* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Handout to Beta blocker therapy in heart failure in the elderly
Survey
Document related concepts
Transcript
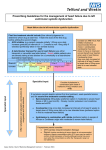
Target dose vs highest tolerated dose: Beta blocker therapy in heart failure in the elderly https://www.newscientist.com Jasmine Peterson, PharmD PGY-2 Ambulatory Care Resident CommUnityCare Clinic University of Texas College of Pharmacy at Austin October 7, 2016 Objectives: 1. Understand the epidemiology and pathophysiology of heart failure 2. Describe the challenges of managing heart failure in elderly patients 3. Summarize the literature regarding the controversy behind achieving target doses of beta blockers in elderly heart failure patients Peterson, Page 1 of 20 I. Definition of elderly27 A. A consensus definition of elderly does not exist i. No general agreement on the age at which a person becomes old ii. May vary in underdeveloped countries B. According to the World Health Organization (WHO), most developed countries have accepted the chronological age of ≥65 years as a definition of elderly II. Heart Failure (HF)1-4 A. Background a. Defined as a complex clinical syndrome in which the heart has an inability to properly fill with and eject blood to the rest of the body b. HF may result from disorders of the pericardium, myocardium, endocardium, or heart valves B. Definitions/Types1-4 a. HF with reduced ejection fraction (HFrEF) i. Also referred to as systolic dysfunction ii. Occurs as a result of dilated left ventricle leading to its inability to pump oxygen rich blood to the rest of the body iii. Defined as left ventricular ejection fraction (LVEF) ≤40% iv. Randomized controlled trials have demonstrated efficacious therapies in this patient population v. Coronary artery disease (CAD) is the most common cause although many other risk factors may lead to systolic dysfunction b. HF with preserved ejection fraction (HFpEF) i. Also referred to as diastolic dysfunction ii. Occurs when the left ventricle loses its ability to relax properly therefore leading to impaired ventricular filling iii. Defined as LVEF ≥50% (however further research is needed to characterize these patients) 1. Other definitions a. HFpEF borderline (LVEF 41-48%) b. HFpEF improved (LVEF >40%) i. Patients with HFpEF who previously had HFrEF c. Patient characteristics, treatments, and outcomes are similar to those of HFpEF iv. Currently, efficacious therapies have not shown proven mortality benefit v. Hypertension (HTN) remains the most common cause of HFpEF vi. These patients are mainly treated for underlying risk factors and comorbidities similar to guideline directed medical therapy (GDMT) use in patients with HFrEF Peterson, Page 2 of 20 C. Classifications 1 Table 1. ACCF/AHA NYHA A At high risk for HF but without structural heart disease or symptoms of HF None B Structural heart disease but without signs and symptoms of HF I No limitation on physical activity C Structural heart disease but with prior or current symptoms of HF I No limitation on physical activity II Slight limitation of physical activity III Marked limitation of physical activity IV Unable to carry on any physical activity without symptoms of HF IV Unable to carry on any physical activity without symptoms of HF D Refractory HF requiring specialized interventions American Heart Association (AHA); American College of Cardiology Foundation (ACCF) ; New York Heart Association(NYHA) D. Epidemiology 1,3,4 a. Prevalence i. The lifetime risk of developing HF is 20% for patients ≥40yo ii. In the US, the incidence is >650,000 new HF cases each year iii. Large percentage of patients suffering from HF are elderly with both incidence and prevalence increasing Figure 1. Darish Mozaffarian et al. Circulation.2016;133:e133:e38-e360 Percentage Prevalence of HF by sex and age (National Health and Nutrition Examination Survey 2009-2012) 16 14 12 10 8 6 4 2 0 13.5 10.6 6.6 Male 4.8 0.2 0.6 20-39 Female 1.5 1.2 40-59 60-79 Age (years) 80+ Peterson, Page 3 of 20 iv. Factors contributing to the rise and incidence of HF 8-11,18 1. Age- related cardiovascular changes a. Reduced