* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 1. circumstances when shared care is appropriate
Survey
Document related concepts
Transcript
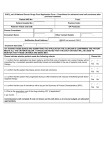
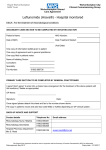
Leflunomide for active Rheumatoid Arthritis and Psoriatic Arthritis in Adults Shared Care Guideline: Prescribing Agreement Section A: To be completed by the hospital consultant initiating the treatment GP Practice Details: Name: Address: Tel no: Fax no: NHS.net e-mail: Consultant name: Clinic name: Contact details: Address: Tel no NHS.net e-mail: Diagnosis: Patient Details: Name: Address: DOB: / / Hospital number: NHS number (10 digits): Fax no: Drug name & dose to be prescribed by GP: Next hospital appointment: / / . Dear Dr. , Your patient was seen on / / and I have started Leflunomide mg (insert dose) for the above diagnosis. I am requesting your agreement to sharing the care of this patient from / / in accordance with the (attached) Shared Care Prescribing Guideline (approval date: / / ). Please take particular note of Section 2 where the areas of responsibilities for the consultant, GP and patient for this shared care arrangement are detailed. Patient information has been given outlining potential aims and side effects of this treatment and * supplied (* insert any support materials issued such as patient held monitoring book etc where applicable) . The patient has given me consent to treatment possibly under a shared care prescribing agreement (with your agreement) and has agreed to comply with instructions and follow up requirements. . The following investigations have been performed on / / and are acceptable for shared care. Please monitor FBC including total and differential WCC and platelets and LFTs every weeks. Test Result Test Result Test Result BP: mmHg LFTs: FBC: Body weight: AST Haemoglobin kg ALT WBC U&E’s: Sodium (Na) GGT Neutrophils Potassium (K) Bilirubin Platelets Urea (U) Alk phosp Creatinine (Cr) Other relevant information: Consultant Signature: ………………………………………Date: / / Section B: To be completed by the GP and returned to the hospital consultant as detailed in Section A above Please sign and return your agreement to shared care within 14 days of receiving this request Tick which applies: I accept sharing care as per shared care prescribing guideline and above instructions I would like further information. Please contact me on: I am not willing to undertake shared care for this patient for the following reason: GP name: GP signature: ………………………………………………Date: / / 1 This Page in Intentionally Blank 2 working in partnership SHARED CARE PRESCRIBING GUIDELINE LEFLUNOMIDE for Active Rheumatoid Arthritis and Psoriatic Arthritis in Adults NOTES to the GP The expectation is that these guidelines should provide sufficient information to enable GPs to be confident to take clinical and legal responsibility for prescribing this drug. The questions below will help you confirm this: Is the patient’s condition predictable or stable? Do you have the relevant knowledge, skills and access to equipment to allow you to monitor treatment as indicated in this shared care prescribing guideline? Have you been provided with relevant clinical details including monitoring data? If you can answer YES to all these questions (after reading this shared care guideline), then it is appropriate for you to accept prescribing responsibility. If the answer is NO to any of these questions, you should not accept prescribing responsibility. You should write to the consultant within 14 days, outlining your reasons for NOT prescribing. If you do not have the confidence to prescribe, we suggest you discuss this with your local Trust/specialist service, who will be willing to provide training and support. If you still lack the confidence to accept clinical responsibility, you still have the right to decline. Your CCG pharmacist will assist you in making decisions about shared care. It would not normally be expected that a GP would decline to share prescribing on the basis of cost. The patient’s