* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Small Business Program 2016
Survey
Document related concepts
Transcript
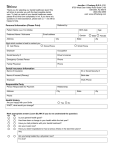
Small Business Program 2016 We keep you smiling ® Delta Dental Insurance Company Delta Dental of Delaware, Inc. Delta Dental of New York, Inc. Delta Dental of Pennsylvania Delta Dental of West Virginia Alpha Dental Programs, Inc. Businesses of all sizes are big on value. That’s why Delta Dental created a portfolio of its most popular plans — each specially designed to provide maximum value for your small business. You can rely on Delta Dental to provide cost management, superior access to dentists and dental plans to meet your needs. No matter which Delta Dental plan you choose, you can feel confident knowing that you’ve chosen a plan that protects your employees and offers your business big value. Delta Dental PPOSM Delta Dental PPO is our open network plan that balances moderate savings with maximum access to network dentists. Enrollees may visit any licensed dentist but usually have the lowest out-of-pocket costs when visiting a PPO dentist. Delta Dental offers access to one of the largest contracted networks of its kind in the U.S., with two levels of savings; Delta Dental PPO and Delta Dental Premier®. Through this two-tier network approach, enrollees are protected from the higher costs that are likely when services are provided by non-Delta Dental dentists. Our small business program offers employers access to a variety of plan options often available only to large employers. These options include PPO plan designs that reimburse the dentist based on the PPO provider’s contracted fee both in- and out-of-network or the PPO plus Premier plan designs that will reimburse Delta Dental Premier dentists based on their contracted Premier fee. With PPO plus Premier — our unique PPO plan design feature — employers can take advantage of the savings from the PPO plan while providing employees with expanded access to Delta Dental dentists who can limit their out-of-pocket costs. PPO dentists accept fees that are more deeply discounted than the fees accepted by dentists who participate in the larger Premier network. Employees who visit a non-PPO dentist can save more by visiting a Premier dentist than they can by visiting a non-Delta Dental dentist. PPO plus Premier provides maximum network access while offering deeper savings within the PPO network and a level of cost protection with the Premier network. All Delta Dental dentists make visits easy and convenient because they file claims and accept payment for services directly from Delta Dental. Patients are only responsible for their share at the time of treatment —they pay no more than the fees allowed by Delta Dental, thus are not required to pay the entire claim up front and wait for reimbursement when they visit a Delta Dental dentist. DeltaCare® USA DeltaCare USA is our closed network prepaid plan that features set copayments, no annual deductibles and no maximums for covered benefits. Enrollees must select a primary care dentist in the DeltaCare USA network from whom they receive treatment, as in a traditional dental HMO. With DeltaCare USA, businesses enjoy higher cost controls, while still providing employees with a broad range of dental benefits. DeltaCare USA delivers quality care for less cost than our traditional fee-forservice plans. DeltaCare USA dentists undergo a comprehensive credentialing process to ensure they meet high-quality standards. The majority of diagnostic and preventive procedures are covered at no cost to the enrollee. DeltaCare USA plans are available in District of Columbia, Maryland, New York, Pennsylvania and West Virginia. Table of Contents Delta Dental PPO — Employer–Paid 2-3 Delta Dental PPO — Voluntary 4-5 How the PPO Plan Works 6 PPO Underwriting Guidelines 7 PPO Limitations and Exclusions 8 DeltaCare USA 9 Using The DeltaCare USA Plan 10 DeltaCare USA Underwriting Guidelines 11 DeltaCare USA Limitation and Exclusions 12-13 Delta Dental’s Value Proposition 14 Delta Dental’s Mission Statement 15 Delta Dental PPO — Employer Paid Summary of Benefits1 PPO 1 PPO Dentists/ NonPPO Dentists Reimbursement Basis For businesses with 2-99 eligible employees PPO 2 PPO Dentists/ NonPPO Dentists PPO 32 PPO Dentists/ NonPPO Dentists PPO 4 PPO Dentists/ NonPPO Dentists PPO A PPO Dentists PPO B NonNonPPO PPO PPO Dentists Dentists Dentists Delta Dental PPO, Delta Dental Premier and Non-Delta Dental dentists: the lesser of the submitted charge or the PPO provider contracted fee. Diagnostic (deductible waived) • Exams (two per calendar year) • Bitewing x-rays (two per calendar year) 100% 100% 100% 100% 100% 80% 100% 80% Preventive (deductible waived) • Prophylaxis (cleaning) (two per calendar year and one additional cleaning for pregnant women) • Fluoride treatments (to age 19) (two per calendar year) • Sealants (to age 14) • Space maintainers (to age 14) 100% 100% 100% 100% 100% 80% 100% 80% Basic Restorative •F illings (amalgam “silver” and composite “white” non-molar) 50% 80% 80% 80% 80% 60% 80% 60% Oral Surgery •E xtraction and oral surgery procedures including pre- and post-operative care •G eneral anesthesia and IV sedation are covered when used in conjunction with covered oral surgical procedures Not a benefit 80% 80% 80% 80% 60% 80% 60% Endodontics • Pulpal therapy • Root canal therapy Not a benefit 80% 80% 80% 80% 60% 80% 60% Periodontics •T reatment to the gums and supporting structures of the teeth Not a benefit 80% 80% 80% 80% 60% 80% 60% Major Restorative3 • Inlays • Onlays • Crowns Not a benefit Not a benefit 50% 50% 50% 50% 50% 50% Prosthodontics3 •P rocedures for replacement of missing teeth by construction or repair of bridges and partial or complete dentures Not a benefit Not a benefit 50% 50% 50% 50% 50% 50% Implants3 Not a benefit Not a benefit 50% 50% 50% 50% 50% 50% Orthodontics3 •S traightening of teeth (children only to age 19) • $1,000 lifetime maximum (per person) Not a benefit Not a benefit Not a benefit 50% 50% 50% Calendar year deductibles (per person/per family) $25/$75 $50/$150 $50/$150 $50/$150 $1,000 $1,500 $1,500 $1,500 Calendar year maximum (per person) Not a benefit $50/ $150 $75/ $225 $50/ $150 $75/ $225 $1,500 $1,000 $1,500 $1,000 1 Subject to Limitations and Exclusions shown on page 8. The benefit explanations contained herein are subject to all provisions of the group dental service contract and do not modify such contract in any way, nor shall the enrollee accrue any rights because of any statement in or omission from this highlight sheet. 