* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Introduction to the Urinary System - Linn
Survey
Document related concepts
Transcript
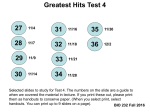
Tips for Success 1. 2. 3. 4. 5. 6. 7. Show up Participate in lab Show up Turn in assignments (completed, refer to #6) Show up Communicate with me, e-mail is best Show up Every point counts! Part 1 Urinary System Wastes Gases versus fluids Urinary system Dispose of water soluble wastes Fluid balance Electrolyte regulation Acid-base regulation Urinary System Other functions Kidneys Renin Erythropoietin Vitamin D activation Nitrogenous Wastes Urine is about 95% water Second largest component is urea Urea derived from breakdown of amino acids Nitrogenous Wastes 1. TOXIC! Dietary amino acids → NH2 removed → NH2 + H+ → NH3 500 ml of urine removes only 1 gram of nitrogen as ammonia 2. Ammonia can be converted to urea Requires energy 50 ml of urine removes 1 gram of nitrogen as urea 3. Ammonia can be converted to uric acid Requires lots of energy 10 ml of urine removes 1 gram of nitrogen as uric acid Fill in the blanks… Ammonia Toxicity Urea Very toxic Energy Costs High = 3 ATP Water Required 50 ml/g Nitrogen Solubility Examples Uric acid Low Fish & aquatic invertebrates Check your answers… Ammonia Urea Uric acid Toxicity Very toxic Moderate Non-toxic Energy Costs Negligible Moderate = 1.5 ATP High = 3 ATP 500 ml/g Nitrogen 50 ml/g Nitrogen 10 ml/g Nitrogen Solubility High Moderate Low Examples Fish & aquatic invertebrates Mammals, sharks & amphibians Birds, reptiles & snails Water Required Urinary System Organs Kidneys Major excretory organs Urinary bladder Temporary storage reservoir for urine Ureters Transport urine from the kidneys to the bladder Urethra Transports urine out of the body Hepatic veins (cut) Esophagus (cut) Inferior vena cava Adrenal gland Aorta Renal artery Renal hilum Renal vein Kidney Iliac crest Rectum (cut) Uterus (part of female reproductive system) Ureter Urinary bladder Urethra Figure 25.1 Anterior Inferior vena cava Peritoneum Peritoneal cavity (organs removed) Renal vein Renal artery Supportive tissue layers • Renal fascia anterior posterior • Perirenal fat capsule • Fibrous capsule Body of vertebra L2 Body wall (a) Aorta Posterior Figure 25.2a Kidneys Retroperitoneal position External anatomy Hilus 3 tissue layers surround & support Fibrous capsule Perirenal fat capsule Renal fascia Hydronephrosis Kidneys Internal Anatomy Renal cortex Superficial region Renal columns extend into medulla Kidneys Renal medulla Cone-shaped medullary (renal) pyramids separated by the renal columns Renal pelvis Funnel-shaped tube, contain calyces Continuous with ureter Kidneys Internal Anatomy Minor calyces Major calyces Branching channels of the renal pelvis Collect urine from minor calyces Empty urine into the pelvis Urine flows from the pelvis to ureter Renal hilum Renal cortex Renal medulla Major calyx Papilla of pyramid Renal pelvis Minor calyx Ureter Renal pyramid in renal medulla Renal column Fibrous capsule (a) Photograph of right kidney, frontal section (b) Diagrammatic view Figure 25.3 Kidneys Blood Supply Renal arteries deliver ~ 22 % of cardiac output (1.2 L/min) 90% directed to cortex Urine formation Cortical radiate vein Cortical radiate artery Arcuate vein Arcuate artery Interlobar vein Interlobar artery Segmental arteries Renal vein Renal artery Renal pelvis Ureter Renal medulla Renal cortex (a) Frontal section illustrating major blood vessels Figure 25.4a Aorta Renal artery Inferior vena cava Renal vein Segmental artery Interlobar vein Interlobar artery Arcuate vein Arcuate artery Cortical radiate vein Cortical radiate artery Peritubular capillaries and vasa recta Afferent arteriole Efferent arteriole Glomerulus (capillaries) Nephron-associated blood vessels (see Figure 25.7) (b) Path of blood flow through renal blood vessels Figure 25.4b Nephrons Structural and functional units that form urine ~1 million per kidney Two main parts 1. 