best interests are always paramount Date Prepared: January 2014 Review date: January 2017 Approved by: SWL Medicines Commissioning Group, Jan 2014 This shared care prescribing guideline has been signed off by the following individuals on behalf of their respective organisations: Participating CCGs Participating Hospital Trusts Croydon CCG Croydon University Hospitals Janice Steele, Deputy Chief Pharmacist Louise Coughlan, Chief Pharmacist on behalf of on behalf of Croydon Prescribing Committee Croydon Prescribing Committee Kingston CCG Epsom and St. Helier University Hospitals Seema Buckley, Chief Pharmacist Anne Davies, Chief Pharmacist Dr Jonathan Edwards, Medicines Management GP Dr Sanjeev Patel, DTC Chair Merton CCG St. George’s Healthcare Sedina Agama, Acting Chief Pharmacist Chris Evans, Chief Pharmacist Dr Vasa Gnanapragam, GP Emma Baker, Professor of Clinical Pharmacology Richmond CCG Kingston Hospital Emma Richmond, Chief Pharmacist Derek Cock, Chief Pharmacist Harriet Bradley, Medical Director Sutton CCG Sarah Taylor, Acting Chief Pharmacist Dr Simon Elliott, Dr Roshni Scott, Prescribing Lead GPs Wandsworth CCG Nick Bevan, Chief Pharmacist Dr Rod Ewen, Chair CEMMaG Date prepared: Date approved: Review date: January 2014 January 2014 January 2017 3 SHARED CARE PRESCRIBING GUIDELINE Leflunomide 1. CIRCUMSTANCES WHEN SHARED CARE IS APPROPRIATE Prescribing responsibility will only be transferred when the consultant and the GP are in agreement that the patient’s condition is stable or predictable. Patients will only be referred to the GP once the GP has agreed in each individual case and the hospital will continue to provide prescriptions until successful transfer of responsibilities as outlined below. The hospital specialist will supervise treatment with leflunomide including prescribing for 6 months and if stable shared care will be requested. 2. AREAS OF RESPONSIBILITY Consultant: Pre-treatment checks: Assess patient suitability for treatment with leflunomide including risk/benefit, drug interactions, contraindications, co-morbidities. Conduct baseline monitoring of FBC, LFTs including ALT, U&Es, blood pressure and body weight. Exclude pregnancy in women of childbearing potential prior to initiation of leflunomide. Patient education: Discuss benefits vs risks with patient. Educate patient about all aspects of treatment including potential adverse effects and monitoring requirements. Provide Arthritis Research Campaign (ARC) patient information sheet on Leflunomide. Issue / explain shared care monitoring card. Starting treatment: Prescribe leflunomide for at least 6 months. Monitor tolerance and follow up to ensure efficacy during first 6 months of treatment. Continuation of treatment: Liaise with GP suggesting that shared care is agreed for the patient after 6 months. The hospital will provide prescriptions until shared care has been agreed. Review patient at agreed intervals. Monitor efficacy and update GP of patient’s progress after each clinic visit Provide advice on dose adjustment if necessary and liaise with GP if repeat prescribing should stop. Evaluate and follow up adverse effects reported by patient or GP. Monitor for drug interactions. Identify non-compliance with drug safety monitoring. GP: Notify the consultant in writing whether or not the GP is agreeable to share care within 14 days (using “Shared Care Guideline: Prescribing Agreement” if available). Continue prescribing maintenance dose of leflunomide as recommended by consultant rheumatologist. Monitor patient’s overall health status and well-being. Monitor FBC, LFTs and blood pressure every 4 or 8 weeks as directed by Consultant and monitoring requirements listed on, page 8. Report any adverse reactions to the consultant rheumatologist. Discuss with rheumatologist before initiating washout procedure and/or reducing or stopping leflunomide. Monitor for drug interactions, see page 8. Monitor for compliance with drug safety monitoring. Report non-compliance to consultant rheumatologist. Liaise with consultant rheumatologist