2 Groups with 2-4 eligible employees are limited to PPO 3, PPO Plus Premier 3 and PPO V2, and a calendar year maximum of $1,000 will apply ($1,000/$750 for PPO Plus Premier 3). 3 For groups under 25 employees there is a six-month waiting period for all major restorative, prosthodontic, implant and orthodontic services. The waiting period may be waived if group can provide proof of prior comprehensive group dental coverage with no break in coverage (copy of group’s prior carrier’s EOC and last bill). 2 Delta Dental PPO — Employer Paid Summary of Benefits1 PPO plus Premier 1 PPO Dentists/ NonPPO Dentists Reimbursement Basis For businesses with 2-99 eligible employees PPO plus Premier 2 PPO Dentists/ NonPPO Dentists PPO plus Premier 32 PPO Dentists/ NonPPO Dentists PPO plus Premier 4 PPO Dentists/ NonPPO Dentists PPO plus Premier A PPO Dentists PPO plus Premier B NonNonPPO PPO PPO Dentists Dentists Dentists Delta Dental PPO dentists: the lesser of the submitted charge or the PPO provider contracted fee. Delta Dental Premier and Non-Delta Dental dentists: the lesser of the submitted charge or the Premier provider contracted fee. Diagnostic (deductible waived) • Exams (two per calendar year) • Bitewing x-rays (two per calendar year) Preventive (deductible waived) • Prophylaxis (cleaning) (two per calendar year and one additional cleaning for pregnant women) • Fluoride treatments (to age 19) (two per calendar year) • Sealants (to age 14) • Space maintainers (to age 14) 100% 100% 100% 100% 100% 80% 100% 80% 100% 100% 100% 100% 100% 80% 100% 80% Basic Restorative •F illings (amalgam “silver” and composite “white”non-molar) Oral Surgery •E xtraction and oral surgery procedures includingpre- and post-operative care •G eneral anesthesia and IV sedation are covered when used in conjunction with covered oral surgical procedures 50% 80% 80% 80% 80% 60% 80% 60% Not a benefit 80% 80% 80% 80% 60% 80% 60% Endodontics • Pulpal therapy • Root canal therapy Periodontics •T reatment to the gums and supporting structures of the teeth Not a benefit 80% 80% 80% 80% 60% 80% 60% Not a benefit 80% 80% 80% 80% 60% 80% 60% Major Restorative3 • Inlays • Onlays • Crowns Not a benefit Not a benefit 50% 50% 50% 50% 50% 50% Prosthodontics3 •P rocedures for replacement of missing teeth by construction or repair of bridges and partial or complete dentures Not a benefit Not a benefit 50% 50% 50% 50% 50% 50% Implants3 Not a benefit Not a benefit Not a benefit Not a benefit 50% 50% 50% 50% 50% 50% Not a benefit 50% 50% 50% $25/$75 $50/$150 $50/$150 $50/$150 $50/ $150 $75/ $225 $1,500 $2,000 $2,000 $2,000 $1,500 $1,500 $1,000 $1,500 $1,500 $1,500 $1,000 $1,000 Orthodontics3 •S traightening of teeth (children only to age 19) • $1,000 lifetime maximum (per person) Calendar year deductible (per person/per family) Calendar year maximum (per person) • Services provided by a PPO dentist • Services provided by a Premier or nonDelta Dental dentist Not a benefit $50/ $150 $75/ $225 See footnotes on page 2. 3 Delta Dental PPO Voluntary For businesses with 2-99 eligible employees Summary of Benefits1 PPO V1 Reimbursement Basis Diagnostic (deductible waived) PPO V22 PPO MPB13 PPO MPB23 Delta Dental PPO, Delta Dental Premier and NonDelta Dental dentists: the lesser of the submitted charge or the PPO provider contracted fee. 100% 100% 100% 100% 100% 100% 100% 100% 80% 80% 80% 80% 80% 80% 80% 80% 80% 80% 80% 80% 80% 80% 80% 80% Not a benefit 50% Not a benefit 50% Not a benefit 50% Not a benefit 50% • Exams (two per calendar year) • Bitewing x-rays (two per calendar year) Preventive (deductible waived) • Prophylaxis (cleaning) (two per calendar and one additional cleaning for pregnant women) • Fluoride treatments (to age 19) (two per calendar year) • Sealants (to age 14) • Space maintainers (to age 14) Basic Restorative • Fillings (amalgam “silver” and composite “white” non-molar) Oral Surgery4 • Extraction and oral surgery procedures including pre- and post-operative care • General anesthesia and IV sedation are covered when used in conjunction with covered oral surgical procedures Endodontics4 • Pulpal therapy • Root canal therapy Periodontics4 • Treatment to the gums and supporting structures of the teeth Major Restorative5 • Inlays • Onlays • Crowns Prosthodontics5 • Procedures for replacement of missing teeth by construction or repair of bridges and partial or complete dentures Implants5 Not a benefit 50% Not a benefit 50% Orthodontics Not a benefit Not a benefit Not a benefit Not a benefit $50/$150 $50/$150 $50/$150 $50/$150 $1,000 $1,000 $1,000 $1,000 Calendar year deductible (per person/per family) Calendar year maximum (per person) 1 Subject to Limitations and Exclusions on page eight. The benefit explanations contained herein are subject to all provisions of the group dental service contract, and do not modify such contract in any way, nor shall the enrollee accrue any rights because of any statement in or omission from this highlight sheet. 