responsiveness to Beta-adrenergic stimulation b. Increased vascular stiffness 2. High prevalence of cardiovascular disease 3. Improved therapy for coronary heart disease a. With pharmacologic therapies more patients survive to eventually develop HF b. Mortality i. Absolute mortality rates of HF are about 50% within 5 years of diagnosis 1. Increase exponentially with advancing age c. Hospitalizations i. 75% occur in patients >65yo ii. HF is the primary diagnosis in more than 1 million hospitalizations per year iii. In the US, the total cost of HF care is over $30 billion annually B. Pathophysiology (Appendix A)1,3,4 a. Initially: i. Myocardial injury produces an initial decline in the heart's pumping capacity which leads to the activation of compensatory mechanisms (renin angiotensin aldosterone system (RAAS), sympathetic nervous system (SNS), and natriuretic peptide system (NPS)) to restore cardiovascular function and prevent further damage ii. During this time the patient usually remains asymptomatic b. Over time: i. The sustained activation of these systems leads to worsening left ventricular remodeling, sustained impaired pumping capacity, and inadequate renal perfusion. ii. Poor renal perfusion triggers sodium and water retention which leads to congestive signs and symptoms often associated with HF C. Clinical Presentation 1,3,84,8-11 a. The cardinal symptoms of HF include: i. Dyspnea ii. Fatigue iii. Exercise intolerance D. Risk Factors 1,3,4 a. Common etiologies of HF in the elderly i. Coronary artery disease (CAD) ii. Uncontrolled chronic disease (i.e. HTN) iii. Valvular heart disease iv. Cardiomyopathy 1. Cardiotoxins (i.e. Alcohol, anthracyclines) v. Myocarditis vi. Pericardial disease vii. Age-related cardiovascular changes E. Challenges of managing HF in the elderly 8-10,26 Peterson, Page 4 of 20 a. Physiological age-related changes i. Influence drug pharmacokinetics and dynamics b. More complex comorbidities (i.e. HTN, atrial fibrillation, peripheral vascular disease, CAD, valvular disease, renal dysfunction) i. Higher risk for drug-related side effects ii. Polypharmacy c. Social issues i. Limited access to caregivers and specialists ii. Cognitive impairment iii. Financial problems affect therapy adherence 1. Low functional status, low body weight, frailty, cognitive impairment, and dementia all of which are associated with worse clinical outcomes F. Guidelines (Appendix B) 1,2 a. 2013 ACCF/AHA guideline for the management of HF b. 2016 ACC/AHA/HFSA focused update on new pharmacological therapy for HF: an update of the 2013 ACCF/AHA guideline G. Management 1-3,5 a. Non- Pharmacologic i. Patient education ii. Restrict sodium intake (1.5- 2 gram/day) iii. Weight control iv. Manage/control underlying causes v. Intensive follow-up vi. Smoking cessation vii. Restrict alcohol H. Pharmacologic Therapies i. Stage A 1. Goals: Prevent structural heart damage and promote heart healthy lifestyle a. Angiotensin Converting Enzyme Inhibitor (ACEI)/Angiotensin Receptor Blocker (ARB) in patients with vascular disease or diabetes ii. Stage B 1. Goals: Prevent HF symptoms and further cardiac remodeling a. ACEI/ARB and beta blockers as appropriate iii. Stage C (HFrEF) 1. Goals: control symptoms, prevent morbidity and mortality, and slow progression of worsening cardiac function a. Diuretics, ACEI/ARB, Angiotensin Receptor Neprilysin Inhibitor (ARNI), beta blockers (BBs), aldosterone antagonists, hydralazine/isosorbide dinitrate, digoxin, ivabradine iv. Stage D 1. Goals: control symptoms, improve quality of life (QOL), reduce hospital admissions, establish end-of-life goals Peterson, Page 5 of 20 a. Advanced care measures, heart transplant, chronic inotropes, implantable cardiac device, palliative care III. Review of BBs A. Background a. First multicenter randomized trial was published in 1993 b. Slow acceptance related to negative inotropic effect and risk of decompensation in HF patients B. Proposed mechanism of action/beneficial effects in HF a. Antagonize the SNS reduce harmful effects of continuous expression of neurohormones (i.e. norepinephrine) on the heart b. Reduce HR, blood pressure, and potential for