if signs/symptoms of disease progression occur. If pregnancy occurs discuss urgently with supervising rheumatologist and refer back to hospital. GP may initiate washout to avoid delay. If patient wishes to become pregnant, refer back to hospital (shared care is no longer appropriate in such cases). Patient: Comply with drug safety monitoring schedule. Report adverse effects and inform GP/Consultant if wishing to become pregnant (if applicable). Show shared care monitoring card to healthcare professionals. Limit alcohol intake well within national limits (4-8 units per week). Date prepared: Date approved: Review date: January 2014 January 2014 January 2017 4 SHARED CARE PRESCRIBING GUIDELINE 3. COMMUNICATION AND SUPPORT Hospital contacts: Out of hours contacts & procedures: (the referral letter will indicate named consultant) St Helier Hospital Dr Oliver Duke Dr Sanjeev Patel CNS Rheumatology Josephine Walmsley CNS Rheumatology Preeja Kugathasan Fax: 020 8296 3643 Epsom General Hospital Dr Helen Linklater / Dr. Pamela Leventis CNS Rheumatology Preeja Kugathasan Tel: 01372 735120; Fax: 01372 735141 St George’s Hospital Dr Patrick Kiely (PK) Dr Virinderjit Sandhu (VS) Dr Katie Moss (KM) Dr Nidhi Sofat Dr A. Kaul Duty Rheumatology SpR Nurse Specialists Margaret Sibley 020 8666 6812 Francesca Leone 020 8666 6807 Dida Cankov 020 8666 6801 Croydon University Hospital Tel: 020 401 3000 Dr Natalie Horwood:: Ext 3010 Dr Rosh Sathanathan: Ext 3010 Dr Sarah Levy: Ext 3010 Ruth Britten CNS Rheumatology: Ext 3010 Medicines Information: Ext 3059 020 8296 2473 020 8296 2473 020 8296 2473 020 8296 2473 On-Call Medical SpR via St Helier Hospital switchboard 020 8296 2000 On-Call Medical SpR via Epsom Hospital switchboard 01372 735 735 020 8725 2109 020 8725 1418 020 8725 1419 020 8725 1419 020 8725 3596 020 8672 1255 Duty Medical SpR via St George’s Hospital switchboard 020 8672 1255 Medical Registrar on call via switchboard 020 8401 3000 On-Call Medical SpR via Kingston Hospital Switchboard Tel: 0208 546 7711 Kingston Hospital Dr Shahid Jawed Tel:0208 934 2089 Dr Hugh Jones Fax No. 0208 934 3287 Dr Jane Foley – Queen Mary’s Hospital Tel 0208 487 6897 or 6898 Fax No. 0208 487 6916 CNS Rheumatology Kate Hunt 0208 934 2089 (or at Queen Mary’s on Tel 0208 487 6898) Specialist support/resources available to GP including patient information: See www.arc.org.uk For patient information on leflunomide see: http://www.arthritisresearchuk.org/arthritis_information/arthritis_drugs__medication/leflunomide.aspx 4. CLINICAL INFORMATION Indication(s): Treatment of adult patients with active rheumatoid arthritis or psoriatic arthritis either alone or in combination with methotrexate. Place in Therapy: For treatment of active rheumatoid arthritis or psoriatic arthritis. Therapeutic summary: Leflunomide is an isoxazole derivative. The active metabolite inhibits the enzyme dihydroorotate dehydrogenase. This results in inhibition of pyrimidine synthesis and arrests activated autoimmune lymphocytes which decreases the autoimmune response. Date prepared: Date approved: Review date: January 2014 January 2014 January 2017 5 SHARED CARE PRESCRIBING GUIDELINE Dose & route of administration: Duration of treatment: Summary of adverse effects: RA - Maintenance dose: 10 – 20mg once a day (if used as monotherapy) 10mg once a day if used in combination with another DMARD like methotrexate. Psoriatic arthritis – Maintenance dose: 20mg once a day. Long term provided treatment effective and without adverse effect. (See summary of product characteristics (SPC) for full list) Adverse effect Frequency Hypertension Mild -common Severe- rare Respiratory, thoracic and mediastinal disorders- Interstitial lung disease (including interstitial pneumonitis), which may be fatal) GI disorders - Diarrhoea, nausea, vomiting, abdominal pain Rare Common - Oral mucosal disorders -Aphthous stomatitis, mouth ulceration Common - Taste disturbances - Pancreatitis Nervous system disorders - Headache Uncommon Very rare - Paraesthesia, dizziness - Peripheral neuropathy