2 Groups with 2-4 eligible employees are limited to PPO 3, PPO Plus Premier 3 and PPO V2, and a calendar year maximum of $1,000 will apply ($1,000/$750 for PPO Plus Premier 3). 3 NY PPO Minimum Participation Base plans. 4 There is a six-month waiting period for all oral surgery, endodontics and periodontics services. The waiting period may be waived if the group can provide proof of prior comprehensive group dental coverage with no break in coverage (copy of group’s prior carrier’s EOC and last bill). 5 There is a 12-month waiting period for all major restorative, prosthodontic and implant services. The waiting period may be waived if the group can provide proof of prior comprehensive group dental coverage with no break in coverage (copy of group’s prior carrier’s EOC and last bill). 4 Delta Dental PPO Voluntary For businesses with 2-99 eligible employees Summary of Benefits1 Reimbursement Basis Diagnostic (deductible waived) PPO plus Premier V1 PPO plus Premier V2 PPO plus Premier MPB13 PPO plus Premier MPB23 Delta Dental PPO dentists: the lesser of the submitted charge or the PPO provider contracted fee. Delta Dental Premier and Non-Delta Dental dentists: the lesser of the submitted charge or the Premier provider contracted fee. 100% 100% 100% 100% 100% 100% 100% 100% 80% 80% 80% 80% 80% 80% 80% 80% 80% 80% 80% 80% 80% 80% 80% 80% Not a benefit 50% Not a benefit 50% Not a benefit 50% Not a benefit 50% • Exams (two per calendar year) • Bitewing x-rays (two per calendar year) Preventive (deductible waived) • Prophylaxis (cleaning) (two per calendar and one additional cleaning for pregnant women) • Fluoride treatments (to age 19) (two per calendar year) • Sealants (to age 14) • Space maintainers (to age 14) Basic Restorative • Fillings (amalgam “silver” and composite “white” non-molar) Oral Surgery4 • Extraction and oral surgery procedures including pre- and post-operative care • General anesthesia and IV sedation are covered when used in conjunction with covered oral surgical procedures Endodontics4 • Pulpal therapy • Root canal therapy Periodontics4 • Treatment to the gums and supporting structures of the teeth Major Restorative5 • Inlays • Onlays • Crowns Prosthodontics5 • Procedures for replacement of missing teeth by construction or repair of bridges and partial or complete dentures Implants5 Not a benefit 50% Not a benefit 50% Orthodontics Not a benefit Not a benefit Not a benefit Not a benefit $50/$150 $50/$150 $50/$150 $50/$150 Calendar year maximum (per person) • Services provided by a PPO dentist $1,500 $1,500 $1,500 $1,500 • Services provided by a Premier or non-Delta Dental dentist $1,000 $1,000 $1,000 $1,000 Calendar year deductible (per person/per family) See footnotes on page 4. 5 How the Delta Dental PPO Plan Works Delta Dental PPO plans provide access to one of the largest networks of its kind nationwide. Delta Dental PPO dentists agree to accept reduced fees as payment in full for covered procedures when treating PPO patients. This means enrollee’s out-of-pocket costs are usually lower when they visit a PPO dentist than when they visit a non-Delta Dental dentist. When covered under the PPO plan, enrollees: • • • • • Can visit any licensed dentist, including a dental specialist of choice May change dentists at any time without notifying us Can receive dental care anywhere in the world (Non-PPO benefits apply) Will not have to pay more than the patient’s share1 for covered services or file claim forms when visiting a Delta Dental dentist. Delta Dental dentists file claim forms for enrollees and accept payment directly from Delta Dental. Can visit a Delta Dental Premier dentist. Delta Dental Premier dentists will not bill above their contracted fees, but they may charge the difference between the PPO contracted fee and the Premier contracted fee. Delta Dental PPO plus Premier plans combine the PPO and Premier networks to maximize opportunities to save money. If an enrollee cannot visit a PPO dentist, the best alternative is to choose a dentist from the Delta Dental Premier network because these dentists also agree to accept limited fees for services and will not bill above the Premier contracted fees. Locating a Delta Dental PPO dentist Enrollees may visit our online directory at deltadentalins.com to find a Delta Dental PPO dentist anywhere in the U.S. For a comparative example of out-of-pocket costs that PPO enrollees might incur when visiting either a Delta Dental PPO, Delta Dental Premier or non-Delta Dental dentist, please see the hypothetical chart below: PPO Delta Dental PPO Dentist Delta Dental Premier Dentist Non-Delta Dental Dentist $180 $180 $180 $90 (PPO provider’s contracted fee) $130 (Premier provider’s contracted fee) $180 (No fee agreement with Delta Dental) Delta Dental’s payment (50%)2 $45 $45 $45 Patient’s share $45 $85 $135 Delta Dental PPO Dentist Delta Dental Premier Dentist Non-Delta Dental Dentist $180 $180 $180 $90 (PPO provider’s contracted fee) $130 (Premier provider’s contracted fee) $180 (No fee agreement with Delta Dental) Delta Dental’s payment (50%)2 $45 $65 $653 Patient’s share $45 $65 $115 Dentist bills (submitted charge) Dentist accepts as payment in full PPO plus Premier Dentist bills (submitted charge) Dentist accepts as payment in full 1 The patient’s share for covered services is their coinsurance, remaining deductible, any amount over the annual maximum, and any unpaid difference between the Premier provider’s contracted fee and the PPO contracted fee. 2 Hypothetical example for illustrative purposes assumes that the plan’s deductible has been previously satisfied, that the annual maximum has not been reached, and that benefit levels for in- and out-of-network treatment are both at 50%. 