* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Peyronies disease
Survey
Document related concepts
Transcript
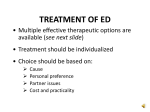
World J Urol (2001) 19: 244±250 Ó Springer-Verlag 2001 FREE PAPER Hari Siva Gurunadha Rao Tunuguntla Management of Peyronie's disease ± a review Abstract Peyronie's disease is an uncommon condition involving middle-aged men and probably resulting from penile trauma. The injury causes an in¯ammation in the tunica and ultimately scarring and penile curvature develop. It may also occur due to nonspeci®c in¯ammation. The use of medications such as b-blockers can sometimes result in Peyronie's disease. In Peyronie's disease, the normal elastic tissue of the tunica is replaced by scar tissue. The penile plaque, or scar tissue in this condition, is not elastic but hard and will not stretch with erection. The side that does not stretch results in penile curvature to the side of the scar. One third of men with Peyronie's disease have painful erections. A low percentage of men with Peyronie's disease develop erectile dysfunction. Because in¯ammation is initially associated with the scar tissue, some amount of discomfort occurs during erection. Most patients with early stage Peyronie's disease can continue to function sexually with the curvature in the penis. Others with a severe penile deformity will have diculty in sexual intercourse. Literature regarding the eectiveness of conservative therapy in the early phase with pain and in¯ammation is limited, with only modest and at times anecdotal bene®ts. The commonly used agents include 400 units of vitamin E (vitamin E promotes healing and prevents scarring), ibuprofen (anti-in¯ammatory) and Colchicine (useful for pain during erection). Fexofenadine is recently being used in the early phase of Peyronie's disease for its antiin¯ammatory eect. Radiation and ultrasound are not usually very helpful. When the disease process stops, there is usually some residual distortion of the penis but H. S. G. R. Tunuguntla 1624, SW 40th Terrace, Apt. D, Gainesville, FL 32607±4086, Florida, USA e-mail: [email protected] Tel.: +1-352-3841817 H. S. G. R. Tunuguntla North Florida Urology Research Institute, 6440, West Newberry Road, Suite 410, Gainesville, FL 32605, USA the majority of patients are able to have satisfactory sexual intercourse. However, if there is severe penile distortion interfering with intercourse, surgery is indicated. Surgical techniques for Peyronie's disease include tightening or plication (Nesbit's tuck) of the penis opposite the curvature to produce straightening. This usually results in some small loss of length. The other type of surgery consists of incision of the plaque or scar tissue and patching with a vein (saphenous vein graft) or dermal graft. Laser therapy is occasionally used. A penile prosthesis is the treatment of choice in patients with Peyronie's disease and erectile dysfunction. Peyronie's disease (PD) is a localized connective tissue disorder of the tunica albuginea of the penis, which results in a severe curvature of the erect penis. The cause of this condition is not completely understood at present [29]. The condition was named after FrancËois Gigot de la Peyronie, the personal physician of King Louis XVI of France. Common presenting complaints of PD include palpable penile plaque, painful erections, and curvature of the penis. It is a psychologically debilitating problem, and aicted men demonstrate a signi®cantly reduced quality of life. Studies are currently underway regarding the exact cause of this disorder. A minor bend (about 10°) in the erect penis is normal. A signi®cant percentage of patients with Peyronie's disease have erectile dysfunction either as a result of the Peyronie's disease or in association with it. In some patients with Peyronie's the penis can form a J or a corkscrew, making intercourse impossible. Statistics [41] Statistically, PD shows the following: ± Occurs in 0.38%±3% of the adult male (40±60 years) population. 