep throat and otitis media) in the last 18 months that have triggered metabolic decompensation and eventual hospitalization. Her growth has been impacted by these illnesses and she has gone from a robust child in the 50th percentile for height and weight to a present height in the 50th percentile and weight in the 25th percentile (100 cm and 14.5 kg, respectively). She is presently well and her physician has recommended increasing her intake to allow for weight gain. For the past two years, her plasma BCAA levels (when well) have been in the treatment range when her LEU intake, from intact PRO, was 325 mg per day. In addition, she has required 40 mg supplemental ILE per day, but no supplemental VAL. GOALS (see Table 2 for recommended intakes) LEU: 325 mg ILE: approx 200 mg from fooda plus 40 mg supplemental ILE VAL: approx 240 mg from fooda Total PRO: 1.7 x 16 kg (ideal weight) = 29 g Intact PRO: 5.4 ga BCAA-free PRO equiv: 23.6 g KCAL: 70 KCAL x 16 kg (ideal weight) =1120 Fluid: 1400-1600 mL/day a These are approximate calculations based on a mixed and varied diet containing, on average: 60 mg LEU 45 mg VAL 37 mg ILE } per g PRO A PRACTICAL GUIDE FOR THE USE OF NUTRICIA’S MSUD PRODUCTS Refer back to the steps outlined in the “DIET PRESCRIPTION” section (pg 8). Always begin with meeting the LEU requirement with intact PRO, then calculate the contribution to the total PRO requirement to be met by the medical food. Summary of diet prescription AMT LEU ILE VAL PRO KCAL Intact PRO (food) varies 325 mg 200 mg 243 mg 5.4 g ~650 MSUD Maxamaid 94 g - - - 23.6 g 305 Non-PRO KCAL source (Duocal ) 30 g - - - - 137 Supplemental VALa - - - - - Supplemental ILEa 4.0 mL - 40 mg - - - 325 mg 240 mg 243 mg 29 g ~1100 KCAL ® Final volume 720 mL/24 fl oz TOTAL Food+drink 1200 -1600 mL a 1% solutions containing 10 mg/mL Two weeks later, plasma BCAA were in the treatment range but analysis of 3-day diet records showed that LG’s intake from food was far less than the recommended 650 KCAL (although she reached her LEU goal by eating foods with higher LEU content), and she often consumed all of her medical food by 2 PM each day. She showed no weight gain in the interval. LG’s mother was counseled to spread the medical food out so that LG had some with each meal and a last serving in the evening. Because LG seemed to want more fluid during the day, her mother was advised to include a low LEU fruit drink with her snacks. This also provided extra KCAL. Also, guidance was given to include more fat sources in the diet as analysis showed that LG was getting only about 25 % of her KCAL as fat. These recommendations were adopted and in two weeks LG showed a weight gain of 0.6 kg. Because she was utilizing the BCAA for protein synthesis (anabolism), her plasma amino acid analysis indicated that all three BCAA had decreased. LG’s intact PRO allowance was increased by 10% to: 360 mg LEU or 6.0 g PRO. LG’s growth, plasma BCAA and dietary intake were closely monitored over the next two months. She returned to and maintained the 50th percentile for both height and weight. Adjustments were made to keep her BCAA within the treatment range. 19 GUIDELINES FOR THE NUTRITIONAL MANAGEMENT OF MAPLE SYRUP URINE DISEASE CASE 3: A nineteen year old young man Usage of MSUD Maxamum and MSUD Lophlex LQ (Case report as an example of diet calculation only.) AM is a nineteen year old male with MSUD who is a college freshman and living in campus housing. At his last clinic visit, his height was 177 cm and weight 73 kg. He has always done well with maintaining his plasma BCAA in the treatment range and initiating sick day protocols when ill. He has had a good understanding of the diet calculations and often prepared an appropriate meal when his parents were not at home. He found that the college cafeteria’s salad/fruit and dessert bar allowed many choices, and he was able to supplement these with low protein baked goods that he carried in his backpack when necessary. Approximately three nights a week he prepared a pasta meal in the dormitory kitchen. His main problem was his medical food. He had been drinking MSUD Maxamum for the last eight years. However, preparing, storing and carrying the prepared medical food was not convenient for him and many days he consumed as little as 50% of the prescribed amount. He realized that he was losing weight and his most recent plasma amino acid analysis indicated that all the BCAA were elevated. GOALS (diet prescription at the time he left for college) LEU: 550 mg ILE: approx 340 mg from fooda VAL: approx 413 mg from fooda Total PRO: 