3 Non-contracted dentists are paid the lesser of the submitted fee or Premier provider contracted fee. 6 Delta Dental PPO Underwriting Guidelines Group size Businesses with 2 to 99 eligible employees. Groups with 5 or more eligible employees must initially enroll and maintain a minimum of 5 primary enrollees (2 for groups with 2-4 eligible employees) for the duration of the contract. Groups with 2-4 primary enrollees are limited to plans PPO 3, PPO Plus Premier 3 and PPO V2. Out-of-state employees Eligible employees residing out of state are allowed. Eligible industries See rate sheets for a complete list of eligible/ineligible industries. Employer contribution PPO — Employer Paid • Employer contributes at least 50% of the cost of the plan (no more than 50% contribution by employee). PPO — Voluntary and NY Minimum Participation Base • Employer contributes less than 50% of the cost of the plan (employee may contribute up to 100% towards the cost of the plan). Participation requirement PPO — Employer Paid • At least 75% of eligible employees (excluding those with dental coverage elsewhere) must enroll. • At least 50% of the employees with dependents must enroll their dependents. • All eligible dependents not covered under another group plan must be enrolled as dependent enrollees if dependent coverage is elected. PPO — Voluntary (not available in New York) • At least 25% of eligible employees (excluding those with dental coverage elsewhere) must enroll. • All eligible dependents not covered under another group plan must be enrolled as dependent enrollees if dependent coverage is elected. PPO — NY Minimum Participation Base (New York only) • At least 50% of eligible employees or two enrolled employees, whichever is fewer. • All eligible dependents not covered under another group plan must be enrolled as dependent enrollees if dependent coverage is elected. Program waiting period PPO — Employer Paid Groups with 2-24 primary enrollees • Subject to a six month waiting period from group’s effective date for major restorative, prosthodontic, implants and orthodontics (if covered) benefits. The waiting period may be waived if the group can provide proof of prior comprehensive group dental coverage with no break in coverage (copy of group’s prior carrier’s EOC and last bill). Groups with 25-99 primary enrollees • No waiting period. PPO — Voluntary and NY Minimum Participation Base (New York only) Plans • Subject to a six month waiting period for oral surgery, endodontic and periodontic services. The waiting period may be waived if the group can provide proof of prior comprehensive group dental coverage with no break in coverage (copy of group’s prior carrier’s EOC and last bill). • Subject to a 12-month waiting period for major restorative, prosthodontic and implants services. The waiting period may be waived if the group can provide proof of prior comprehensive group dental coverage with no break in coverage (copy of group’s prior carrier’s EOC and last bill). Eligible employees • Full-time, permanent employees will be entitled to receive benefits after completing all eligibility requirements of the employer. • Contract employees (category 1099 employees) are not eligible. • A group of two cannot be comprised of a dependent relationship, e.g. husband and wife. Eligible dependents • Legal spouse or domestic partner (if offered by group). • Dependent children to age 26 for all covered services, except orthodontic services. • Orthodontic treatment, if applicable, covers dependent children to age 19. New employee/ dependent enrollment • New employees must enroll within 30 days of satisfying their eligibility requirements. • Dependents must enroll within 30 days of becoming eligible. Employee or dependent terminations • Dental coverage will end on the last day of the month when an employee is no longer eligible for coverage. • Dependent coverage will end at the same time as the employee or when the dependent is no longer eligible. Waive coverage PPO — Employer–Paid • Employees or dependents can waive coverage if they have coverage elsewhere (i.e., spouse’s plan). • Participation in other coverage will count toward Delta Dental’s participation requirement. PPO — Voluntary and NY Minimum Participation Base (New York only) Plans • Employees or dependents can waive coverage. Dual choice • Employer can offer a PPO plan with a DeltaCare USA plan. • 10 or more eligible and enrolled employees – minimum of 5 in each plan. • Less than 10 eligible and/or enrolled employees – minimum of 2 in each plan (5 enrolled in DeltaCare USA in NY). When enrolling less than 5 in PPO, use the 2-4 rates. Open enrollment Employees may enroll, terminate or change coverage based on the group’s open enrollment policy. Changing Benefits Groups must wait until anniversary to change benefits. 7 Delta Dental PPO Plan Limitations and Exclusions Limitations THIS IS ONLY A BRIEF SUMMARY OF THE PLAN. The group dental service contract must be consulted to determine the exact terms and conditions of coverage. Benefits, limitations and exclusions may vary by state. 4. Treatments or supplies primarily for cosmetic purposes, except as part of a treatment dentally necessary due to accident or injury and directly attributable thereto and except for reconstructive surgery necessary because of a congenital disease or anomaly of a covered dependent child which has resulted in a functional defect. 5. Services provided or supplies furnished or devices started prior to the effective eligibility date of a patient, unless the treatment was a year in duration and was completed after the enrollee became eligible. 1. Prophylaxis and exams are a benefit twice in a calendar year. 2. Bitewing x-rays are a benefit twice in a calendar year. 3. Complete intraoral series and panoramic films are each limited to once every three years. 