245 ± Occurs in 1.5% in men in the 30±39-year age group. ± Occurs in 6.5% in men older than 70 years. ± Approximately 40% of men with PD have some evidence of erectile dysfunction Characteristics of PD in young men include a past history of trauma during sexual intercourse and painful erections. Medical therapy is commonly used for painful erections in this subset of patients, although it is not eective in all patients. Structure of the penis [27] The penis is composed of three cylindrical structures, two on the dorsum, called the corpora cavernosa (cavernous spaces, blood-®lled spaces which expand and trap the blood during erection), and one on the ventrum, the corpus spongiosum (along with the urethra). The corporal bodies are surrounded by an elastic covering called the tunica albuginea. The nerves and blood vessels (dorsal artery and veins) of the penis are located on the dorsal aspect of the corpora cavernosa. The tunica of the corpus cavernosum is a 2-layered structure. The inner layer, with its circularly oriented ®bers, has supportive function and surrounds the cavernous tissue. Intracavernosal pillars (ICPs) radiate inwards from the inner layer and augment the support provided by the septum (the main structure providing support to the erectile tissue of the corporal bodies). The ®ber bundles of the outer layer are oriented longitudinally extending from the glans penis to the proximal crura and insert into the inferior pubic ramus. These ®ber bundles are, however, are absent at the 6 o'clock positions. The tunica albuginea consists of elastic ®bers forming an irregular network of elastic ®bers and collagen ®bers. Emissary veins travel between the inner and outer layers and obliquely pierce the outer ®bers. The tunica aords great ¯exibility, rigidity and tissue strength to the penis during erection, with its outer layer compressing the veins. Branches of the dorsal artery of the penis travel within the penis in a perpendicular direction, surrounded by a periarterial ®brous sheath. The corpus spongiosum is a low-pressure structure during erection due to the absence of an outer investing layer and the intracorporeal struts, speci®c to the corpora cavernosa. Internal pudendal artery (a branch of the hypogastric artery) is the main arterial supply to the penis and becomes the common penile artery after giving o the perineal branch in Alcock's canal. The penile artery gives 3 branches: bulbourethral artery (which supplies the urethral bulb, the spongiosum and the glans penis), cavernous (deep or central) artery of the penis (which supplies the erectile tissue of the corpora cavernosa) and the dorsal artery (which supplies the glans penis, penile skin and subcutaneous tissue). Collaterals among the cavernosal, dorsal, and urethral arteries run along the length of the penis. Proximal to the glans, the three arteries converge to form a vascular ring. Accessory pudendal arteries sometimes originate from vesical, obturator or external iliac arteries, which may explain the postoperative vascular impotence following radical cystectomy and prostatectomy. In the ¯accid penis, most of the penile arterioles are in a constricted state (30 lm in diameter). The sinusoids and their interconnecting channels are also in a constricted state due to contracted cavernous muscles. The intrinsic tone, coupled with the sympathetic innervation is believed to contribute to the cavernous muscle contraction in the ¯accid penis. Regarding venous drainage, the emissary veins of the corpora cavernosa drain into four groups of veins: dorsal, right lateral, left lateral and ventral. These groups of veins form circum¯ex, deep dorsal, cavernous, and crural veins. The deep dorsal vein primarily drains the glans penis, whereas in the mid and distal shaft, the emissary veins either empty directly into the deep dorsal vein or drain through ®ve to ten sets of circum¯ex veins into the deep dorsal vein (which subsequently drains into the periprostatic venous plexus). The base and hilum of the corpora cavernosa drain into many cavernous and crural veins, which join the periurethral vein and form the internal pudendal vein. The super®cial dorsal vein primarily drains the skin and subcutaneous tissue of the penis. Communications exist between the super®cial dorsal, deep dorsal, and cavernous veins of the penis. Venous drainage of the penis begins as tiny venules from sinusoidal spaces, which merge into the subtunical venous plexus. The emissary veins (approximately 100 lm) then originate from the subtunical venous plexus. Physiology of erection [27] The sinusoids become distended during erection from the arterioles and capillaries. The arterioles open directly into the sinusoidal spaces and the capillaries supply the connective tissue framework. In the ¯accid state, the terminal arterioles are tortuous and contracted, whereas during erection the arterioles and the main cavernous artery become dilated and straight. In the ¯accid state, the venous channels remain open due to the constricted sinusoids. During erection, on the other hand, the expanded sinusoids compress the tiny venules in the trabeculae between them. With increasing tumescence, expansion of the sinusoidal system against the noncompliant tunica albuginea further compresses the subtunical venous plexuses. At full erection, the unequal stretch of the inner circular and outer longitudinal tunical layers further reduce the venous ¯ow to a minimum. 