* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download David Dinh
Survey
Document related concepts
Transcript
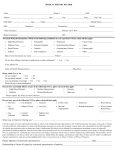
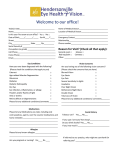
Acute Vogt-Koyanagi-Harada Syndrome in Uveitic Stage Abstract Vogt-Koyanagi-Harada Syndrome is a multi-staged condition characterized by bilateral panuveitis and serous detachments with frequent neurological, auditory, and integumentary associations. This case presents an initial presentation representative of the syndrome’s uveitic stage. Case Report A 33-year-old Hispanic male presented to the clinic with a chief complaint of sudden and progressive decreased vision for one month. Patient reports mild headaches since episode of decreased vision began. His mother, who accompanied him, mentioned that she felt his hearing was slightly decreased compared to normal. His ocular history included recent visits to a retinal specialist who diagnosed bilateral posterior uveitis with macular detachments in each eye, which was being treated with topical corticosteroids (prednisolone acetate) and cycloplegic (cyclopentolate). The patient reported no history of ocular trauma or surgery and non-progressive reduced hearing in both ears since birth. Aside from the recently initiated topical medications, the patient is taking no additional medications. Initial Examination: BCVA: HM OD/OS, PH: 20/400 Pupils: fixed, dilated secondary to topical cyclopentolate SLE: o Iris remnants on the anterior lens capsule suggestive of previous/broken posterior synechiae, o (-) AC cell/flares o All other anterior structures unremarkable IOP: 18 mmHg OD/OS DFE: o 1-2+ Cells in the vitreous o ONH eval: Bilateral edematous nerves with associated disc hemorrhages o Macula: large, 3-4DD serous macular detachments (Figure 1) o Periphery: Non-rhegmatogenous inferior serous retinal detachments Assessment: o Bilateral: Granulomatous panuveitis with associated ONH edema, macular detachments, and retinal detachments. o Differential Dx: VKH, Toxoplasmosis, Cat Scratch Disease, Syphilis, and Lupus. Plan: o Rule out infectious etiologies for ONH edema. Refer for additional blood work and/or cranial imaging. Recommended testing: CBC w/ differential, FTA-ABS/ RPR, ANA, RF, Toxoplasmosis panel, Cat Scratch (Bartonella) panel. Follow-up #1 with retinal specialists – Same Day as Initial Visit: BCVA: HM OD/OS Blood work came back negative for all panels run, suggestive of non-infectious etiology Assessment: Atypical, non-infectious panuveitis. Suggestive of VKH. Plan: Initiate systemic corticosteroid therapy with continued topical corticosteroid and cyclopentolate Follow-up #2 with retinal specialists – 1 week later: BCVA: HM OD/OS Mild improvement in vitritis OS Assessment: Assumed Vogt-Koyanagi-Harada based on history and presentation. Plan: Continue current treatment. Follow-up #3 with retinal specialists – 3 weeks later: BCVA: 20/400 OD, 20/200 OS Continued improvement in vitritis, OS Plan: Continue current treatment. Follow-up #4 with initial OD – 4 weeks later: BCVA: 20/100 OD, 20/80 OS Residual trace cells in the vitreous, OU DFE: Bilateral serous macular detachments per OCT, improved; ONH edema OU w/ resolution of disc hemes, improved Plan: Coordinate with retinal specialists to begin slow taper of systemic corticosteroid, continue topical steroid and cycloplegic. Patient is in active follow-up. Resolution is still ongoing. Discussion: Vogt-Koyanagi-Harada Disease is an idiopathic chronic, bilateral, granulomatous inflammatory condition with multi-systemic associations. It has a strong association with darkly pigmented individuals with a strong prevalence among Far East Asians, Hispanics, and African Americans. There is a greater predilection among females and tends to occur between the 2nd and 4th decade, though pediatric and geriatric cases have been reported. Based on new criteria, it can be broadly grouped into three groups based on clinical features1: o Probable These patients have a lack of any significant ocular trauma or surgery preceding the initial uveitic event, no evidence of other ocular disease via clinical and laboratory testing Bilateral involvement o Incomplete The above findings plus either neurologic/auditory findings OR integumentary findings o Complete The above findings with both neurologic/auditory AND integumentary findings Additionally, the stage of diagnosis can vary the clinical manifestations observable2: o Prodromal Stage -- Short duration (3-5 days) with extraocular symptoms such as headaches, tinnitus, difficulty hearing, and/or