4. Sealants are a benefit, limited to age 14 on unfilled permanent first and second molars. Treatment with sealants as a covered service is limited to applications to eight posterior teeth. Applications to deciduous teeth or teeth with caries are not covered services. Sealants will be replaced only after three years have elapsed following any prior provision of such materials. 6. Preventive plaque control programs, including oral hygiene programs. 7. Periodontal splinting, equilibration and gnathological recordings. 8. Myofunctional therapy, unless covered by the exception in exclusion two above. Pregnant enrollees may receive an additional benefit per calendar year: one additional routine prophylaxis or one additional periodontal scaling and root planning per quadrant. Written confirmation of the pregnancy must be provided by the enrollee or her dentist when the claim is submitted. 9. Temporomandibular joint dysfunction unless covered under the group contract. 5. 6. Flouride applications are a benefit twice in a calendar year up to age 19. 7. Space maintainers are a benefit up to age 14. 8. Episodes of surgical periodontal treatment must be separated by a period of no less than three years to qualify the patient for additional periodontal benefits. 9. Substandard work until corrected. 10. Payment of any claim, bill or other demand or request for payment for health care services that the appropriate regulatory board determines were provided as a result of a prohibited referral. (Maryland only) Exclusions 1. 2. 3. 8 Treatment for materials provided in a hospital or any other surgical treatment facility unless covered under the group contract. Procedures to correct skeletal malformations, except for treatment due to accidental injury to sound natural teeth within 12 months of the accident or treatment necessary due to congenital disease or anomaly, or treatment of enamel hypoplasia (lack of development), except that this exclusion shall not apply to covered dependent children or eligible newborn children. Treatments or devices that increase the vertical dimension of an occlusion, restore an occlusion to normal, replace tooth structure lost by attrition or erosion, or otherwise, except as part of a treatment dentally necessary due to accident or injury and directly attributable thereto. 10. Implants are not a benefit under PPO 1, PPO 2, PPO plus Premier 1, PPO plus Premier 2, PPO V1, PPO MPB1, PPO plus Premier V1 and PPO plus Premier MPB1. 11. Prescription drugs, pre-medication, and relative analgesias. 12. Treatment or supplies for which the patient would have no legal obligation to pay in the absence of this or any other similar coverage. 13. Experimental procedures. 14. Anesthesia, except for general anesthesia and IV sedation given by a dentist for covered oral surgery procedures and select endodontic and periodontic procedures. 15. Major restorative services, inlays, onlays and crowns are not a benefit under PPO 1, PPO 2, PPO plus Premier 1, PPO plus Premier 2, PPO V1, PPO MPB1, PPO plus Premier V1 and PPO Plus Premier MPB1. 16. Prosthodontic services, including bridges and dentures, are not a benefit under PPO 1, PPO 2, PPO plus Premier 1, PPO plus Premier 2, PPO V1, PPO MPB1, PPO plus Premier V1 and PPO plus Premier MPB1. 17. Orthodontic services, including tooth guide appliances, are not a benefit under PPO 1, PPO 2, PPO 3, PPO plus Premier 1, PPO plus Premier 2, PPO plus Premier 3, PPO V1, PPO MPB1 PPO V2, PPO MPB2, PPO plus Premier V1, PPO plus Premier MPB1, PPO plus Premier V2 and PPO plus Premier MPB2. 18. Endodontics, periodontics and oral surgery are not a benefit under PPO 1 and PPO plus Premier 1. 19. Adult orthodontics. DeltaCare USA1 Sample Procedures3 For businesses with 22 - 99 eligible employees with and without Employer Contribution Sample Patient Copayments PLAN 13A PLAN 15A PLAN M73 (Not available in New York) Prophylaxis cleaning — adult (one per six month period) D1110 No cost $5 No cost Bitewing — single radiographic image D0270 No cost No cost No cost Bitewings — four radiographic images — limited to 1 series every 6 months D0274 No cost No cost $20 Topical application of fluoride — excluding varnish — child — to age 19; one per six month period D1208 No cost No cost No cost Amalgam two surfaces, primary or permanent D2150 No cost $12 $48 Extraction, coronal remnants — deciduous tooth D7111 No cost $10 $45 Sealant, per tooth — limited to permanent molars through age 15 D1351 $10 $15 $15 Periodontal scaling and root planing — one to three teeth per quadrant D4342 $40 $50 $60 Crown — full cast noble metal D2792 $295 $335 $465 Root canal — endodontic therapy, molar (excluding final restoration) $335 $365 $470 $285 $365 $600 Comprehensive orthodontic treatment of the transitional dentition — child or adolescent to age 19 D8070 $1,900 $1,900 75 percent of the contract orthodontist’s “filed fee” Comprehensive orthodontic treatment of the adult dentition — adults, including covered dependent adult children D8090 $2,100 $2,100 75 percent of the contract orthodontist’s “filed fee” D3330 Complete denture — maxillary D5110 1 2 3 DeltaCare USA is not available in Delaware. In New York, groups must initially enroll and maintain a minimum of 5 primary enrollees for the duration of the contract. 2016 Current Dental Terminology codes under copyright by the American Dental Association (ADA). Subject to Limitations and Exclusions beginning on page 12. A complete listing of procedures and copayments, as well as benefit frequency limitations, may be found in the Description of Benefits and Copayments (available upon request). Benefits The following are included in all three DeltaCare USA plans: • • • • • • No claim forms No deductibles No annual maximums Access to specialty care Professional treatment standards Out-of-pocket costs are clearly defined DeltaCare USA enrollees must select a contract dental office in the state where the group is headquartered to provide care for themselves and their families. The low turnover rate among DeltaCare USA dentists means enrollees can enjoy a long-term relationship with their family dentist. 