246 Risk factors Local penile trauma during aggressive sexual intercourse is a well-identi®ed cause for PD. The presence of the HLA antigen, DRW 52 (commonly found in patients with certain autoimmune disorders) has been found to be associated with PD. PD has been found to be associated with certain autoimmune diseases such as SjoÈgren's syndrome, BehcËet's disease, systemic sclerosis, and systemic lupus erythematosus (SLE). Pathophysiology and mechanism of injury [2, 10, 15, 20, 36] PD has a multifactorial etiology. Repetitive microtrauma of the penis during sexual intercourse is thought to incite a local autoimmune reaction in genetically susceptible individuals. Penile trauma acts as an initiating factor in the majority of young men with PD [4]. Abnormal healing of tissue injury along with progressive chromosomal instability then results in PD. Altered composition of certain tissue proteins in the extracellular matrix (such as decorin, biglycan, ®bromodulin, gelatinase A, and collagenase II) in the tunica albuginea of men with PD has been identi®ed, suggesting an abnormal remodeling process following tissue injury [2, 10, 15, 36]. Some studies have found that levels of the enzyme, nitric acid synthase (NOS) are also diminished in the cavernous tissue of the penis in patients with PD. Normal levels of this enzyme are essential for normal penile erection. Diminished local concentration of this enzyme may be one of the causes of erectile dysfunction in PD [29]. The disease is thought to result when blood leaks (from penile trauma during intercourse/penile fracture) from the corpora cavernosa during erection and accumulates between the layers of the tunica albuginea, resulting in excessive scar tissue production, and a plaque formation [20]. This leakage of blood most often occurs where the septal ®bers attach to the under surface of the tunica albuginea, and this accounts for the most frequent location of the plaque in the dorsal midline and along the septum. Young men have strong elastic tissues that resist injury. Old men have weak tunica that tears, but their erections are also weak and consequently injury does not occur. In contrast, middle-aged men begin to lose the elastic strength of their corporeal tissues and at the same time maintain fairly strong erections making injury likely. Injury may occur suddenly (in 1/3 of patients). In the other two-thirds of cases injury may occur gradually over a period of time, and these patients have a more gradual onset and slow progression of the disease (classical PD). Men who sustain traumatic rupture of the tunica albuginea (fractured penis) experience sudden pain when the penis is forcibly bent during erection. They then have penile swelling and ecchymosis (local collection of clotted blood). If the defect in the tunica albuginea is not repaired surgically, it will heal but a large scar or plaque forms. This post-penile fracture penile plaque is located laterally at the base of the penis. Plaque distribution The most common location for plaque in PD is the dorsal midline resulting in an upward bend of the erect penis. The next most common site is a dorsal midline plaque with septal extension. The plaque may also extend from the dorsal midline circumferentially around the corporeal bodies. Rarely, the plaque may be seen between the corpus spongiosum and the ventral surface of the corpora cavernosa. A dorsal plaque and a ventral plaque may connect through septal extensions to form an I-beam. Peyronie's disease and erectile dysfunction A signi®cant percentage of patients with PD have erectile dysfunction. The erectile dysfunction may be a result of PD or may be occurring simultaneously. The causes of erectile dysfunction in PD include psychological factors (performance anxiety), penile pain and deformity (especially if it is ventral or lateral) preventing coitus, ¯ail penis/lack of tumescence due to cavernosal ®brosis and penile vascular (arterial and/or venous) disease. Diminished elastic ®ber content of the tunica along with increased type III (immature) collagen may contribute to veno-occlusive dysfunction in PD [7, 42]. In the acute in¯ammatory phase, patients suer from pain during ¯accidity and/or during erection and sexual intercourse. In addition to pain, a predominantly dorsal penile deviation is the main symptom; in later stages it is often