neck stiffness. o Uveitic Phase – Longer duration (several weeks). Bilateral granulomatous uveitis with serous retinal detachments (SRD). Optic nerve swelling can be present with prevalence ranging from 27% to 87% with associations favoring older age, concurrent systemic vasculopathies, and optic nerve disc size2,3. o Convalescent Phase – Variable duration (months to years) with depigmentary changes: retinal changes observed as a “sunset glow” retina or choroidal depigmentation, perilimbal vitiligo, alopecia, and/or poliosis of the hairs of the head and eyes. o Chronic Recurrent Phase – Acute recurrent episodes of anterior uveitis. Other complications include choroidal neovascularization, glaucoma, and cataracts. VA at presentation can vary wildly but is associated with the level of ONH swelling, extent of macular detachments, and duration of the acute inflammation. VA recovery may be predicted based on OCT analysis after analyzing the extent of the macular detachments and subsequent reattachment with the level of disruption between the inner and outer cone/rod segments4. Ancillary Testing: OCT – aids in quantifying and visualizing extent of retinal detachment. Useful in monitoring for progression and efficacy of treatment regimens. Fluorescein Angiography – used to check for classic pinpoint leakages throughout the retina in early stages as well to check for the presence of any choroidal neovascularization in the later stages mfERG(acute stage)/ffERG (chronic phase) – can be used to baseline macular function at diagnosis and track efficacy of treatment based on improvement in testing. VA can be directly attributed to mfERG abnormalities. Blood Work – helps to rule out infectious etiologies that may mimic this similar presentation. Treatment and Management: First Line: High-dose oral corticosteroids to help control the acute panuveitis. Adjunct topical cycloplegics and corticosteroids are also useful to quell any anterior chamber reaction as well as attempts to prevent posterior synechiae formation. With all treatments, a slow taper –typically over several months – is indicated to help reduce the chance of rebound or recurrent uveitis5. For patients with signs of resistance with steroid therapy, immunosuppressive agents (Cyclosporin A) are a necessary adjunct with corticosteroids to help achieve best recovered vision5,6. Intravitreal bevacizumab has been shown to be effective in a single patient with persistent serous detachment secondary to VKH. Further research is warranted but results showed promise for a concomitant approach with intravitreal bevacizumab and systemic steroids for early recovery and minimization of risk of permanent visual impairment6,7. Once the acute inflammatory phase is over, visual field testing may be useful to monitor for any lasting NFL defects secondary to optic nerve swelling. Continued monitoring for cataract formation, glaucoma, subretinal neovascularization, and recurrent events is highly recommended as these patients have a high predilection for early acquisition of these conditions. Conclusion Accurate diagnosis and prompt, aggressive treatment is the patient’s best opportunity to regain best vision. Despite optimum therapy, the patient is at continued risk for a host of ocular complications related to the disease and therapy. Patient education is key to ensure continued follow-up care. Bibliography 1. Read RW et al., Revised Diagnostic Criteria for Vogt-Koyanagi-Harada Disease: Report of an International Committee on Nomenclature. American Journal of Ophthalmology. 2012. 131(5):647-652. 2. Pan D, Hirose T. Vogt-Koyanagi-Harada Syndrome: Review of Clinical Features. Seminars in Ophthalmology. 2011. 26(3-4):312-315. 3. Nakao K, Abematsu N, Mizushima Y, Sakamoto T. Optic Disc Swelling in Vogt-Koyanagi-Harada Disease. Investigative ophthalmology & Visual Science. 2012. 55(4): 1917-1922. 4. Zhao C et al., Spectral Domain Optical Coherence Tomography of Vogt-Koyanagi-Harada Disease: Novel Findings and New Insights into the Pathogenesis. Journal of Chinese Medical Science. 2012. 27(1):29-34. 5. Bordaberry MF. Vogt-Koyanagi-Hara disease; diagnosis and treatments update. Current Opinion in Ophthalmology. 2010. 21:430-435. 6. Nussenblatt RB. Vogt-Koyanagi-Harada syndrome . In Nussenblatt RB, Whitcup SM (eds) Uveitis Fundamentals in Clinical Practice, 3rd Ed. pp. 324-328. 7. Park HS, Nam KY, Kim JY. Intravitreal bevacizumab injection for persistent serous retinal detachment associated with Vogt-Koyanagi-Harada disease. Archive of Clinical Experimental Ophthalmology. 2011. 249:133-136.