arrhythmias C. Pharmacology (Appendix C) 7,8,21 a. Onset, absorption, metabolism, excretion, contraindications, drug interactions, dosing, etc. D. Safety 6, 16,17 a. Generally well tolerated b. Refer to Appendix C for common adverse reactions and contraindications IV. Current recommendations regarding BB use in HF 1,2 A. The 2013 ACCF/AHA guideline states: i. “Use of 1 of the 3 beta blockers proven to reduce mortality (i.e. bisoprolol, carvedilol, and sustained-release metoprolol succinate) is recommended for all patients with current or prior symptoms of HFrEF, unless contraindicated, to reduce morbidity and mortality.” (Class I, Level of evidence A) 1. Class I: Recommendation that treatment is effective/beneficial 2. Level of evidence A: Data derived from multiple randomized controlled trials (RCTs) a. Refer to Appendix D ii. “Clinicians should make every effort to achieve the target doses of the beta blockers shown to be effective in major clinical trials.” V. BB use in the elderly19-21,24,25 A. Mostly underrepresented in large randomized controlled trials (RCTs) where therapeutic agents have demonstrated clinical efficacy i. Refer to Appendix D B. Previous studies and surveys have demonstrated that the underuse of BBs are evident in the elderly mostly due to: i. More comorbidities, less frequently referred to cardiologist for optimal management, and less tolerance to medications VI. Evidence evaluating titrations of BB to target doses in elderly HF patients A. CIBIS-ELD trial i. Objective: This was a randomized, double blind trial with the primary endpoint tolerability of BBs when used at recommended target doses 1. Bisoprolol (10mg daily) vs carvediolol (25mg BID) ii. Inclusion criteria: 1. ≥65yo LVEF ≤45% and NYHA class II, BB naive or on <25% of the recommended target dose Peterson, Page 6 of 20 iii. Results: 1. 75.7% of the subjects with mean age 72.8 years did not reach the primary endpoint a. Bisoprolol 24% vs carvedilol 25% 2. No significant difference between the two groups in the incidence of worsening HF, hospital admission, hypotension, and mortality 3. Older age and NYHA class III-IV were associated with not achieving target dose 4. Significant differences in adverse events included: bradycardia (bisoprolol) and pulmonary events (carvedilol) iv. This trial demonstrated that up-titration of BBs in the elderly is difficult v. Short follow-up therefore unable to determine correlation between tolerability to the target dose and mortality VII. Evidence evaluating effect of BBs on mortality in elderly HF patients A. Meta-analysis27 i. Evaluated all-cause mortality data involving elderly and non-elderly chronic HF patients from 5 completed BB clinical trials 1. Revealed no statistically significant difference in mortality reduction between elderly and non-elderly HF patients 2. Trials evaluated in this analysis included 12,729 patients with HF; only 4,617 patients (36.3%) were classified as elderly a. Mean age <65 yrs old b. 2 trials excluded patients >80yo c. Percentage of patients >70yo was not reported in 2 trials d. See Appendix E B. Further studies are needed to determine whether elderly HF patients benefit clinically from uptitration to the maximal tolerated dose of BBs VIII. THE BIG CLINICAL QUESTION!!!!!: Is achieving target doses of BBs in elderly patients with HF associated with better clinical outcomes? Peterson, Page 7 of 20 IX. Literature Review: Table 7. Sin D., McAlister F., et al. The effects of beta-blockers on morbidity and mortality in a population-based cohort of 11,942 elderly patients with heart failure. Am J Med. 2002;113:650–656 Purpose Study Design Inclusion criteria Exclusion criteria Outcomes Methods Statistics Results Author’s Conclusions Evaluate the associations between BBs and outcomes in older HF patients Retrospective cohort study All residents of Alberta, Canada ≥ 65 years old who had at least 1 hospitalization for HF between 1994 and 1999 Patients who died during the index hospitalization Patients who had been hospitalized for HF in the 2 years before the index hospitalization All-cause mortality HF hospitalization Followed patients from the date of their