1.1 g x 73 kg (ideal weight) = 80 g Intact PRO: 9.2 ga BCAA-free PRO equiv: 70.8 g KCAL: 35 x 73 kg (ideal weight) = 2500 Fluid: ~ 3000 mL/day a These are approximate calculations based on a mixed and varied diet containing, on average: 60 mg LEU 45 mg VAL 37 mg ILE } per g PRO A PRACTICAL GUIDE FOR THE USE OF NUTRICIA’S MSUD PRODUCTS Refer back to the steps outlined in the “DIET PRESCRIPTION” section (pg 8). Always begin with meeting the LEU requirement with intact PRO, then calculate the contribution to the total PRO requirement to be met by the medical food. Summary of diet prescription Intact PRO (food) AMT LEU ILE VAL PRO KCAL varies 550 mg 340 mg 413 mg 9.2 g ~1500 Free foods ~450 MSUD Maxamum 177 g - - Supplemental VALa - - - Supplemental ILEa - - - 550 mg 340 mg Final volume - 70.8 g 540 - - - - - 413 mg 80 g 2500 KCAL 1080 mL/ 36 fl oz TOTAL 2-3000 mL Food+drink a 1% solutions containing 10 mg/mL AM tried the ready-to-drink MSUD Lophlex LQ. He recognized that its small volume and individual serving-sized packaging would be convenient for his busy life. His insurance company initially denied coverage for this new product. He was able to appeal their decision with a copy of the product’s nutrition profile (see Table 3 or appendix), and a letter of necessity from his clinic that included information about his weight loss and rise in BCAA when he was unable to consume all of the MSUD Maxamum. AM replaced the MSUD Maxamum with 4 servings of MSUD Lophlex LQ. This provided him with 80 g PRO, 480 KCAL and 500 mL fluid. AM was advised that he would need to drink more BCAA-free fluids (approximately 16 fl oz) to replace what he had been getting in the MSUD Maxamum. AM has found that he can easily do this by mixing one serving of the MSUD Lophlex LQ in a serving of sweetened beverage when he eats in the cafeteria. 21 GUIDELINES FOR THE NUTRITIONAL MANAGEMENT OF MAPLE SYRUP URINE DISEASE Appendix 1 MSUD Analog® Weight, g Energy, kcals Protein Equivalent, g Amino Acids, g L- Alanine L-Arginine L-Aspartic Acid L-Cystine L-Glutamic Acid Glycine L-Histidine L-Isoleucine* L-Leucine* L-Lysine L-Methionine L-Phenylalanine L-Proline L-Serine L-Threonine L-Tryptophan L-Tyrosine L-Valine* L-Carnitine Taurine L-Glutamine Carbohydrate, g Fiber, g Fat, g Saturates, g Monosaturates, g Polyunsaturates,g Ratio n6: n3 fatty acids Linoleic Acid, mg Linolenic Acid, mg DHA, mg Vitamins Vitamin A, IU Vitamin A, mcg RE Vitamin D, IU Vitamin D, mcg Vitamin E, IU Vitamin E, mg alpha TE Vitamin K, mcg Thiamine, mg Riboflavin, mg Vitamin B6, mg Vitamin B12, mcg Niacin, mg Folic Acid, mcg Pantothenic Acid, mg Biotin, mcg Vitamin C, mg Choline, mg Inositol, mg Minerals Calcium, mg Phosphorus, mg Magnesium, mg Iron, mg Zinc, mg Manganese, mg Copper, mcg Iodine, mcg Molybdenum, mcg Chromium, mcg Selenium, mcg Sodium, mg Potassium, mg Chloride, mg 100 475 13 MSUD Maxamaid® 100 324 25 MSUD Maxamum® 100.00 305 40 MSUD Lophlex LQ® 125 mL (4.2 fl oz) 120 20 0.76 1.34 1.11 0.49 1.49 1.19 0.76 None None 1.38 0.32 0.90 1.44 0.89 1 0.40 0.90 None 0.01 0.02 0.10 59 20.9 6.8 9.5 3.6 14.1 3025 230 - 1.48 2.60 2.17 0.96 0.00 2.31 1.49 None None 2.69 0.63 1.75 2.81 1.73 1.94 0.77 1.75 None 0.02 0.14 1.50 56 <0.1 trace trace trace - 2.40 4.10 3.40 1.60 4.60 3.70 2.30 None None 4.20 0.99 2.80 4.50 2.80 3.10 1.30 2.80 None 0.04 0.14 0.32 34 <1 trace trace trace - 1.40 1.90 1.45 1.20 0.00 1.90 1.00 None None 1.78 0.43 1.18 2.38 1.65 1.30 0.53 2.00 None 0.01 0.06 0.00 9.30 0.50 0.44 0.10 0.13 0.21 150 1760 528 340 8.5 4.9 3.3 21 0.5 0.6 0.52 1.25 4.5 38 2.6 26 40 50 100 1665 500 48 12 14.3 9.6 48 0.8 0.8 0.8 2 5 240 3.2 18 62.5 250 56 2228 669 332 8.30 18.3 12.3 82 0.91 0.97 1.6 3.1 5.7 491 4.9 24.5 62 430 80 949 285 320 8.0 4.8 3.2 24.9 0.54 0.50 0.58 1.8 7.1 120 1.8 53.4 17.8 153 40.6 600 500 40 10 8 0.6 450 47 15 15 15 120 420 290 810 810 128 14 11 1.9 1000 144 33 21.5 40 580 840 450 1183 1137 306 14.7 9 1.8 820 131 37 26 58 560 700 560 319 244 96.3 5.1 3.8 0.56 563 56.3 25 10.8 26.8 <25 90 <25 * MSUD Lophlex LQ Juicy Berries may contain traces of leucine, isoleucine and valine from fruit juice (from concentrate) at a level of <1.5 mg/100mL A PRACTICAL GUIDE FOR THE USE OF NUTRICIA’S MSUD PRODUCTS 23 Guidelines for the Nutritional Management of Maple Syrup Urine Disease A Practical Guide for the Use off Nutricia's MSUD Products For more information or product samples, please visit www.nutricia-na.com or call US: (800) 365-7354 Canada: (877) 636-2283 For more tools and resources for the management of your metabolic patients, please visit www.NutriciaLearningCenter.com