2. Blood capillaries (glomeruli) Renal tubule: begins as cup-shaped glomerular (Bowman’s) capsule surrounding the glomerulus Figure 25.5 Nephrons Renal corpuscle Glomerulus + Bowman’s capsule Fenestrated glomerular endothelium Allows filtrate to pass from plasma into the glomerular capsule Glomerular capsule Glomerulus Efferent arteriole Afferent arteriole Parietal layer of glomerular capsule Capsular space Foot processes of podocytes Podocyte cell body (visceral layer) Red blood cell Proximal tubule cell Efferent arteriole Juxtaglomerular apparatus • Macula densa cells of the ascending limb of loop of Henle • Extraglomerular mesangial cells • Granular cells Afferent arteriole Juxtaglomerular apparatus Copyright © 2010 Pearson Education, Inc. Lumens of glomerular capillaries Endothelial cell of glomerular capillary Mesangial cells between capillaries Renal corpuscle Figure 25.8 Cortical nephron • Has short loop of Henle and glomerulus further from the corticomedullary junction • Efferent arteriole supplies peritubular capillaries Efferent arteriole Glomerular capillaries Renal corpuscle (glomerulus) Glomerular (Bowman’s) capsule Proximal convoluted tubule Peritubular capillaries Ascending or thick limb of the loop of Henle Arcuate vein Arcuate artery Cortex Loop of Henle Medulla Renal pelvis Descending Ureter or thin limb of loop of Henle Kidney Juxtamedullary nephron • Has long loop of Henle and glomerulus closer to the corticomedullary junction • Efferent arteriole supplies vasa recta Cortical radiate vein Cortical radiate artery Afferent arteriole Collecting duct Distal convoluted tubule Afferent arteriole Efferent arteriole Corticomedullary junction Vasa recta (a) Copyright © 2010 Pearson Education, Inc. Figure 25.7a Nephrons Renal tubules Proximal convoluted tubule (PCT) Functions Major site of reabsorption (amino acids, glucose, water, Na+) Secretion (medications, nitrogenous wastes) Exchange of ions important for pH (H+, HCO3-) Confined to the cortex Loop of Henle Descending and ascending limbs More later… Nephrons Renal tubules Distal convoluted tubule (DCT) Important site for secretion, aldosterone & ADH activity Exchange of ions important for pH (H+, HCO3-) Reabsorption of some electrolytes such as Na+ Confined to the cortex Nephrons Renal tubules Collecting tubules (CT) Receive filtrate from many nephrons Fuse together to deliver urine through papillae into minor calyces Functions Important site for secretion, aldosterone & ADH activity Site of reabsorption of water and electrolytes Exchange of ions important for pH (H+, HCO3-) Glomerular capsule: parietal layer Renal cortex Renal medulla Basement membrane Renal corpuscle • Glomerular capsule • Glomerulus Renal pelvis Ureter Podocyte Distal convoluted tubule Kidney Fenestrated endothelium of the glomerulus Glomerular capsule: visceral layer Microvilli Mitochondria Proximal convoluted tubule Highly infolded plasma membrane Proximal convoluted tubule cells Cortex Medulla Thick segment Thin segment Loop of Henle • Descending limb • Ascending limb Distal convoluted tubule cells Collecting duct Loop of Henle (thin-segment) cells Principal cell Intercalated cell Collecting duct cells Copyright © 2010 Pearson Education, Inc. Figure 25.5 Nephrons Juxtaglomerular Apparatus (JGA) Ascending limb of loop of Henle and afferent arteriole contact one another One per nephron Function Regulation of filtrate formation and blood pressure Glomerular capsule Glomerulus Efferent arteriole Afferent arteriole Parietal layer of glomerular capsule Capsular space Foot processes of podocytes Podocyte cell body (visceral layer) Red blood cell Proximal tubule cell Efferent arteriole Juxtaglomerular apparatus • Macula densa cells of the ascending limb of loop of Henle • Extraglomerular mesangial cells • Granular cells Afferent arteriole Juxtaglomerular apparatus Copyright © 2010 Pearson Education, Inc. Lumens of glomerular capillaries Endothelial cell of glomerular capillary Mesangial cells between capillaries Renal corpuscle Figure 25.8 Nephron Capillary Beds Glomerulus 1. Afferent arteriole glomerulus efferent arteriole Specialized for filtration Nephron Capillary Beds Peritubular capillaries 2. Low-pressure, porous capillaries adapted for absorption Arise from efferent arterioles Cling to adjacent renal tubules in cortex Empty into venules Cortical nephron • Has short loop of Henle and glomerulus further from the corticomedullary junction • Efferent arteriole supplies peritubular capillaries Efferent arteriole Glomerular