index hospitalization until the date of their death, first rehospitalization for HF, or December 31, 1999, whichever came first Obtained prescription information through Alberta Blue Cross program Divided the daily dose of BBs into 3 categories: o Not dispensed, lower dose (<50% of target dose) , and higher dose (≥50% of target dose) Sensitivity analysis: o Examined effects of BB therapy in the youngest and healthiest subgroup (65-74 yo with no documented comorbid conditions) Continuous variables Tukey test Ordinal and dichotomous variables chi-squared test Cox proportional hazards model Kaplan-Meier analyses Sensitivity analysis to minimize effects of confounding variables P value <0.05 = statistical significance Male (~50%) +80 years old (58%) Of 11,942 patients of whom 2569 (22%) had Charlson comorbidity scores of at least 2 Median follow-up was 21 months 1162 patients (10%) received BB therapy Most frequently prescribed BB was metoprolol (n = 488 (42%)) Of the patients prescribed BBs, 519 (45%) received lower doses and 643 (55%) received higher doses BB use was associated with significant reductions in all-cause mortality (HR 0.72; 95% CI: 0.65 to 0.80), mortality due to HF (HR 0.65; 95% CI: 0.47 to 0.90), and hospitalizations for HF (HR 0.82; 95% CI: 0.74 to 0.92) Patients were less likely to be prescribed a BB if: o they were older, had several comorbid conditions, had COPD, or a history of bradycardia/atrioventricular block (all P<0.05) Patients were more likely to be prescribed BBs if: o they had ischemic heart disease or HTN, or if they were taking other medications for HF, particularly ACEIs or loop diuretics (all P<0.05) Patients were more likely to receive lower doses if: o they had a history of heart block, were taking lower doses of ACEIs, or were also receiving digoxin (all P<0.05) The benefits of BBs seen in randomized trials extend to a broader population of elderly patients with HF Peterson, Page 8 of 20 Comments Strengths Large sample size Baseline characteristics similar between groups Evaluated BB dose associations with mortality and morbidity Limitations Retrospective study Unable to monitor adherence (Refills does not guarantee adherence) Did not collect data on functional status/ severity of HF Did not determine if patients had systolic or diastolic dysfunction Included BBs not proven to reduce morbidity and mortality in HF Did not report number of clinical events per dosing group (i.e. number of deaths in each BB group) Table 8. Barywani S., Ergatoudes C., et al. Does the target dose of neurohormonal blockade matter for outcome in systolic heart failure in octogenarians?. Intl J Cardiology 2015. 187:666-672. Purpose Study Design Inclusion criteria Exclusion criteria Outcomes Methods Statistics To investigate whether elderly HF patients receiving ≥50% target dose outperform those receiving <50% target dose, despite maximum up-titration, and whether the target dose outperforms all other doses Retrospective chart review of 2 outpatient HF clinics ≥80 yo LVEF ≤40% LVEF >40% Primary: All-cause mortality after ≥ 5 years Secondary: 5-year cardiac mortality Hospitalization due to worsening HF 185 patients aged ≥80 years with HF and LVEF ≤40% referred between January 2000 and January 2008 to 2 HF outpatient clinics Up-titrations of HF medications o Done by HF specialized nurses according to a prespecified schedule and after discussion with a cardiologist over a 3-6 month period o Titration was stopped after reaching the target dose or highest tolerated dose which was based on the following vital signs HR <55 bpm, SBP <100 mmHg, and increase in SCr of >40% or serum potassium >5.5 mmol/L Definition of groups according to doses o Low dose = <50% of the target dose, intermediate= ≥ 50% of target dose but less than the target dose, and the highest dose group = target dose Common BBs used: metoprolol succinate (84%), bisoprolol (12%), carvedilol (4%) Baseline characteristics descriptive statistics Continuous variables once-way analysis of covariance Categorical variables Chi-squared test Cox proportional-hazard survival model mortality analysis P value <0.05 = statistical significance