* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Multi-axis passive and active stiffnesses of the glenohumeral joint
Survey
Document related concepts
Transcript
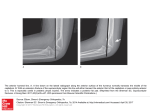
Clinical Biomechanics 19 (2004) 107–115 www.elsevier.com/locate/clinbiomech Multi-axis passive and active stiffnesses of the glenohumeral joint q Mohsen Makhsous, Fang Lin, Li-Qun Zhang * Department of Physical Medicine & Rehabilitation, Northwestern University, Chicago, IL, USA Department of Orthopaedic Surgery, Northwestern University, Chicago, IL, USA Department of Biomedical Engineering, Northwestern University, Evanston, IL, USA Rehabilitation Institute of Chicago, 345 E. Superior Street, Room 1406, Chicago, IL 60611, USA Received 25 September 2003; accepted 26 November 2003 Abstract Objective. To investigate passive and active glenohumeral stiffness in the anterior, posterior, superior, and inferior directions at different lateral positions of the humerus. Design. Glenohumeral stiffness along multiple axes was determined in fresh-frozen shoulder specimens under both passive (no simulated muscle contraction) and active (with simulated muscle contraction) conditions. Background. Glenohumeral laxity has been evaluated in various studies with focus on one of the multiple directions. However, glenohumeral stiffness characterizing the force–displacement relationship and stability has not been evaluated in all four directions under passive and active conditions. Methods. The humeral head was translated in the posterior, anterior, inferior and superior directions relative to the glenoid with different lateral positions, and multi-axis glenohumeral stiffness generated by passive and active structures were investigated. Results. Without muscle loading, glenohumeral stiffness in the superior direction (Ksup ¼ 5:83 N/mm) was higher than that in the inferior (Kinf ¼ 4:32), anterior (Kant ¼ 3:67), and posterior (Kpost ¼ 2:89) directions (P < 0:008), and Kinf was higher than Kpost (P ¼ 0:011). Stiffness in the different directions were correlated to each other (P < 0:001), and shifting the humerus laterally increased stiffness in all directions (P < 0:05) except for the superior direction. With moderate muscle loads, the glenohumeral joint became significantly stiffer in all four directions (P < 0:05) with less difference among different directions. Conclusions. Glenohumeral stiffnesses are different in the different directions but are correlated to each other and contribute jointly to glenohumeral stability. Muscle contractions can increase glenohumeral stiffness significantly. Relevance Multi-axis glenohumeral stiffness characterizes glenohumeral stability in 3D space and is related to glenohumeral functional movement that always involves multiple directions. The approach provides us a quantitative tool to evaluate shoulder biomechanical properties, and similar method can potentially be used in vivo on human subjects to assess shoulder injuries and treatment outcome. Ó 2003 Elsevier Ltd. All rights reserved. Keywords: Glenohumeral joint; Stiffness; Stability; Shoulder; In vitro 1. Introduction The glenohumeral (GH) joint is one of the most mobile joints of the human body with the humeral head supported partially by the relatively small concave gle- q Supplementary data associated with this article can be found, in the online version, at doi:10.1016/j.clinbiomech.2003.11.009 * Corresponding author. E-mail address: [email protected] (L.-Q. Zhang). 0268-0033/$ - see front matter Ó 2003 Elsevier Ltd. All rights reserved. doi:10.1016/j.clinbiomech.2003.11.009 noid. Passive structures, including the joint capsule, ligaments, labrum and articular surfaces, function together with muscles crossing the GH-joint to maintain stability of it (Soslowsky et al., 1997). One or more of the structures may be injured in various shoulder problems, resulting in altered GH stability and stiffness in the anterior, posterior, superior, and/or inferior directions (Soslowsky et al., 1997; Halder et al., 2001a; Blasier et al., 1997; Weiser et al., 1999; Ticker and Warner, 2000; Debski et al., 1999b; Warner et al., 1992; McQuade et al., 1999). 108 M. Makhsous et al. / Clinical Biomechanics 19 (2004) 107–115 GH-joint stability and laxity have been assessed by evaluating the resistance and/or range of motion during passive manual movement (Soslowsky et al., 1997; Halder et al., 2001a; Blasier et al., 1997; Weiser et al., 1999; Ticker and Warner, 2000; Debski et al., 1999b; Warner et al., 1992; McQuade et al., 1999). Since the measured joint laxity depends on the force applied, joint stiffness that characterizes the relationship between the force and displacement avoids such dependence and provides us an objective measure of the joint stability, independent of the load applied by an examiner. Clinically, GH stiffness may be changed considerably in shoulder injuries. On the one hand, the GH-joint may become too compliant with much reduced joint stiffness in unstable shoulders. On the other hand, a joint may become too stiff with severely reduced the range of motion in cases like frozen shoulders. GH instabilities occur in various directions of the GH-joint. A number of studies have been conducted to determine how different capsuloligamentous structures and muscles contribute to GH laxity, with each study generally focused on only one or two specific anatomical directions, such