associated with erectile dysfunction and/or distal ¯accidity [47]. The anxiety associated with PD may trigger functional impotence; these patients may be referred to a sex therapist and/or be treated with sildena®l citrate. In addition, a mild erectile deformity may precipitate some mechanical diculties during coitus. The patient should be given reassurance and suggestions such as the use of a water-soluble lubricant, elevation of the partner's hips on a pillow, and manual guidance of the penis for vaginal penetration. Diagnosis The ability of the patient to obtain and maintain an erection should be determined, and any problems with vaginal penetration or thrusting should be noted [1, 17, 22, 25, 35, 37]. If chordee (curvature) is present, the 247 patient should be asked to describe the direction and extent (estimated in degrees). Any other erectile deformity should also be noted. This is best achieved with a polaroid picture when the patient gets an erection. On physical examination the penis should be stretched out and a careful examination for plaque should be performed. The number, size, and location of plaques are recorded, and whether the plaques are sharply demarcated. Intracorporal injections of vasoactive drugs (Prostaglandin E1, Papaverine) are used to produce erections, and if a full erection is not obtained after injection, visual sexual stimulation (VSS) can be used. This allows the urologist to examine the erect penis and to note the type and extent of erectile deformities (Fig. 1). If an erection cannot be produced in the oce, the clinician can ask the patient to make a polaroid photo of his erect penis at home. Penile ultrasound can be useful in determining the location and extent of plaque; however, not all plaque is readily visualized by ultrasound and magnetic resonance imaging (MRI) may be better in this regard. Contrast-enhanced MRI is especially useful for a detailed assessment of the plaque prior to surgical intervention in extensive PD. Objective evaluation of erectile function is achieved by assessment of penile arterial in¯ow (and arterial collaterals), venous out¯ow and resistive indices (factors useful in selecting patients with PD who can bene®t from surgery for erectile dysfunction) by nocturnal penile tumescence (NPT) testing and duplex ultrasound (after injection of 10 mcg of PG-E1) [1, 17, 25, 35, 37]. In a study by Kadioglu and associates, color Doppler ultrasonography (CDU) revealed penile vascular abnormalities in 76.5% of patients with PD. Veno-occlusive dysfunction (VOD) was observed in 40% of men with normal erection (based on history), whereas mixed (arterial + venous) vascular disease was diagnosed in 10% [22]. In those who presented with erectile dysfunction, penile vascular disease was detected in 87.5% patients (VOD in 28%, arterial disease in 9.3% and mixed vascular disease in 50%). The prevalence of arterial disease on CDU among PD patients with erectile dysfunction (59.3%) was found to be signi®cantly higher than that among patients with normal erection (10%). The prev- alence of pure VOD was, however, similar in those with or without erectile dysfunction. Penile vascular abnormalities were observed in 76.5% of PD patients by CDU and this ratio increased to 87.5% in patients with erectile dysfunction by history. In addition, arterial disease accounted for much of the diminished rigidity in those with PD. Careful documentation of the type and extent of erectile deformity is important not only to plan therapy but for medicolegal reasons as well. NPT studies, color/ duplex ultrasound examinations of the penile arteries and MRI of the plaque are, therefore, helpful in identifying PD patients most likely to bene®t from the different surgical options currently available, such as penile plaque excision, penile straightening procedures, and penile prostheses. For example, patients with penile deformity combined with vasculogenic erectile dysfunction are best treated by implantation of penile prosthesis. Treatment Many patients with PD may not have symptoms and reassurance that the palpable lesion is not cancer is all that is necessary. Treatment is indicated only when penile pain (an indication of early disease) or deformity is troublesome. Medical treatment Stabilization of the condition may require approximately 6 months [8, 12, 14, 16]. There is, therefore, a waiting period between diagnosis and the decision to start de®nitive surgical treatment. The condition usually evolves over a period of time and in some patients it can resolve or improve spontaneously without treatment. Remission of PD in