* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Highly lipophilic Β-lactams ~ 10-30% of serum
Survey
Document related concepts
Transcript
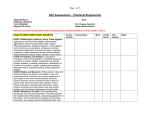
Pharm 9- Pharmacology of CNS Infections Bacterial Meningitis Meningitis is the most common type of CNS infection In the U.S., the 3 most likely pathogens are Streptococcus pneumoniae, Neisseria meningiditis, and Hemophilus influenzae The incidence of H. influenzae infections has declined by more than 90% since the introduction of the Hib vaccine in 1985 The pneumococcal vaccine, introduced in 2000, decreased rates of meningitis in children less than 5 years old nearly 60% Important anatomical considerations for drug therapy Barriers to exchange of drugs: blood-brain-barrier (BBB) and blood-CSF barrier (BCSFB) BBB – tightly joined capillary endothelial cells; drugs enter by direct passage and penetrate the glial cells that envelop the capillary structure BCSFB – tightly fused ependymal cells of the choroid plexus create a barrier to diffusion of substances The surface of the BBB is > 5000 times that of the BCSFB Treatment Principles Prompt institution of appropriate antimicrobial therapy; delay is associated increased morbidity and mortality Antibiotics must penetrate adequately into the CSF Regimen must have potent activity against the known or suspected pathogen(s) AND exert a bactericidal effect Antimicrobial penetration into CSF Amount of bacteria in the CSF is often much higher than the standard inoculum used for susceptibility testing (105 CFUs/mL) Inoculum effect: increase in MIC with increase in inoculum size Purulent CSF is acidic; may reduce bactericidal activity Lipid solubility, molecular weight, protein binding, active transport systems of the choroid plexus also affect penetration Good news – penetration of most antibiotics into the CSF is increased when the meninges are inflamed Pharm 9- Pharmacology of CNS Infections Treatment by Organism S. pneumonia (Pneumonococcus): gram+ aerobe 3rd generation cephalosporins: cefotaxime or ceftriaxone PLUS Vancomycin, in case of highly resistant isolates Monitor culture & sensitivity results and adjust accordingly Duration of therapy: 10-14 days 3rd Generation cephalosporins o Cefotaxime and ceftriaxone o Good activity against pneumococcus o MOA: Cell wall synthesis inhibitors o P’kinetics: given IV o Cefotaxime metabolized by the kidney & liver; active metabolite; 20-36% excreted unchanged via urine; t ½ ≈ 1 h; adjust dose if ClCr < 20 mL/min o Ceftriaxone metabolized & excreted by the kidney and bile/feces (33-67% unchanged); t ½ ≈6-9h o AEs: Well-tolerated; ~ 5% “cross-sensitivity” with pcns; diarrhea w/high doses ceftriaxone; “biliary sludging” o CI: ceftriaxone - neonates with hyperbilirubinemia Vancomycin o Active against gram+ cocci (aerobes), some strains of MRSA o MOA: bacterial cell wall synthesis inhibitor o P’kinetics: not absorbed orally; not metabolized; eliminated via the kidney; t ½ ≈ 4-6 h o AEs: o “Red man syndrome” – hypotension and erythematous rash on the face if infused too quickly o Oto- and possibly nephrotoxicity w/high concentrations Pharm 9- Pharmacology of CNS Infections N. meningiditis (Meningococcus): gram- aerobe Aggressive, early, high-dose penicillin G IV q4h OR 3rd generation cephalosporin (cefotaxime or ceftriaxone) Alternative: chloramphenicol Monitor culture & sensitivity results and adjust accordingly Duration of therapy: 7 days Spread by direct person-to-person contact including respiratory droplets & pharyngeal secretions Prophylaxis for close contacts (day care center, household): rifampin PO every 12 h for 2 days Penicillin o Active against gram+ cocci, N. meningiditis & spirochetes o MOA: bacterial cell wall synthesis inhibitors o P’kinetics: metabolized & eliminated via the kidneys; t ½ ≈ 20-30 min o AEs: immediate hypersensitivity (IgE), i.e., urticaria or anaphylactic shock, serum sickness, interstitial nephritis, rash o CI: penicillin allergy Chloramphenicol o Active against gram+ cocci, meningococci, H. influenzae in meningitis o MOA: binds to the 50S ribosomal subunit and inhibits bacterial protein synthesis o P’kinetics: lipophilic - concentrations in CNS; metabolized by the liver; excreted via the kidney; t ½ ≈ 1.5 – 4 h o AEs: “Gray baby” syndrome – weakness, respiratory depression, hypotension, shock & ashen gray cyanosis; aplastic anemia o DIs: CYP 3A4 inhibitor o Rarely used due to unpredictable metabolism in infants and DIs Rifampin o Broad spectrum, active against gram+, gram- and acid-fast bacilli including M. tuberculosis & M. aviumintracellulare o MOA: binds to the β-subunit of RNA polymerase; inhibits protein synthesis o P’kinetics: rapidly absorbed; widely distributed including lung, saliva, peritoneal and pleural fluids; metabolized in the liver to desacetylrifampin (active metabolite); excreted primarily in the feces via biliary elimination; t ½ ≈ 3-5 h; 2-3h with repeated dosing o AEs: hepatitis – monitor LFTs; hypersensitivity reaction – flu-like; reddish-brown saliva, tears & urine o Drug interactions Inducer of CYP450 1A2, 2C9, and 3A4- increases metabolism of macrolides, calcium channel blockers, digoxin, estrogens, warfarin and others P-gp inducer H. influenzae 3rd generation cephalosporins – active against β-lactamase-producing and non- β-lactamase-producing H. influenzae Switch to ampicillin if pcn-susceptible Duration of therapy: 7 days Prophylaxis with rifampin for close contacts Exposed unvaccinated children should receive the vaccine Pharm 9- Pharmacology of CNS Infections L. monocytogenes: gram+ aerobe/ facultative anaerobe Neonates, alcoholics, immunocompromised adults and elderly Penicillin G or ampicillin +/- gentamicin Alternative: TMP/SMX Duration of therapy: ≥ 21 days; combination for 10-day minimum; complete with pcn or ampicillin alone Gentamicin o Active against aerobic gram-negative bacilli; synergistic against L. monocytogenes o MOA: binds to the 30S ribosomal subunit, inhibiting protein synthesis o P’kinetics: poor absorption; eliminated via the kidneys; t ½ ≈ 2.5 h o AEs: renal toxicity, ototoxicity TMP-SMX o Active against gram- aerobes, MRSA o MOA: bacterial dihydrofolate synthesis inhibitor o P’kinetics: well absorbed; widely distributed (CSF); excreted via urine; t ½ ≈ 6-10 h o AEs: skin hypersensitivity reactions (Stevens-Johnson Syndrome), hemolytic anemia w/G6PD deficiency, hyperkalemia o DIs: warfarin, phenytoin Adjunctive treatment Dexamethasone o MOA: inhibits the production of cytokines TNF and IL-1 o Possible protection against hearing loss o Recommendations: give dexamethasone for pneumococcal or H. influenzae meningitis in adults and children for 2-4 days o 1st dose should be administered prior to the 1st dose of antibiotics Prevention= VACCINATION Pharm 9- Pharmacology of CNS Infections Brain Abscess Bacterial - Streptococci (aerobic, anaerobic, and microaerophilic) 70%; Staphylococcus aureus 10% - 20%; Bacteroides species, gram- bacilli Protozoal - Toxoplasma gondii is most common Fungal - Candida spp. is most prevalent Treatment Principles Antimicrobial therapy with high-dose intravenous agents has traditionally been administered for 6 to 8 weeks in patients with bacterial brain abscesses o Shorter courses (3 - 4 weeks) of antimicrobial therapy may be adequate for patients who have undergone surgical excision of the abscess Optimal therapy for brain abscesses usually requires a combined medical and surgical approach There is no role for monotherapy for toxoplasmosis Metronidazole o Active against: anaerobic bacteria; some parasites o Nitroimidazole compound, chemically reduced in anaerobic bacteria o MOA: reactive reduction products (free nitro-radicals) appear to exert antimicrobial activity o P’kinetics: well absorbed; good penetration into brain abscess cavities; extensively metabolized; renally excreted o AEs: anorexia, N/V, metallic taste; take w/food o DIs: 2C9 inhibitor; warfarin. Disulfiram-like reaction w/EtOH: nausea, vomiting, sweating, flushing, palpitations & dyspnea Toxoplasmosis (T. gondii) Pyrimethamine – most effective anti-Toxoplasma agent o MOA: folic acid antagonist (inhibits dihydrofolate reductase) o P’kinetics: excreted via urine t½ ≈ 96 h o AEs: bone marrow suppression (most common), which may be decreased by concomitant administration of folinic acid; GI distress, rash, headaches, a bad taste in the mouth o DIs: other myelosuppressive drugs AND Sulfadiazine – synergistic with pyrimethamine o AEs: skin rashes (which may be life-threatening) and crystal-induced nephrotoxicity Alternative: Clindamycin o AEs: diarrhea, Clostridium difficile colitis (diarrhea, abdominal pain and fever) Pharm 9- Pharmacology of CNS Infections Viral Encephalitis Prolonged hospitalizations, a multitude of expensive diagnostic tests, and frequently poor outcomes including disability and death Worldwide – mumps and poliomyelitis U.S. – coxsackieviruses A & B and enteroviruses 70 & 71 account for 85% Pathogens are not usually identified; 1/3 to 2/3 of encephalitis cases remain of unknown, thus, treatment is supportive Herpes simplex virus is treated with IV acyclovir; decreases mortality to 20% Alternative for acyclovir-resistant HSV: foscarnet Acyclovir MOA: Nucleoside analogue that competitively inhibits DNA polymerases & terminates DNA elongation inhibits viral DNA & RNA synthesis P’kinetics: bioavailability 22%; distributes into CSF, vesicular fluid, vaginal secretions and tissues; excreted renally; t ½ ≈ 3 h AEs: phlebitis (15%), crystalline nephropathy DIs: probenecid Foscarnet MOA: inhibits DNA & RNA polymerases & reverse transcriptases Used primarily for CMV retinitis; alternative for acyclovir-resistant HSV P’kinetics: low bioavailability, given IV; binds to divalent cations and accumulates in bone; excreted unchanged in urine; t ½ ≈ 3-4h AEs: hypocalcemia, hypomagnesemia, seizures, cardiac arrhythmias, renal insufficiency (monitor SCr) DIs: other nephrotoxic drugs (aminoglycosides, acyclovir) Pharm 9- Pharmacology of CNS Infections Fungal Meningitis Cryptococcus neoformans is the most common cause of fungal meningitis Major cause of morbidity and mortality, especially in immunosuppressed patients 85% of cases in HIV-infected patients DOC – amphotericin B +/- flucytosine Alternative: azole antifungals – fluconazole, posaconazole Amphotericin B Polyene antifungal active against a wide variety of fungi MOA: Binds to ergosterol in fungal membranes, permeability; K+ & Mg++ leaks out metabolism is disrupted (also bind to cholesterol in mammalian cells) P’kinetics: not absorbed orally; hepatic metabolism; excreted in the urine; t ½ ≈ 24h; 15 d AEs:”Amphoterrible” – renal toxicity in 80% of patients; hypokalemia & hypomagnesemia; acute liver failure, arrhythmias, anemia, leukopenia, thrombocytopenia, chills, fever, headache N/V: pre-treatment with corticosteroids, acetaminophen and antihistamines may help Note: lipid formulations cause less renal toxicity DIs: other nephrotoxic drugs (aminoglycosides, etc.) Flucytosine Pyrimidine antimetabolite MOA: inhibits protein synthesis; only antifungal that affects nucleic acid Drug resistance develops rapidly; used in combination w/amphotericin B P’kinetics: well absorbed; excreted unchanged in urine; t ½ ≈ 3-6 h AEs: well-tolerated; myelosuppression DIs: other nephrotoxic drugs (aminoglycosides, etc.) Azole antifungals (fluconazole, et al) Active against a wide variety of fungi MOA: inhibit 14-α-demethylase and block ergosterol synthesis P’kinetics: well absorbed; widely distributed to tissues and body fluids; only fluconazole, voriconazole & posaconazole achieve significant concentrations in the CSF; hepatic metabolism; renal excretion; t ½ ≈ 35h AEs: hepatotoxicity DIs: 2C9/19, 3A4 inhibitor; HMG-CoA-reductase inhibitors (“statins”), warfarin, some benzodiazepines Pharm 9- Pharmacology of CNS Infections Bottom Line… Treat immediately…or faster! Do appropriate lab/diagnostic tests Empiric coverage for the most common pathogens Use drugs that penetrate the BBB, at a high enough dose for a sufficient length of time