9 Using The DeltaCare USA Plan DeltaCare USA promotes great dental health for enrollees and their families with quality dental benefits at an affordable cost. By covering many services at no cost to the enrollee, Delta Dental encourages regular preventive dental visits. Enrollees must select a contracted DeltaCare USA dentist to provide covered services. DeltaCare USA enrollees also enjoy great features including out-of-area emergency coverage, an orthodontic treatment in progress provision and expanded business hours for toll-free customer service (subject to Limitations and Exclusions). When covered by a DeltaCare USA plan, enrollees: • • • • • • Won’t be subject to annual deductibles or maximums; Will know in advance what out-of-pocket costs will be; Won’t be subject to restrictions on pre-existing conditions, except for work in progress; Won’t have to complete claim forms and submit them for reimbursement; Will be covered for accidental injury based on procedures listed in the Description of Benefits and Copayments; and Will receive a plan in which all listed procedures are covered with set fixed copayments. Know the name and location of a DeltaCare USA dentist Enrollees must select and obtain treatment from a primary care dentist listed on DeltaCare USA’s participating dental offices in the state where the group is headquartered. If enrollees change their DeltaCare USA dentist by the 21st of the month, the change will be effective on the first day of the following month. If the dentist’s network status changes, Delta Dental will notify the enrollee, but they should verify their dentist’s status with us by calling Customer Service or by visiting our web site — deltadentalins.com. How the plan works Following enrollment in DeltaCare USA, enrollees will receive an ID card and a plan booklet. The booklet contains a complete list of the procedures and copayments that are covered for the DeltaCare USA plan, as well as plan limitations and exclusions. Delta Dental will also include in the packet the name, address and phone number of the enrollees’ DeltaCare USA dentist. Enrollees simply call the dental office to make an appointment. We will notify the DeltaCare USA dentist about the enrollees’ enrollment in the plan, as well as other important details about enrollee coverage such as dependent information, group number and enrollee ID number. One of the great features of the plan is that enrollees have a list of the copayments and covered services so they can always refer to it before visiting the dentist. Orthodontic treatment in progress DeltaCare USA has an orthodontic treatment in progress provision that allows new enrollees to continue treatment with their current orthodontist, so long as the enrollee is in active treatment started under his or her previous employer-sponsored dental plan. Enrollees are responsible for all copayments and fees subject to the provisions of their prior dental plan. 10 DeltaCare USA Underwriting Guidelines Group size Businesses with 2 to 99 eligible employees (5 to 99 in New York). Group must initially enroll and maintain a minimum of 2 primary enrollees (5 in New York) for the duration of the contract. Eligible industries See rate page for a list of eligible/ineligible industries. Employer contribution Employer will provide payroll deduction for employee contributions. With employer contribution • Employer contributes at least 25% of the cost of the plan. Without employer contribution — Voluntary • Employer may contribute up to 24.9% of the cost of the plan. Participation requirement Employee • A minimum of 2 primary enrollees (5 in New York) must enroll. Dependent • Dependents are not required to enroll. • All eligible dependents not covered under another group plan must be enrolled as dependent enrollees if dependent coverage is elected. Eligibility waiting period As required by employer. Program waiting period No waiting period for any services. Eligible employees • Full-time, permanent employees will be entitled to receive benefits after completing all eligibility requirements of the employer. • Contract employees (category 1099 employees) are not eligible. • A group of two cannot be comprised of a dependent relationship; e.g., husband and wife. New employee/ dependent enrollment • New employees must enroll within 30 days of satisfying their eligibility requirements. • Dependents must enroll within 30 days of becoming eligible. Eligible dependents • Legal spouse or domestic partner (if offered by group). • Dependent children to age 26. Employee or dependent terminations • Dental coverage will end on the last day of the month when an employee is no longer eligible for coverage. • Dependent coverage will end at the same time as the employee’s or when the dependent is no longer eligible. Waive coverage Employees or dependents can waive coverage. Orthodontics Immediately available to new groups without proof of prior orthodontic coverage. Dual choice • Employer can offer a PPO plan with a DeltaCare USA plan. • 10 or more eligible and enrolled employees – minimum of 5 in each plan. • Less than 10 eligible and/or enrolled employees – minimum of 2 in each plan (5 enrolled in DeltaCare USA in NY). When enrolling less than 5 in PPO, use the 2-4 rates. DeltaCare USA dentist • Enrollees must select and obtain treatment from a primary care dentist listed on DeltaCare USA’s participating dental offices in the state where the group is headquartered. Open enrollment Employees may enroll, terminate or change coverage based on the group’s open enrollment policy. Out-of-state employees Out-of-state employees are covered by the plan. However, services must be rendered in the state where the contract is issued, except New York and Pennsylvania contracts where services must be rendered in New York, Pennsylvania or New Jersey. Changing Benefits Groups must wait until anniversary to change benefits 11 DeltaCare USA Limitations of Benefits Limitations THIS IS ONLY A BRIEF SUMMARY OF THE PLAN. The group dental service contract must be consulted to determine the exact terms and conditions of coverage. Benefits, limitations and exclusions may vary by state. 