the early stage has been reported in approximately 40%, overall spontaneous regression in 13%, stable disease in 47%, and progression in 40% of patients [12, 14, 36]. Nonoperative treatment of Peyronie's disease Fig. 1 Penile curvature (chordee) in Peyronie's disease Conservative treatment is useful during the early in¯ammatory and painful stage of the disease. No causal therapy is currently available due to the lack of concrete knowledge regarding its etiology. Nonoperative treatment is mainly symptom-directed and mostly of questionable ecacy as no placebo controlled double blind trials are available to date [8]. Agents tried include vitamin E, p-aminobenzoate, orgotein (super oxide dismutase), clostridial collagenase, procarbazine, dimethylsulfoxide (DMSO), parathyroid hormone, b-aminopropionitrile, a-chymotrypsin, colchicines, tamoxifen, nonspeci®c antihistamines such as terfenadine and fexofenadine, and systemic steroids 248 [11, 17, 31, 37, 44]. However, only vitamin E and potassium p-aminobenzoate were found to be useful [48]. Vitamin E is the traditional treatment of choice for PD. It is easy to take, cheap, free of side eects and better than placebo for treating the pain. It is used in a dose of 400 mg twice daily. Vitamin E acts by its free radical scavenging eect [3, 5, 37, 40, 43]. Para-aminobenzoate (Potaba) has been found to be bene®cial in patients with noncalci®ed plaques. It is effective in a dose of 12 g per day (twenty four 500 mg tablets or six 2 gram packets). In a retrospective review of 32 patients treated for at least 3 months, Carson reported improvement in penile discomfort in eight, decreased plaque size in 18, and improvement in penile angulation in 18 [6]. However, this agent is very expensive, unpleasant to take and the recommended dose may be associated with signi®cant gastrointestinal side eects [26]. Potaba is to be taken for 12 months, which allows time for the disease to stabilize and patients with persisting symptoms may then be candidates for surgical treatment. When the disease reaches the mature stage with curvature of the penis resulting in erectile dysfunction, surgical correction is indicated after a preliminary evaluation for impotence with duplex Doppler study, dynamic infusion pharmacocavernosometry and cavernosography (DICC) with/without nocturnal penile tumescence (NPT) testing. Early stage disease is more likely to respond to medical therapy compared to long-standing Peyronie's plaques. Most authorities currently recommend a trial of medical therapy with a safe, inexpensive and welltolerated agent [17]. Other forms of treatment These include radiation therapy, diathermy, laser treatment, ultrasound therapy, local injection of interferon a-2b, dexamethasone, calcium channel blockers (verapamil), superoxide dismutase and collagenase into the plaque, and iontophoresis ± rubbing of agents such as steroids/histamine on the penis, the drug gets absorbed through the skin and subcutaneous tissue [34, 35]. Recently iontophoresis with a combination of dexamethasone, lidocaine and verapamil has been reported to yield pain relief in 96% of patients and improvement in penile deviation in 37% in patients with a short history of disease [39]. Intralesional injection of verapamil: 10 mg of verapamil is diluted in 10 cc of normal saline and injected throughout the plaque every 2±4 weeks for a total of 6± 12 injections. A decrease in penile curvature has been reported in 61% of the patients (range, 10±40°), an increase in penile curvature in 8.3%, and no change in 31%. Improved sexual performance has been reported in 91% of treated men. There were no recurrences over a follow-up period of 6 years. [23]. None of the intralesional agents has been shown to have a long-term eect in a controlled trial till date [8]. Current medical therapy (including vitamin E and p-aminobenzoate) for PD results in symptomatic relief only in some patients with painful and prolonged early stage of the disease with active in¯ammation. Local radiation may sometimes be eective in relieving penile pain and discomfort. Recently, extracorporeal shock waves (ESWT) were used to noninvasively target the plaque of PD [19, 30]. The mechanism of action of ESWT in PD is twofold: direct damage to the plaque and increased vascularity of the plaque (by local heat generation), which results in local in¯ammatory reaction, lysis of the plaque, and removal by phagocytic cells (macrophages). Each patient is treated with a minimum of three sessions of ESWT (3000 shock waves at an energy density of 0.11±0.17 mJ/sq mm) at 3-week intervals. Over a mean