Skin reactions/hair loss - Increased hair loss Common Very rare - Eczema, dry skin - Rash (incl maculopapular rash), pruritus Common Common - Urticaria - Severe anaphylactic, anaphylactoid reactions, vasculitis (incl cutaneous necrotizing vasculitis) - Stevens-Johnson syndrome, toxic epidermal necrolysis, erythema multiforme Uncommon Very rare Date prepared: Date approved: Review date: January 2014 January 2014 January 2017 Common Common Very rare Very common: ≥ 1/10 Common:≥1/100, <1/10) Uncommon:≥1/1000, <1/100 Rare:≥1/10,000, <1/1000 Very rare: <1/10,000 Management by GPs If BP > 140/90 treat in line with NICE guidance. If BP remains uncontrolled discuss with consultant and consider referral back to consultant for dose adjustment / wash-out or change in treatment. Contact hospital urgently if cough plus dyspnoea presents. If increasing shortness of breath occurs stop leflunomide and refer back to hospital for washout Give symptomatic treatment (eg anti emetic, antidiarrhoeal) or refer back to hospital for dose reduction. If severe or persistent stop and consider wash-out. Discuss with consultant in all cases. Stop treatment until extent of reaction clear. If Stevens Johnson syndrome refer immediately to hospital. If reaction confined to mouth then symptomatic relief or dose reduction, with or without partial wash-out. Discuss with consultant. Refer to hospital. If headache is severe refer back to hospital to consider dose reduction and if headaches persist stop and consider washout. Discuss with supervising consultant. Discuss with consultant. Alopecia is reversible with dose reduction or discontinuation. Contact consultant for advice with a view to consider dosage reduction. If severe refer back to consultant to consider stopping treatment and washout. Treat symptomatically. If mild continue leflunomide and monitor. If moderate or severe discuss with consultant with a view to consider symptomatic treatment (eg anti histamine) or dose reduction, with or without partial wash-out. Discuss with supervising consultant. Requires immediate assessment in hospital. As soon as skin and/or mucosal reactions observed which raise suspicion of such severe reactions, discontinue leflunomide, contact consultant immediately and refer back to hospital for washout. 6 SHARED CARE PRESCRIBING GUIDELINE Summary of adverse effects cont’d: (See summary of product characteristics (SPC) for full list) Adverse effect Liver reactions - Raised liver parameters Transaminases (mainly ALT) Gamma-GT, alkaline phosphatase, bilirubin - Hepatitis, jaundice/cholestasis - Hepatic failure, acute hepatic necrosis (may be fatal) Frequency Infections Severe - rare Haematological reactions (manifested as abnormal bruising or severe sore throat) - Anaemia Uncommon - Leucopenia(leucocytes>2G/l) - Leucopenia(leucocytes<2G/L) - Mild thrombocytopenia (platelets <100G/l) - Pancytopenia, eosinophilia - Agranulocytosis, vasculitis Common Less often Rare Very rare Common Rare Uncommon Rare Very rare Management by GPs If < 2 fold rise in AST, ALT (from upper limit of normal reference range –ULN) Monitor LFTs every 2 weeks and expect values to normalise spontaneously. If between 2 and 3 times rise in AST, ALT (from upper limit normal reference range-ULN) Recheck LFTs within 72 hours. If still 2 to 3 times ULN, reduce dosage and recheck LFTs every 2 weeks. If still 2 to 3 times ULN then stop Leflunomide. If > 3 fold rise in AST, ALT (from upper limit of normal reference range –ULN) Recheck LFTs within 72 hours. If still > 3 times ULN, contact consultant, stop leflunomide and consider washout. In event of severe, uncontrolled infection refer to hospital. Susceptibility to infections increased, particularly opportunistic infections. Infections may be more severe and require early and vigorous treatment. Patients with tuberculin reactivity must be carefully monitored because of risk of tuberculosis reactivation. Check FBC immediately and withhold drug(s) until results known. Check haematinics and replace appropriately. Discuss with consultant. If