* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Blood Vessels PowerPoint
Blood sugar level wikipedia , lookup
Hemolytic-uremic syndrome wikipedia , lookup
Blood transfusion wikipedia , lookup
Schmerber v. California wikipedia , lookup
Autotransfusion wikipedia , lookup
Blood donation wikipedia , lookup
Plateletpheresis wikipedia , lookup
Jehovah's Witnesses and blood transfusions wikipedia , lookup
Men who have sex with men blood donor controversy wikipedia , lookup
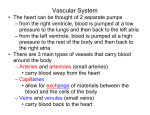
The Cardiovascular System blood vessels Blood Circulation Blood is carried in a closed system of vessels that begins and ends at the heart Human Cardiovascular System The 3 major types of vessels Arteries – carry blood away from the heart Veins – carry blood toward the heart Capillaries – contact tissue cells (Serving cellular needs) Capillaries · Very narrow (10 µm diameter, the red blood cells that travel through capillaries are 6 µm in diameter). Capillaries are made of thin endothelial cells (one layer thick) Capillary Blood Flow • Blood flow across the capillary bed is regulated by a sphincter muscle on the arteriole side. Whenever there is little need to supply blood to a given capillary bed, the sphincter closes and blood bypasses the capillary bed via an arteriovenal shunt. • On the arterial side of the capillaries, blood is under high pressure, whereas the blood at the venal side is under low pressure. Hydrostatic & Osmotic Pressures • The high hydrostatic pressure on the arterial side squeezes water and nutrients out of the capillaries. • Water leaving the capillaries builds up the osmotic pressure because the blood components have become more concentrated. • Towards the venal end, water and waste materials are sucked into capillaries by the osmotic pressure. Capillary Dynamics Capillary Exchange Gases, nutrients, and wastes are exchanged between blood in the capillaries of tissues in 3 ways: • 1. Diffusion • a. most common • b. substances including O2, CO2, glucose, & hormones • c. lipid-soluble substances pass directly through endothelial cell membrane; • d. water-soluble substances must pass through fenestrations or gaps between endothelial cells. • 2. Vesicular transport (endo/exocytosis); • 3. Bulk flow (filtration and absorption). Arteries & arterioles • (High pressure & Low resistance) The blood vessels before the capillary beds have to bear high hydrostatic pressures created by the heart Arteries and smaller arterioles are thick walled tubes made of smooth muscle (to resist high pressure), containing a layer of collagen fibers (to give elasticity), and lined with endothelial cells (to protect red blood cells from mechanical damage). Tunica’s Tunica’s Veins & venules (Low Pressure & Low Resistance) • Contain valves to prevent the backflow of blood • Varicose veins result due to a failure of these valves Venous Blood Flow HEMODYNAMICS: THE PHYSIOLOGY OF CIRCULATION Blood pressure = pressure exerted by blood on the wall of blood vessels. • In clinical use, we most commonly refer to mean (systemic) arterial blood pressure (MABP), because the blood pressure in the veins is essentially insignificant. • The mean arterial blood pressure (MABP) rises to its maximum during systole (contraction) and falls to its lowest during diastole (relaxation). • In a normal adult at rest, the MABP = 120 mmHg/80 mmHg Factors that Influence Arterial Blood Pressure • Heart Action (cardiac output) • Blood Volume (increase in blood volume increases BP) • Peripheral Resistance (resistance; R = opposition to blood flow usually due to friction) • So we can say CO = MABP/R Blood Flow Friction This friction depends on 3 things: • 1. Blood viscosity • 2. Total blood vessel length • 3. Blood Vessel Radius Regulation of BP “Blood Flow” • F = ΔP/ R • ΔP= change in pressure between arterial & venous ends • R= Peripheral Resistance Hormonal Control Several hormones affect BP by: • acting on the heart • altering blood vessel diameter • adjusting blood volume. Hormones that increase BP Epinephrine and norepinephrine Increases CO (rate & force of contraction) & causes vasoconstriction of arterioles. Antidiuretic hormone (ADH) Causes vasoconstriction of arterioles during diuresis and during hemorrhage. Angiotensin II Causes vasoconstriction of arterioles and causes the secretion of aldosterone Aldosterone Increases Na+ and water reabsorption in the kidneys. Hormones that decrease BP Atrial natriuretic peptide (ANP) Causes vasodilation of arterioles and promotes the loss of salt and water in urine. Histamine Causes vasodilation of arterioles (plays a key role in inflammation) Regulation of Blood Pressure and Blood Flow: • Neural Regulation: • The cardiovascular (CV) center is located in the medulla oblongata • CV Center Input: • Nerve impulses are sent to the CV center from three areas: • 1. Higher brain centers • 2. Baroreceptors (or pressoreceptors) which • detect changes in BP in aorta and carotid arteries • 3. Chemoreceptors that detect changes in key blood chemical concentrations (H+, CO2, and O2) • Regulation of Blood Pressure and Blood Flow: • Neural Regulation: • CV Center Output: • Nerve impulses are sent from the CV center to either: • 1. The Sinoatrial (SA) Node of heart • 2. The smooth muscle of peripheral blood vessels (i.e. arterioles). • Regulation of Blood Pressure and Blood Flow: • Negative-Feedback Regulation: • If BP is too high: • 1. Increase is detected by baroreceptors in the carotid artery or aorta • 2. Baroreceptors send an impulse to CV center • 3. CV center interprets that message and sends a signal to the SA Node and arterioles • 4. The SA Node decreases heart rate • 5. The arterioles dilate • If BP is too low... • 1. SA Node increases hr; • 2. Constriction of arterioles