* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Off Schedule Laboratory Tests
Eradication of infectious diseases wikipedia , lookup
Epidemiology of metabolic syndrome wikipedia , lookup
Fetal origins hypothesis wikipedia , lookup
Forensic epidemiology wikipedia , lookup
Epidemiology wikipedia , lookup
Seven Countries Study wikipedia , lookup
Public health genomics wikipedia , lookup
Prenatal testing wikipedia , lookup
Alzheimer's disease research wikipedia , lookup
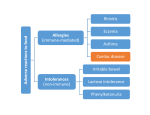
PEGASUS HEALTH GP SMALL GROUP EDUCATION DIAGNOSTIC DILEMMAS Diagnostic Dilemmas Tests covered in this session: Faecal calprotectin HLA DQ2/DQ8 Homocysteine BNP Vitamin D (a quick look at data) Case One Samantha, 34 year old woman: 6/12 diarrhoea Abdo cramps Occasional PR bleeding No weight loss What else would you like to know? What are the differential diagnoses? Case One – Differential Dx Irritable Bowel Syndrome Coeliac Disease Inflammatory Bowel Disease Lactose Intolerance Infective Diarrhoea Endometriosis Pelvic Inflammatory Disease Cancer in older patient – Colorectal or Ovarian What tests (if any) would you order for Samantha? Faecal Calprotectin Testing Pros: Helps rule out inflammatory causes of diarrhoea High negative predictive value Cons: Can be raised in all causes of GI inflammation (including irritation from NSAID use) Many false positives occur Also increases with age, inactivity, and obesity Samantha – 6 Months Later Sister just diagnosed with coeliac disease Samantha on gluten free diet last 4/52 with only slight improvement in symptoms Requesting blood test for coeliac disease What do you do now? Is HLA gene testing appropriate? Human Leucocyte Antigens & Coeliac Disease >99% coeliac patients are HLA DQ2/DQ8 positive HLA testing has >99% negative predictive value 20-30% general population HLA DQ2/DQ8 positive • only 3% of these will develop coeliac disease HLA genes necessary but not sufficient for development of coeliac disease Human Leucocyte Antigens & Coeliac Disease Entire NZ Population 30% of Caucasian population will test positive for HLA DQ2/8 3% of those with a positive HLA will develop coeliac disease 0.1% of those with negative HLA will develop coeliac disease Illustration for Patients What Role Does HLA Typing Play? Not diagnostic for coeliac disease (high rate false +ve) Negative test rules out coeliac disease IgA tTG is first-line test for Dx coeliac disease If positive, go back on gluten for 4wks then test IgA tTG and total IgA HLA testing not indicated if family history coeliac disease (~10% prevalence in 1st degree relatives) Vitamin D Testing GP count by number of tests Number of GPs (9 month period from July 09 – Mar 10) 92 Total number tests = 2911 Number unique patients = 2780 50 41 31 28 14 14 9 1 2 3 4 5 6 7 8 11 10 6 9 10 4 11 12 3 4 13 14 7 6 4 6 6 2 2 2 1 0 1 15 16 17 18 19 20 21-30 31-40 41-50 51-99 100+ Number of tests/GP Indications for Testing Vitamin D Atypical osteoporosis Unexplained raised serum alkaline phosphatase or low calcium or phosphate Unexplained proximal limb pain in older people Unexplained bone pain, unusual fractures or other evidence suggesting metabolic bone disease Malabsorption disorders Long-term anticonvulsant therapy High risk for deficiency Consider supplementation for: Institutionalised or house-bound elderly People who are veiled Very dark skin and little sunlight Infants exclusively breastfed by mothers at risk of deficiency Cholecalciferol 1.25mg 2 stat then 1 monthly No requirement for prior testing or monitoring Case 2 - Homocysteine Bill, 55yrs, long-term patient, few visits Recent NSTEMI Committed to changing his lifestyle to reduce his risk of another “heart attack” Wants his homocysteine level tested What do you know about homocysteine? Hyperhomocysteinaemia Has been linked to: MI, acute coronary syndrome, recurrent coronary events Premature coronary heart disease Cardiovascular and total mortality Adverse outcomes after angioplasty Carotid artery stenosis Stroke, recurrent stroke, silent brain infarct Venous thromboembolic disease (PE/DVT) What factors can cause ↑ homocysteine levels? Is Knowledge of Homocysteine Level Useful in Improving Outcome? There is evidence that reducing homocysteine levels is of no benefit There is no evidence to support screening Routine homocysteine testing is not justified So… Would you Test Bill? No. What would you tell Bill? Knowing Bill’s homocysteine level will not alter his management or risk Modification of risk factors such as DM, smoking, hypertension, and hypercholesterolemia shown to be beneficial Case 3 John, 73y, 1mth history increasing SOB NSTEMI 18 mth ago Mild hypertension, hypercholesterolaemia On Examination • • • • Temp 37.6, P 88 reg, BP 150/95 HS dual and nil Chest dull at bases, some coarse creps Trace pedal oedema What else do you want to know? What are the differential diagnoses? What investigations would you do? BNP (Brain Natriuretic Peptide) Secreted in response to ventricular distension High negative predictive value useful for ruling out HF Diagnosing HF is difficult in Primary Care: - Early symptoms often mild and non-specific - Clinical findings neither specific nor sensitive - Echo not readily available Back to John… BNP = 52 pmol/L < 30 30 – 80 >80 What does this mean? Low – HF unlikely (2%) Indeterminate – HF still possible High – HF likely (95%) A normal BNP in an untreated patient effectively rules-out heart failure An intermediate BNP does not rule out heart failure A high BNP indicates heart failure but does not exclude other chest/heart problems Alternative Scenario What if John’s BNP was 217 pmol/L? (High) What would this mean? How would you manage him? Can you use BNP testing to guide optimal drug treatment of John’s HF? When is BNP Useful in General Practice? High BNP supports diagnosis of HF o but does not exclude other conditions Low BNP can rule out HF in an untreated patient May have role in known HF patients o for helping diagnose cause of acute dyspnoea When is BNP not Useful in General Practice? No role in screening for asymptomatic LV dysfunction monitoring well patients who have HF excluding CHF in those already on therapy Not recommended for guiding drug titration in HF patients with obvious clinical diagnosis of HF BNP Data GP count by number of BNP tests Number of GPs (9 month period from July 09 – Mar 10) 200 180 175 Total number tests = 4563 Number unique patients = 3728 160 140 120 100 85 80 57 60 40 22 20 20 16 9 4 7 36 to 40 41 to 45 3 8 2 0 1 to 5 6 to 10 11 to 15 16 to 20 21 to 25 26 to 30 31 to 35 46 to 50 51 to 100 > 100 Number of tests/GP Summary - Diagnostic Dilemmas ‘Off-schedule’ tests were developed in 2° care - Place in 1° care not yet established Only test if it will influence management Most of these tests have significant limitations Test results may be misleading Paramount to use clinical judgment Take Home Messages Faecal Calprotectin • • HLA DQ2/DQ8 • • second line test may help rule out Inflammatory Bowel Disease in young patient with chronic diarrhoea Not recommended to diagnose Coeliac Disease 30% of Caucasians express these markers Vitamin D • Don’t test, just treat Take Home Messages Cont’d Homocysteine • • BNP • • • Reducing levels does not improve patient outcomes No role for testing If normal, useful to rule out HF If high, may support diagnosis of HF May be raised by other conditions that strain the heart Sometimes it is best not to do a test!