WBC < 3.5 x109/l, neutrophils <2.0x109/l or platelets < 150x109/l stop leflunomide and any concomitant myelosuppressive medication and contact consultant immediately. Refer back to hospital. Monitor carefully. If >10% weight loss with no other cause identified discuss with consultant with a view to consider dose reduction. Refer back if stopping treatment/washout required. Neoplasms, benign, malignant and unspecified (including cysts and polyps) Increased risk of malignancy, particularly lymphoproliferative disorders is increased with use of some immunosuppressive agents. Metabolism and nutrient disorders: Common - CPK increased Uncommon Discuss with consultant. - Hypokalaemia, hyperlipidaemia, hypophosphataemia Rare - LDH increased Unknown - Hypouricemia Miscellaneous Uncommon Seek advice from consultant if needed. - Anxiety Common - Tenosynovitis Uncommon - Tendon rupture Not known - Renal failure Common - Asthenia Not known -Marginal (reversible) decreases in sperm concentration, total sperm count and rapid progressive motility. Weight loss (usually insignificant) / anorexia Date prepared: Date approved: Review date: January 2014 January 2014 January 2017 Common 7 SHARED CARE PRESCRIBING GUIDELINE Monitoring Requirements: Clinically relevant drug interactions: Practical issues: Key references: Original Author(s) Update Author(s) Date prepared: Date approved: Review date: January 2014 January 2014 January 2017 Monitoring conducted by the hospital: Pre-treatment assessment Baseline FBC, LFTs including ALT, U&Es, blood pressure and body weight. Pregnancy test prior to initiation of leflunomide if appropriate. Monitoring treatment† FBC including total and differential white cell count, LFTs every 4 weeks for first 6 months then every 8 weeks thereafter. The frequency should be increased to monthly where combination therapy with another immunosuppressant or hepatotoxic drug is used. Monitoring conducted by GP : FBC including total and differential white cell count, LFTs every 8 weeks or if used in combination with another immunosuppressant or hepatotoxic drug every 4 weeks. Monitor for side effects and act accordingly (see under side effects). Check blood pressure and weight at the time of blood testing. Increased risk of toxicity with other haematotoxic drugs. Increased risk of toxicity with other hepatotoxic drugs. Alcohol should be avoided due to the risk of additive hepatotoxic effects. Should ONLY be used /initiated in combination with other DMARDs under consultant supervision. Warfarin – metabolism may be inhibited by leflunomide with increased anticoagulant effect–check INR 7 days after initiation of leflunomide and 7 days after any dose change of warfarin. Ask patient to report any evidence of severe bruising which may indicate high INR. Phenytoin – metabolism may be inhibited with increased phenytoin levels. Take phenytoin levels 14 days after initiation of leflunomide. Tolbutamide – metabolism may be inhibited with enhanced hypoglycaemic effect. Increase blood glucose monitoring for a few days following introduction of leflunomide then revert to normal frequency of monitoring. Cholestyramine – effect of leflunomide significantly decreased. Avoid unless drug elimination required. Vaccines – avoid concomitant use of leflunomide with live vaccines. Full washout procedure – Cholestyramine 8g TDS or Activated charcoal 50g QDS for 11 days. Partial washout procedure – Cholestyramine 8g TDS for 1 – 3 days British Society of Rheumatology Guidelines. Rheumatology 2008 Summary of Product Characteristics, Arava®, www.emc.medicines.org.uk accessed 14/11/2013 (last updated 08/01/2013) †The guidance and monitoring requirements included in this document derived from the BSR guidelines may deviate from those included in the SPC Dr. Patrick Kiely, Consultant Rheumatologist, St. George’s Hospital Dr. Sanjeev Patel, Consultant Rheumatologist, Epsom and St. Helier Hospital Brigitte van der Zanden, Chief Pharmacist Sutton and Merton PCT Christopher Haigh, Commissioning Support Pharmacist, South London CSU 8