follow-up of 7.5 months (range, 5±11 months), 47% of the patients have reported an improvement in penile angulation (mean reduction, 29.3°) (range, 10±60°). Sixty percent of patients with pain on erection report immediate relief (mean reduction on the visual analog scale, 2.3) (range, 1±4). No adverse eects are reported except minimal bruising at treatment site. In those with disease duration <12 months, ESWT results in signi®cant improvement in both pain and angulation. However, the treatment is more eective in reducing penile angulation in those with long standing disease (>12 months) [19, 30]. Surgical treatment The surgical management of PD consists of either correction of the penile deformity (once the disease is fully stable) or the insertion of a penile prosthesis in those with a concomitant erectile dysfunction. The various operations are discussed below, but the choice rests between a Nesbit-type procedure and the implantation of a penile prosthesis. The mere presence of a lump or a minor erectile deformity is not an indication for surgery. Indications for surgery in PD with and without erectile dysfunction Currently, there is no clear-cut evidence as to when (i.e., at which stage of the disease) semi-invasive and surgical procedures are indicated, although it is believed that conservative therapy is indicated in the earlier in¯ammatory and painful stage [8]. The role of conservative therapy in nonresponders to drug therapy and for those with calci®ed plaques who do not want surgery, remains unanswered. In contrast to this, surgery (e.g., penile straightening with or without plaque excision) can be performed in patients with severe penile angulation without loss of erection [24]. In those with PD and erectile dysfunction, insertion of penile prosthesis is the ®rst-line therapy [24]. Many such patients, in fact, ask 249 for other treatments following failure of drug and intralesional therapy. Dorsal penile curvature with preservation of penile erection and optimal rigidity is treated by plaque incision/excision, grafting, and penile plication. Jean, Wessells and associates recently reported on partial penile disassembly and corporal resection in a PD patient with distal corporal narrowing with poor glans support [21]. On the other hand, severe erectile dysfunction due to dorsal penile deviation combined with distal ¯accidity of the penis in late stage of the disease may necessitate the insertion of a penile prosthesis. Surgery can only create a penis that is adequately straightened to the extent that any residual curvature does not impede sexual intercourse and erectile function can be preserved at preoperative levels. Three surgical procedures are commonly used in the treatment ofPD: 1. Penile plication (Nesbit's procedure) [45] 2. Plaque excision or incision with grafting (tunica vaginalis/saphenous vein/dermal grafts/cadaveric pericardium/dermabraded preputial patch) [4, 9, 13, 18, 28, 32] 3. Penile prosthesis implantation with or without corporoplasty [32] The ®rst two procedures should only be used in men who have no diculty in obtaining or maintaining erections, and these procedures should not be employed until it is reasonably certain that the PD is stable. Plication results in penile shortening, erectile dysfunction, and diminished sexual satisfaction. Penile prosthesis implantation is usually the procedure of choice when there is coexisting diculty obtaining or maintaining erections. Prosthesis should be inserted only after resolution of the acute painful, in¯ammatory stage, which may take approximately 6 months. Penile plication [24, 45] Penile plication may be a reasonable option when there is penile curvature without signi®cant narrowing or poor distal rigidity. On the convex surface opposite the point of maximal curvature, 1-cm longitudinal incisions are made on the normal tunica. The incisions are then closed transversely with running 3±0 PDS suture. Excellent results with this procedure have been reported in 89% of the patients and good results in 7%. Plaque excision and grafting [4, 9, 13, 18, 28, 33, 46] Large, thick, or calci®ed plaques are best excised. Access to the plaque can be obtained through a degloving incision with circumcision or through a dorsal or ventral longitudinal penile incision. Access to a dorsal plaque requires re¯ection and preservation of the neurovascular bundle, whereas access to a ventral plaque requires elevation of the corpus spongiosum and urethra. The defect in the tunica albuginea following plaque excision is ®lled with a graft. Tissue used for grafting includes: tunica vaginalis, temporalis