Kaplan-Meier analysis and univariable Cox proportional-hazard regression analysis were used to build multivariable models for 3 doses of each agent Peterson, Page 9 of 20 Results Author’s Conclusions Comments Primary: All-cause mortality was 76.8% (142 events) Secondary: Cardiac mortality was 60.6% (86 events) Doses after titrations: 50% received <50% of target dose 29% received ≥50% of target dose 21% received target dose Main reasons for not reaching target doses Symptomatic bradycardia (53%), symptomatic hypotension (<100mmHg, 46%), and worsening pulmonary obstruction symptoms (1%) Relationship between dose level and outcome: No significant difference in survival between the target dose and lower dose (<50% of target dose) groups, or between those receiving >50% of the target dose and the lower dose, regardless of all-cause mortality (HR =0.6, 95%CI 0.3-1.1, P =0.115), or cardiac mortality (HR = 0.7, 95%CI 0.4-1.4, P =0.401) No significant differences in non-cardiac deaths or hospital readmissions between the 3 different dose-groups No significant differences in HR between the all 3 groups after up-titration The clinical outcome of BB therapy is independent of BB dose when the target HR is achieved Strengths: Evaluated elderly patients with multiple comorbidities (increased generalizability of results) Evaluated optimal clinical outcomes (mortality/morbidity) Appropriate duration (5 year follow-up) Used guideline recommended BBs Limitations: Small sample size Retrospective study Differences in baseline characteristics Table 9. Pelaez J., Garcia M., et al. Relationship between different doses of beta-blockers and prognosis in elderly patients with reduced ejection fraction. Intl J Cardiology 2016.220: 219–225. Purpose Study Design Inclusion criteria Exclusion criteria Outcomes Methods To determine the impact of different doses of BBs on survival and admission for HF in elderly patients with reduced ejection fraction (REF) Single-center observational study Age ≥ 75yo LVEF ≤ 35% Patients who died or suffered a major cardiovascular event (HF admission requiring intravenous diuretics or sustained ventricular arrhythmia) within this time period Primary Time to all-cause death Secondary Time to first HF admission requiring intravenous diuretics Between January 2008 to June 2014, 784 patients were assessed for eligibility Peterson, Page 10 of 20 Statistics Results Six months after diagnosis, patients were divided into 3 groups depending on BB dose: no BB (NBB), low dose(LD) <50% of the target dose, and high dose (HD) ≥50% of the target dose The maximal tolerated doses of carvedilol, bisoprolol, metoprolol, and nebivolol were recorded for calculations of the ratio of maximal tolerated dose/recommended target dose (50 mg daily for carvedilol, 10 mg for bisoprolol and nebivolol, and 200 mg for metoprolol succinate) Quantitative datamedian and interquartile range (IQR) ANOVA comparison between quantitative variables Linear association X2 test and likelihood ratio X2 test compare qualitative variables Kaplan Meier survival curves Log- rank test comparison between groups Multivariate Cox proportional hazard and propensity-score matched analysis avoid potential cofounding factors Significance P<0.05 Out of 784 patients, 559 were included with a median age of 81.3 years, 134 of whom (24.0%) were not taking BBs, 259 (46.3%) were taking <50% of the target dose, and 166 (29.7%) were taking 50% or more of the target dose Baseline characteristics between the groups were similar with significant differences in age, QRS complex width, resting HR, chronic obstructive pulmonary disease (COPD), cognitive impairment, functional disability, ischemic etiology of REF, NYHA class, in the use of implantable cardioverter defibrillator (ICD), and ivabradine Reported reasons for lack of BB treatment were the following: COPD (35.1%), bradyarrhythmia (13.4%), symptomatic hypotension (6.0%), concomitant use of sotalol (6.0%), and unknown causes (39.5%) Bisoprolol was the most frequently used BB (59.3%), followed by carvedilol (37.4%), metoprolol succinate (2.4%), and nebivolol (0.9%) Median follow-up was ~30 months Primary Outcome: o 212 