1. The frequency of certain benefits is limited. All frequency limitations are listed in Description of Benefits and Copayments, available upon request: 2. If the enrollee accepts a treatment plan from the general dentist that includes any combination of more than six crowns, bridge pontics and/or bridge retainers, the enrollee may be charged an additional ($100.00 for plans 13A and 15A) or ($75.00 for plan M73) above the listed copayment for each of these services after the sixth unit has been provided; 3. General anesthesia and/or intravenous sedation/ analgesia is limited to treatment by a contracted oral surgeon and in conjunction with an approved referral for the removal of one or more partial or full bony impactions, (Procedures D7230, D7240, and D7241); 4. For plans 13A and 15A, benefits provided by a pediatric dentist are limited to children through age seven following an attempt by the assigned contract dentist to treat the child and upon prior authorization by the plan less applicable copayments. Exceptions for medical conditions, regardless of age limitation will be considered on an individual basis. For plan M73, benefits provided by a contract pediatric dentist are available at 75 percent of the contract specialist’s “filed fees.” Referral by the assigned contract dentist is required before services are rendered; 5. The cost to an enrollee receiving orthodontic treatment whose coverage is cancelled or terminated for any reason will be based on the contract orthodontist’s usual fee for the treatment plan. The contract orthodontist will prorate the amount for the number of months remaining to complete treatment. The enrollee makes payment directly to the contract orthodontist as arranged; Maryland Only: Should an enrollee’s coverage be cancelled or terminated for any reason, and at the time of cancellation or termination the enrollee is receiving orthodontic treatment, the enrollee will be solely responsible for payment for treatment provided after cancellation or termination, except: If an enrollee is receiving ongoing orthodontic treatment 12 at the time of termination, ALPHA will continue to provide orthodontic benefits for: — 60 days if the enrollee is making monthly payments to the contract orthodontist, or — until the later of 60 days or the end of the quarter in progress, if the enrollee is making quarterly payments to the contract orthodontist. At the end of 60 days (or at the end of the quarter), the enrollee’s obligation will be based on the contract orthodontist’s usual fee for the treatment plan. The contract orthodontist will prorate the amount over the number of months remaining in the initial 24 months of treatment. The enrollee will make payments based on an arrangement with the contract orthodontist. 6. Orthodontic treatment in progress is limited to new DeltaCare USA enrollees who, at the time of their original effective date, are in active treatment started under their previous employer sponsored dental plan as long as they continue to be eligible under the DeltaCare USA program. Active treatment means tooth movement has begun. Enrollees are responsible for all copayments and fees subject to the provisions of their prior dental plan. The plan is financially responsible only for amounts unpaid by the prior dental plan for qualifying orthodontic cases. 7. Pennsylvania Only: A pre-existing condition is a disease or physical condition caused by illness or injury for which medical advice or treatment has been received within 90 days immediately prior to becoming eligible with the DeltaCare USA program. A pre-existing condition shall be covered after an enrollee has been covered for more than 12 months under the group contract. Example: teeth prepared for crowns, root canals in progress, orthodontic treatment. If an enrollee begins comprehensive orthodontic treatment within 90 days immediately prior to becoming eligible under the DeltaCare USA program, a provision for treatment in progress is available, subject to a waiting period of 12 months of continuous coverage under the DeltaCare USA program unless the individual qualifies for the onetime orthodontic treatment in progress provision. DeltaCare USA Exclusions of Benefits Exclusions 1. Any procedure that is not specifically listed under Description of Benefits and Copayments , available upon request: 2. Any procedure that in the professional opinion of the contract dentist: a.has poor prognosis for a successful result and reasonable longevity based on the condition of the tooth or teeth and/or surrounding structures, or b.is inconsistent with generally accepted standards for dentistry; 3. Services solely for cosmetic purposes, with the exception of procedure D9972, external bleaching, per arch, or for conditions that are a result of hereditary or developmental defects, such as cleft palate, upper and lower jaw malformations, congenitally missing teeth and teeth that are discolored or lacking enamel, except for the treatment of newborn children with congenital