capillaries Renal corpuscle (glomerulus) Glomerular (Bowman’s) capsule Proximal convoluted tubule Peritubular capillaries Ascending or thick limb of the loop of Henle Arcuate vein Arcuate artery Cortex Loop of Henle Medulla Renal pelvis Descending Ureter or thin limb of loop of Henle Kidney Juxtamedullary nephron • Has long loop of Henle and glomerulus closer to the corticomedullary junction • Efferent arteriole supplies vasa recta Cortical radiate vein Cortical radiate artery Afferent arteriole Collecting duct Distal convoluted tubule Afferent arteriole Efferent arteriole Corticomedullary junction Vasa recta (a) Copyright © 2010 Pearson Education, Inc. Figure 25.7a Nephrons Cortical nephrons 85% of nephrons; almost entirely in the cortex Juxtamedullary nephrons Long loops of Henle deeply invade the medulla Extensive thin segments Important in the production of concentrated urine Cortical nephron • Has short loop of Henle and glomerulus further from the corticomedullary junction • Efferent arteriole supplies peritubular capillaries Efferent arteriole Glomerular capillaries Renal corpuscle (glomerulus) Glomerular (Bowman’s) capsule Proximal convoluted tubule Peritubular capillaries Ascending or thick limb of the loop of Henle Arcuate vein Arcuate artery Cortex Loop of Henle Medulla Renal pelvis Descending Ureter or thin limb of loop of Henle Kidney Juxtamedullary nephron • Has long loop of Henle and glomerulus closer to the corticomedullary junction • Efferent arteriole supplies vasa recta Cortical radiate vein Cortical radiate artery Afferent arteriole Collecting duct Distal convoluted tubule Afferent arteriole Efferent arteriole Corticomedullary junction Vasa recta (a) Copyright © 2010 Pearson Education, Inc. Figure 25.7a Ureters Convey urine from kidneys to bladder Retroperitoneal location Enter base of bladder through posterior wall ↑ bladder pressure = distal ends of the ureters close Prevents backflow of urine Mucus is protective Urinary Bladder Muscular sac for temporary storage of urine On pelvic floor posterior to pubic symphysis Males—prostate gland surrounds the neck inferiorly Females—anterior to the vagina and uterus Urinary Bladder Stretch receptors in bladder create desire to void Micturition Urge to void usually occurs with about 300ml urine Can hold up to about 500ml Hepatic veins (cut) Esophagus (cut) Inferior vena cava Adrenal gland Aorta Renal artery Renal hilum Renal vein Kidney Iliac crest Rectum (cut) Uterus (part of female reproductive system) Ureter Urinary bladder Urethra Figure 25.1 Urethra Sphincters Internal CNS control External Voluntary control Peritoneum Ureter Rugae Detrusor muscle Ureteric orifices Bladder neck Internal urethral sphincter External urethral sphincter Urogenital diaphragm (b) Female. Copyright © 2010 Pearson Education, Inc. Trigone Urethra External urethral orifice Figure 25.21b Peritoneum Ureter Rugae Detrusor muscle Adventitia Ureteric orifices Trigone of bladder Bladder neck Internal urethral sphincter Prostate Prostatic urethra Urogenital diaphragm External urethral sphincter Membranous urethra Spongy urethra Erectile tissue of penis External urethral orifice (a) Male. The long male urethra has three regions: prostatic, membranous and spongy. Copyright © 2010 Pearson Education, Inc. Figure 25.21a Brain Higher brain centers Urinary bladder filling stretches bladder wall Allow or inhibit micturition as appropriate Pontine micturition center Afferent impulses from stretch receptors Simple spinal reflex Promotes micturition by acting on all three spinal efferents Pontine storage center Inhibits micturition by acting on all three spinal efferents Spinal cord Spinal cord Parasympathetic activity Sympathetic activity Detrusor muscle contracts; internal urethral sphincter opens Parasympathetic activity Sympathetic activity Somatic motor nerve activity External urethral sphincter opens Micturition Copyright © 2010 Pearson Education, Inc. Somatic motor nerve activity Inhibits Figure 25.22 Incontinence Damage to spinal cord Frequent micturition in infants Incontinence is normal: control of the voluntary urethral sphincter develops with the nervous system Pathway of Urine Flow Urine formed in nephrons calyces renal pelvis ureters bladder urethra