deaths (NBB: 70 (52.2%); LD: 94 (36.3%); HD: 48 (28.9%)) Cause of death was unknown in 93 (43.9%) patients, 79 (37.3%) died from non-cardiac causes, 6 (2.8%) from sudden death, and 34 (16%) from nonsudden cardiac death Secondary Outcome: o 171 HF admissions (NBB: 42 (31.3%); LD: 85 (32.8%); HD: 44 (26.5%)) Both LD and HD were associated with improved survival, with no differences between them (HD vs. NBB = 0.67, 95% CI (0.46–0.98), P= 0.037; HD vs. LD = 1.03, 95% CI (0.72– 1.46), P= 0.894; and LD vs. NBB = 0.65, 95% CI (0.48–0.90), P= 0.009) BB therapy failed to show benefits in HF admissions Peterson, Page 11 of 20 Author’s Conclusions Comments BB therapy was associated with a significant reduction in mortality and was not associated with a decrease in HF admissions among elderly patients with REF, regardless of dose Strengths: Appropriate statistics (i.e. propensity score matching) Representative of elderly population reflection of real- world clinical practice (comorbidities, +/- BB target doses) Assessed optimal clinical outcomes (mortality/morbidity) Limitations: Single- center observational study Excluded patients with serious events in the first 6 months after diagnosis limits applicability of results to elderly patients with severe REF Did not collect data on changes in BB doses during follow-up Included BB (nebivolol) not shown to reduce mortality Did not evaluate safety reasons for up-titration failure Peterson, Page 12 of 20 A. Literature review summary i. 2002 Sin et al. 1. Reported a 28% reduction in mortality and 18% reduction in hospitalizations which was consistent with the data from the previous trials of BBs 2. All doses of BBs were associated with benefit, but there was a trend towards greater benefit in patients receiving higher doses ii. 2015 Barywani et al. 1. Recommend patients receive the highest tolerable doses of BB vs target doses a. No statistically significant differences in survival or morbidity were observed between the different BB dosing groups iii. 2016 Pelaez et al. 1. Provide evidence that BB treatment improved survival, at low or high doses, in the elderly (≥75 yo) patients with HF (LVEF ≤35%) a. This effect of BB on survival is independent of the target dose reached 2. BB treatment in this patient population has no relationship to probability of HF hospitalizations B. Literature review discussion 11-13, 20-23 i. Survival is independent of BB dose in the elderly ii. Trials suggest HR may be an appropriate indicator for optimized therapy iii. BB doses may not be associated with reductions in HF admissions due to this patient population having a high number of comorbidities that may mask or mimic HF symptoms iv. Proposed that achieving target BB doses in the elderly does not always guarantee optimal treatment X. Safety A. Studies suggests that BBs are mostly well-tolerated in the elderly B. Most common reported reasons for up-titration failure include: i. Symptomatic bradycardia, symptomatic hypotension, and pulmonary adverse events XI. Conclusion A. Up-titration of BBs to target doses in the elderly is challenging i. Limited by age, polypharmacy, bradycardia, hypotension, etc. B. According to current literature, achieving target doses in the elderly is not associated with better survival outcomes i. Benefit on morbidity is inconsistent C. Randomized controlled trials are needed to determine the optimal BB doses in elderly HF patients D. Would recommend to initiate BBs in this patient population at low doses and titrate up to the highest tolerated dose based on HR and BP Peterson, Page 13 of 20 XII. References 1. Yancy CW, et al. 2013 ACCF/AHA guideline for the management of heart failure. Circulation. 2013; 128:240-327. 2. Yancy CW, et al. 2016 ACC/AHA/HFSA focused update on new pharmacological therapy for heart failure: an update of the 2013 ACCF/AHA guideline for the management of heart failure. Circulation. 2016; 134:1-46. 3. Moore, T and Anderson, J. Chapter 2. Heart failure. Pharmacotherapy in Primary Care. Eds. William D. Linn, et al. New York, NY: McGraw-Hill, 2009. 