fascia, saphenous vein, lyophilized dura, dorsal penile skin and penile dermal ¯ap. Synthetic graft materials (Dacron or GoreTex) have also been used but are not recommended because of their inelasticity. Plaque incision and saphenous vein graft has recently been reported to yield good results (penile straightening in 80% of the patients) during a follow-up period of 32 months. Penile prosthesis implantation with or without corporoplasty [32] When men have both penile deformity and diculty in obtaining or maintaining erections (due to vasculogenic erectile dysfunction), penile prosthesis implantation is preferred. Both semirigid and in¯atable (2-piece/3-piece) penile prostheses are available. Semirigid prosthesis, is however, often much more dicult to insert in patients with corporal ®brosis. In most patients with PD an in¯atable prosthesis is utilized. Conclusions Peyronie's disease is an acquired condition probably resulting from injury with a variable and sometimes selflimiting natural history. Patient and partner counseling can be very helpful. Penile pain during erection is the most common symptom in the early stage of the disease, which can be treated by various agents. In patients who develop a sexual disability because of signi®cant erectile deformity, surgical treatment is indicated. No one surgical procedure is applicable to all patients with PD, and the procedure should be selected based on the patient's ®ndings and wishes. References 1. Amin Z, Patel U, Friedman EP, et al (1993) Color Doppler and duplex ultrasound assessment of Peyronie's disease in impotent men. Br J Radiol 66: 398±402 2. Bivalacqua TJ, Diner EK, Novak TE, et al (2000) A rat model of Peyronie's disease associated with a decrease in erectile activity and an increase in inducible nitric oxide synthase protein expression. Program and abstracts from the American Urological Association 95th Annual Meeting; April 29±May 4, Atlanta, Georgia. Abstract 745 3. Bour H (1984) Current status of vitamin E. Rev Prat 34: 1270±1271 4. Brannigan RE, Kim ED, Oyasu R, et al (1998) Comparison of tunica albuginea substitutes for the treatment of Peyronie's disease. J Urol 159: 1064±1068 5. Chesney J (1975) Peyronie's disease. Br J Urol 47: 209±218 6. Carson CC (1997) Potassium para-aminobenzoate for the treatment of Peyronie's disease: is it eective? Tech Urol 3: 135±139 250 7. Chiang PH, Chiang CP, Shen MR, et al (1992) Study of the changes in collagen of the tunica albuginea in venogenic impotence and Peyronie's disease. Eur Urol 21: 48±51 8. El-Sakka AI, Lue TF (1998) Peyronie's disease. Curr Opin Urol 8: 203±209 9. El-Sakka AI, Rashwan HM, Lue TF (1998) Venous patch graft for Peyronie's disease. Part II: Outcome analysis. J Urol 160: 2050±2053 10. Elterman L, Bewsey K, Cs-Szabo G, et al (2000) Connective tissue components of Peyronie's disease plaque. Program and abstracts from the American Urological Association 95th Annual Meeting; April 29±May 4, Atlanta, Georgia. Abstract 748 11. Fitkin J, Ho GT (1999) Peyronie's disease: current management. Am Fam Physician 60: 549±552) 12. Furlow WL, Swanson HE, Lee RE (1975) Peyronie's disease: A study of its natural history and treatment with orthovoltage radiotherapy. J Urol 114: 69±71 13. Gelbard MK, Hayden B (1991) Expanding contractures of the tunica albuginea due to Peyronie's disease with temporalis fascia free grafts. J Urol 145: 772 14. Gelbard MK, Dorey F, James K (1990) The natural history of Peyronie's disease. J Urol 144: 1376±1379 15. Hauck W, Warten U, Hackstein H, et al (2000) HLA-system screening in Peyronie's disease. Program and abstracts from the American Urological Association 95th Annual Meeting; April 29±May 4, Atlanta, Georgia. Abstract 744 16. Hauck EW, Altinkilic BM, Ludwig M, et al (2000) Extracorporal shock wave therapy in the treatment of Peyronie's disease. Eur Urol 38: 663±670 17. Hellstrom WJ, Bivalacqua TJ (2000) Peyronie's disease: etiology, medical, and surgical therapy. J Androl 21: 347±354 18. Henry GD, Coming TJ, Makuli, MJ, et al (2000) Histochemical analysis of vein grafting of the tunica albuginea in comparison to tunica vaginalis. Program and abstracts from the American Urological Association 95th Annual Meeting; April 29 ± May 4, Atlanta, Georgia. Abstract 749 19. Husain J, Lynn NNK, Jones DK (2000) Extracorporeal shock wave therapy in the management of Peyronie's disease: initial experience. BJU Int 86: 466±468 20. Jarow JP, Lowe FC (1997) Penile trauma: an etiologic factor in Peyronie's disease and erectile dysfunction. J Urol 157: 1388± 1390 21. Jean VO, Wessells H, Jordan JH, et