defects or birth abnormalities; 4. Porcelain crowns, porcelain fused to metal, cast metal or resin with metal type crowns and fixed partial dentures (bridges) for children under 16 years of age; 5. Lost or stolen appliances including, but not limited to, full or partial dentures, space maintainers and crowns and fixed partial dentures (bridges); 6. Procedures, appliances or restoration if the purpose is to change vertical dimension, or to diagnose or treat abnormal conditions of the temporomandibular joint (TMJ); 7. Precious metal for removable appliances, metallic or permanent soft bases for complete dentures, porcelain denture teeth, precision abutments for removable partials or fixed partial dentures (overlays, implants, and appliances associated therewith) and personalization and characterization of complete and partial dentures; 8. Implant-supported dental appliances and attachments, implant placement, maintenance, removal and all other services associated with a dental implant; 9. Consultations for non-covered benefits; 11. Under plan M73 dental services received from any dental facility other than the assigned contracting dentist, including the services of an out-of-network dentist who provides specialized services are excluded unless expressly authorized by the Administrator, or as covered under Emergency Services as described in the Contract and/or Evidence of Coverage (EOC). 12. All related fees for admission, use, or stays in a hospital, out-patient surgery center, extended care facility, or other similar care facility; 13. Prescription drugs; 14. Dental expenses incurred in connection with any dental or orthodontic procedure started before the enrollee’s eligibility with the DeltaCare USA program. Examples include: teeth prepared for crowns, root canals in progress, full or partial dentures for which an impression has been taken and orthodontics unless qualified for the orthodontic treatment in progress provision;1 15. Lost, stolen or broken orthodontic appliances; 16. Changes in orthodontic treatment necessitated by accident of any kind; 17. Myofunctional and parafunctional appliances and/or therapies; 18. Composite or ceramic brackets, lingual adaptation of orthodontic bands and other specialized or cosmetic alternatives to standard fixed and removable orthodontic appliances; 19. Treatment or appliances that are provided by a dentist whose practice specializes in prosthodontic services.2 1 Does not apply in Pennsylvania. 2Does not apply in Maryland. 10. Under plans 13A and 15A, dental services received from any dental facility other than the assigned contracting dentist, a preauthorized dental specialist, or a contract orthodontist are excluded, except for Emergency Services as described in the Contract and/ or Evidence of Coverage (EOC). 13 Value Proposition We keep you smiling® Why do 68 million enrollees trust their smiles to Delta Dental?1 Most of our enrollees stay with us year after year2, and it’s no wonder. Delta Dental sets the industry standard by doing whatever it takes and then some. We deliver: •Less out-of-pocket. The Delta Dental Difference® saves clients and enrollees billions of dollars a year.3 Because Delta Dental dentists agree to our determination of fees, clients enjoy extensive cost controls, and enrollees pay less out-of-pocket. •More dentists. Four out of five dentists4 nationwide are contracted Delta Dental dentists, giving enrollees convenient access and quality assurance through one of the nation’s largest dentist networks. •Simpler process. Our dental plans are easy to use. No ID card is required to receive services and there are no claim forms to file — Delta Dental dentists do that for you. And because we pay Delta Dental dentists directly, you are responsible only for your share of payment. 1Delta Dental of California, Delta Dental of New York, Inc., Delta Dental of Pennsylvania, Delta Dental Insurance Company and our affiliated companies form one of the nation’s largest dental benefits delivery systems, covering 33 million enrollees. All of our companies are members, or affiliates of members, of the Delta Dental Plans Association, a network of 39 Delta Dental companies that together provide dental coverage to almost 68 million people in the U.S. 2Delta Dental retained 95.7 percent of our 33 million enrollees in 2014. 3Savings due to reduction of premiums or claims liability and patient out-of-pocket costs, based on Delta Dental’s cost management report, 2014. 4Proportion of total practicing dentists contracted with Delta Dental based on the Delta Dental Plans Association National Provider File, 2015. 14 Delta Dental’s Mission Statement To advance dental health and access through exceptional dental benefits service, technology and professional support. 15 Call your broker, participating general agent or Delta Dental Delta Dental’s toll-free number 800-471-7091 Or write to Delta Dental at: One Delta Drive Mechanicsburg, PA 17055 [email protected] Delta Dental PPOSM Delta Dental Premier® and Delta Dental PPO® is underwritten by Delta Dental Insurance Company in DC, and by not-for-profit dental service companies in these states: PA and MD — Delta Dental of Pennsylvania; NY — Delta Dental of New York, Inc.; DE — Delta Dental of Delaware, Inc.; WV — Delta Dental of West Virginia. DeltaCare® USA DeltaCare USA is underwritten in these states by these entities: DC and WV — Delta Dental Insurance Company; MD — Alpha Dental Programs, Inc.; NY — Delta Dental of New York, Inc.; PA — Delta Dental of Pennsylvania; Delta Dental Insurance Company acts as the DeltaCare USA administrator in all these states. These companies are financially responsible for their own products. Visit Delta Dental’s website at: deltadentalins.com © Delta Dental SBA DDP #89479 (rev. 8/15)