4. Mann, Douglas L., and Murali Chakinala. "Heart Failure: Pathophysiology and Diagnosis." Harrison's Principles of Internal Medicine, 19e. Eds. Dennis Kasper, et al. New York, NY: McGraw-Hill, 2015. n. pag. AccessMedicine. Web. 3 Sep. 2016. 5. McMurray, J., Packer, M., et al. Angiotensin–neprilysin Inhibition versus enalapril in heart failure. N Eng J Med 371; 11(2014):993-1004. 6. Lexicomp Online®, Pediatric & Neonatal Lexi-Drugs®, Hudson, Ohio: Lexi-Comp, Inc. August 2016. 7. Rich MW. Chapter 78. Heart Failure. In: Halter JB, Ouslander JG, Tinetti ME, Studenski S, High KP, Asthana S. eds. Hazzard's Geriatric Medicine and Gerontology, 6e. New York, NY: McGraw-Hill; 2009 8. Diez-Villanueva P. and Fernando, A. Heart failure in the elderly. J Ger Card. 2016. 13:115-117. 9. Lien C, Gillespie N, et al. Heart failure in frail elderly patients: diagnostic difficulties, comorbidities, polypharmacy and treatment dilemmas. Eur J Heart Fail 2002; 4: 91–98. 10. Cacciatore F, Abete P, Mazzella F, et al. Frailty predicts longterm mortality in elderly subjects with chronic heart failure. Eur J Clin Invest 2005; 35: 723–730. 11. Moser DK, Dracup K, Evangelista LS, et al. Comparison of prevalence of symptoms of depression, anxiety, and hostility in elderly patients with heart failure, myocardial infarction, and a coronary artery bypass graft. Heart Lung 2010; 39:378–385. 12. Dobre D., Haaijer-Ruskamp F., et al. B-adrenoreceptor antagonists in elderly patients with heart failure. Drug Aging. 2007. 24: 1031-44. 13. Pelaez J., Garcia M., et al. Relationship between different doses of beta-blockers and prognosis in elderly patients with reduced ejection fraction. Intl J Cardiology 2016.220: 219–225. 14. Barywani S., Ergatoudes C., et al. Does the target dose of neurohormonal blockade matter for outcome in systolic heart failure in octogenarians?. Intl J Cardiology 2015. 187:666-672. 15. Gelbrich G., Edelmann F., et al. Is target dose the treatment target? uptitrating beta-blockers for heart failure in the elderly . Intl J Cardiology 2012. 155:160–166. 16. Gheorghiade M., Colucci W., et al. B-blockers in chronic heart failure. Circulation, 2003; 107:157075. 17. Beta blockers. Micromedex. Truven Health Analytics. August 2016. 18. Malek, Filip. Reaching betablockers target dose in elderly patients with chronic heart failure. Cor Et Vasa. 2014,56:37-41. 19. The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): a randomized trial, Lancet. 1999;353: 9–13. 20. Effect of metoprolol CR/XL in chronic heart failure: metoprolol CR/XL randomize intervention trial in congestive heart failure (MERIT-HF), Lancet.1999; 353:2001–2007. 21. Packer M., Fowler M., et al. Effect of carvedilol on the morbidity of patients with severe chronic heart failure: results of the carvedilol prospective randomized cumulative survival (COPERNICUS) study, Circulation. 2002:106:2194–99. Peterson, Page 14 of 20 22. Dungen H., Apostolovic S., et al. On behalf of CIBIS-ELD Investigators. Titration to target dose of bisoprolol vs. carvedilol in elderly patients with heart failure: the CIBISELD trial, European Journal of Heart Failure. 2011; 13:670–680. 23. Calvert MJ, Shankar A, McManus RJ, Ryan R, Freemantle N. Evaluation of the management of heart failure in primary care. Fam Pract 2009;26:145–153. 24. Komajda M, Follath F, Swedberg K, et al. The Euroheart Failure Survey programme—a survey on the quality of care among patients with heart failure in Europe: Part 2: treatment. Eur Heart J 2003;24: 464–474. 25. Cheng J., et al. A review of heart failure management in the elderly population. Am J Geriatr Pharmacother. 2009; 7:233–249. 26. Dulin B., et al. Do elderly systolic heart failure patients benefit from beta blockers to the same extent as the non-elderly? meta-analysis of >12,000 patients in large-scale clinical trials. Am J Cardiol 2005;95:896–898. 27. Word Health Organization. 