al (2000) Partial penile disassembly and corporeal resection Peyronie's disease with distal narrowing. J Urol 164: 449±450 22. Kadioglu A, Tefekli A, Erol H, et al (2000) Color Doppler ultrasound assessment of penile vascular system in men with Peyronie's disease. Int J Impotence Res 12(): 263±268 23. Levine LA, Goldman KE (2000) Updated experience with intralesional verapamil injection treatment for Peyronie's disease. Program and abstracts from the American Urological Association 95th Annual Meeting; April 29 ± May 4, Atlanta, Georgia. Abstract 751 24. Levine LA, Lenting EL (1997) A surgical algorithm for the treatment of Peyronie's disease. J Urol 158: 2149±2152 25. Lopez JA, Jarrow JP (1993) Penile vascular evaluation of men with Peyronie's disease. J Urol 149: 53±55 26. Ludwig G (1991) Evaluation of conservative therapeutic approaches to Peyronie's disease (®brotic induration of the penis). Urol Int 47: 236±239 27. Lue TF (1998) 1998 AUA Annual Meeting (San Diego '98) PG course, ``Erectile dysfunction, priapism and Peyronie's disease'': Functional anatomy of the penis. AUA Oce of Education, Course No 009821 PG; Sunday, May 31, 1998 28. Lue TF, El-Sakka AI (1998) Venous patch graft for Peyronie's disease. Part I: technique. J Urol 160: 2047±2049 29. Matkov G, Levine LA, Storm DW (2000) Peyronie's disease aecting the younger male. Program and abstracts from the American Urological Association 95th Annual Meeting; April 29 ± May 4, Atlanta, Georgia. Abstract 743 30. Michel MS, Braun P, Sazova O, et al (1999) Shock wave therapy for the treatment of Peyronie's disease: ®rst clinical study for the objective determination of deviation improvement by means of arti®cial erection. J Urol 161: 262 31. Mirone V, Imbimbo C, Palmieri A, et al (1999) Our experience on the association of a new physical and medical therapy in patients suering from induratio penis plastica. Eur Urol 36: 327±330 32. Montague DK, Angermeier KW, Lakin MM, et al (1996) AMS 3-piece in¯atable penile implantation in men with Peyronie's disease: comparison of CX and Ultrex cylinders. J Urol 156: 1633±1635 33. Montorsi F, Salonia A, Maga T, et al (2000) Evidence based assessment of long-term results of plaque incision and vein grafting for Peyronie's disease. J Urol 163: 1704±1708 34. Mulhall JP, Lubrano T, Thom J, et al (2000) Cytogenetic evidence in support of Peyronie's disease being a tunical ®eld defect process. Program and abstracts from the American Urological Association 95th Annual Meeting; April 29 ± May 4, Atlanta, Georgia. Abstract 747 35. Muralidhar S, Gulati M, Kumar B, et al (1996) An ultrasonographic study of Peyronie's disease. Australas Radiol 40: 106±108 36. Poutasse EF (1972) Peyronie's disease. J Urol 107: 419±422 37. Ralph DJ (1999) What's new in Peyronie's disease? Curr Opin Urol 9(): 569±571 38. Ralph DJ, Hughes T, Lees WR, et al (1992) Pre-operative assessment of Peyronie's disease using colour Doppler sonography. Br J Urol 69: 629±632 39. Riedl CR, Plas E, Engelhardt P, et al (2000) Iontophoresis for treatment of Peyronie's disease. J Urol 163: 95 40. Roberts HJ (1995) Vitamin E. Lancet 345: 737 41. Schwarzer U, Klotz T, Braun M, et al (2000) Prevalence of Peyronie's disease: results of an 8,000 men survey. Program and abstracts from the American Urological Association 95th Annual Meeting; April 29 ± May 4, Atlanta, Georgia. Abstract 742 42. Somers KD, Sismour EN, Wright GL, et al (1989) Isolation and characterization of collagen in Peyronie's disease. J Urol 141: 629±631 43. Stojic M, Negrojevic M, Josic P, et al (1987) Conservative therapy of Peyronie's disease using vitamin E. Med Pregl 40: 133±135 44. Teloken C, Rhoden EL, Grazziotin TM, et al (1999) Tamoxifen versus placebo in the treatment of Peyronie's disease. J Urol 162: 2003±2005 45. van der Drift DGF, Vroege JA, Groenendijik PM, et al (2000) The plication procedure for penile curvature: surgical outcome and post-operative sexual function. Program and abstracts from the American Urological Association 95th Annual Meeting; April 29 ± May 4, Atlanta, Georgia. Abstract 753 46. Wayne JG, Hellstrom WJ, Reddy S (2000) Application of pericardial graft in the surgical management of Peyronie's disease. J Urol 163: 1445±1447 47. Weidner W, Schroeder-Printzen I, Weiske WH (1997) Sexual dysfunction in Peyronie's disease: an analysis of 222 patients without previous local plaque therapy. J Urol 157: 325±328 48. Weidner W, Schroeder-Printzen I, Rudnick J, et al (1999) Randomized prospective placebo-controlled therapy of Peyronie's disease (IPP) with Potaba (aminobenzoate potassium). J Urol 161[Suppl]: 205