2016. Accessed on September 25, 2016. Available at: http://www.who.int/healthinfo/survey/ageingdefnolder/en Peterson, Page 15 of 20 Appendix: Appendix A. Figure 2 and 3. Pathophysiology of HF3 Peterson, Page 16 of 20 Appendix B. Table 10 Guideline Treatment Recommendations1-2 Recommendations for Pharmacological Therapy for Management of Stage C HFrEF Peterson, Page 17 of 20 Table 11. Recommendations for Treatment of HFpEF Table 12 2016 ACC/AHA/HFSA focused update on new pharmacological therapy for HF: an update of the 2013 ACCF/AHA guideline recommendations Peterson, Page 18 of 20 Appendix C. Table 13. Pharmacology of BBs recommended by 2013 ACCF/AHA HF guidelines6,17 Drug Carvedilol Metoprolol Succinate Mechanism of Blockade Dosing considerations Warning Absorption Metabolism/ Distribution Excretion Half- Life Absolute Contraindications Relative Contraindications Most common Drug Interactions Most common Adverse Reactions Pregnancy Monitoring Bisoprolol * Non-selective α1,β1,β2 β1 selective β1 selective IR: (Initial dose) 3.125mg BID; double dose every 2 weeks to target dose Maximum recommended dose: Mild to moderate HD: <85 kg: 25 mg BID >85 kg: 50 mg BID Severe HF: 25 mg BID Initial: 25 mg once daily (reduce to 12.5 mg once daily in NYHA class higher than class II); may double dosage every 2 weeks as tolerated up to target dose of 200 mg/day Initial: 1.25 mg once daily; may double dosage every 2 weeks as tolerated up to target dose of 10 mg once daily ER: (Initial dose) 10mg once daily, titrate dose every 2 weeks Maximum dose: 80mg once daily Therapy should not be withdrawn abruptly, but gradually tapered over 1 to 2 weeks to avoid acute tachycardia, hypertension, and/or ischemia Rapid and extensive; delayed with Rapid Rapid food Extensively (98%) hepatic via CYP2D6 Extensively hepatic via Extensively hepatic Vd: 115 L; distributes into CYP2D6; Vd: 3.2 to 5.6 L/kg; Widely distributed; extravascular tissues crosses the blood brain highest concentrations barrier in heart, liver, lungs, and saliva; crosses blood-brain barrier Primarily feces Primarily urine Primarily urine 7 to 10 hours 3 to 4 hours 9 to 12 hours Advanced heart block (2nd or 3rd degree), Sick sinus syndrome (without a functional pacemaker), severe bradycardia (<50 bpm), cardiogenic shock, decompensated HF Caution in HF, COPD, diabetes, and peripheral vascular disease, asymptomatic hypotension, sinus bradycardia (50 to 60 bpm), depression CYP2D6 substrates CYP2D6 substrates CYP3A4 substrates Hypotension (9% to 20%), dizziness (2% to 32%), fatigue (4% to 24%), hyperglycemia (5% to 12%), weight gain (10% to 12%), diarrhea (1% to 12%) Hypotension (1% to 27%), bradycardia (2% to 16%), dizziness (2% to 10%), fatigue (1% to 10%), depression (>2% to 5%) C C HR, BP, renal function, liver function, blood glucose in diabetics Fatigue (dose related; 6% to 8%), diarrhea (dose related; 3% to 4%), upper respiratory infection (5%), rhinitis (3% to 4%) C *Not FDA approved for HF in US Peterson, Page 19 of 20 Appendix D. Table 14. Major Placebo- Controlled Trials of BBs Supporting HF Guideline Recommendations 1-2 Drug Trial Mean N Patient Mean Target % Achieved follow Population age dose Target dose -up (yo) Metoprolol MERIT-HF 1 yr 3991 NYHA ll-lV; 64 200mg 64% XL (1999) LVEF <40%; daily Bisoprolol* CIBIS-II (1999) 1.3 yrs 2647 Carvedilol COPERNICUS (2002) 10.4 mo 2289 NYHA class III-IV; LVEF <35% NYHA class lV; LVEF <25% Mortality/ Morbidity (RRR) ↓ 34%/ ↓ 18% 61 10mg daily 48% ↓ 34%/ ↓ 20% 63 25mg BID 65% ↓ 35%/ ↓ 20% *Not FDA approved for HF in US CIBIS-II (Cardiac Insufficiency Bisoprolol Study II) MERIT-HF (Metoprolol CR/XL Randomized Intervention Trial in Congestive Heart Failure) COPERICUS (Carvedilol Prospective Randomized Cumulative Survival) APPENDIX E. Table 16. BB Clinical Trials Included in Meta-analysis26 Drug Trial Mean N Patient follow-up Population (mo) Metoprolol MERIT-HF 12 3991 NYHA ll-lV; XL (1999) LVEF <40% Mean age (yp) 64 Inclusion Criteria (Age, yo) 40-80 % ≥70yo 31% Mortality/ Morbidity (RRR) ↓ 34%/ ↓ 18% NYHA class III-IV; LVEF <35% NYHA class lV; LVEF <25% 61 18-80 20% ↓ 34%/ ↓ 20% 63 ≥18 NR ↓ 35%/ ↓ 20% Bisoprolol* CIBIS-II (1999) 15.6 2647 Carvedilol COPERNICUS (2002) 10.4 2289 Carvedilol Carvedilol U.S. Trials (1996) 6.5 1094 NYHA ll-lV; LVEF <35% 59 ≥18 NR ↓ 65%/ ↓ 27% Bucindolol* BEST (2001) 24 2708 NYHA llI-lV; LVEF <35% 60 >18 28% NS/ ↓ 8% NS= non-significant, NR= Not reported *Not FDA approved for HF in US BEST (Beta-Blocker Evaluation of Survival Trial) Peterson, Page 20 of 20