as the inferior (Soslowsky et al., 1997; Halder et al., 2001a), posterior (Blasier et al., 1997), anterior (Weiser et al., 1999; Ticker and Warner, 2000), posterior–anterior (Debski et al., 1999b; McQuade et al., 1999), inferior–superior (Warner et al., 1992) or anterior–inferior directions (Ticker and Warner, 2000; Malicky et al., 2001). It is not clear how different structures contribute to GH stability in the various anatomical directions (anterior, posterior, inferior and superior) in the same specimens, although GH stability along the multiple axes are related to each other and shoulder functions always involve multi-axis GH movement. There is also a lack of information on the dependence of GH stability on the humeral lateral position relative to the glenoid. Therefore, characterizing GH-joint stiffness along the multiple anatomical directions, and at different lateral humeral positions in the same specimens is useful to understand and evaluate GH-joint stability and functional performance in 3D space. The purpose of this study was to investigate contributions of capsuloligaments and muscle-tendon complexes crossing the GH-joint to GH stiffness along four anatomical axes of the glenoid (rather than only along a single direction). The hypotheses were: (1) GH capsuloligaments stiffness in the superior (Ksup ), inferior (Kinf ), anterior (Kant ), and posterior (Kpost ) directions are different from each other in amplitude but are correlated to each other; (2) lateral shift of the humerus increases GH stiffness in all four directions; (3) moderate loading of muscles crossing the GH-joint increases the joint stiffness significantly in all four directions. Study of passive and active control of GH-joint will help us better understand biomechanics of the GH-joint in 3D space, which may help us evaluate shoulder injuries, surgical outcome, and rehabilitation progress more accurately. Quantitative measure of GH stiffness along multiple axes may also help us improve existing computer shoulder models by providing characterization of GH stiffness/stability associated with GH translations that have been neglected in existing models and the joint is assumed to have only three rotational degrees of freedoms (a ball-socket joint). 2. Methods Specimen: Six fresh-frozen shoulder specimens (three left and three right specimens) from five cadavers with no sign of injury were used in the study. The donors were on average 56.83 (SD 3.43) years old at death and all of them were male. After peeling off the skin and subcutaneous tissues, the anterior, medial, and posterior portions of the deltoid, supraspinatus, teres minor, long head of biceps, upper, middle, and lower portions of the subscapularis and infraspinatus were dissected and separated from each other. A cable was sutured to each of the individual muscles through fiberglass mesh wrapped around the proximal end of the muscles except for the long head of biceps, which was loaded at the distal end. Each portion of the muscles was loaded along its line of action through a pulley system. The posterolateral corner and inferior part of the anterolateral of the acromion was chopped off to eliminate acromiohumeral impingement during the passive movement. Furthermore, potential impingement was checked by visual inspection and by monitoring possible sharp rise of the restraining force during the passive movement. Experimental setup: The specimen was mounted on a custom designed testing device, which allowed three rotations (abduction–adduction, flexion–extension, and internal–external rotation) and three translations (posterior–anterior, inferior–superior, and medial–lateral) of the humerus relative to the glenoid (Fig. 1). The scapula was bolted rigidly onto a Teflon plate with the glenoid surface oriented vertically. The humerus was fixed into an aluminum tubing by sharpened screws and the shaft of humerus was aligned with the centerline of the tubing. The arm was positioned at 60° GH abduction in the scapular plane. The aluminum tubing was attached to a beam parallel to the humeral shaft (Fig. 1). The beam was in turn mounted to an X –Y table controlled by two micrometers, which allowed adjustment of the humerus relative to the glenoid in the posterior–anterior and proximal–distal directions. The X –Y table was fixed to the bench through a six-axis force sensor (JR3 Inc., Woodland, CA, USA), which was aligned with the axes of the humerus coordinate system (Fig. 1). The scapula could be translated in the medial–lateral and inferior– superior directions by another X –Y table. The dis- M. Makhsous et al. / Clinical Biomechanics 19 (2004) 107–115 Fig. 1. Experimental setup: The scapula was bolted onto a plate with the glenoid surface oriented vertically. The arm was positioned at 60° GH abduction in the scapular plane. An X –Y table allowed adjustment of the humerus relative to the glenoid in the posterior–anterior and proximal–distal directions. The X –Y table was fixed to the bench through a six-axis force sensor (JR3). Another X –Y table was used to translate the scapula in the medial–lateral and inferior–superior directions. The displacements of the two X –Y tables were measured by four linear potentiometers. Three precision rotary potentiometers were used to measure the humeral abduction, flexion, and axial rotation. placements of the two X –Y tables were measured by four linear potentiometers (Midori America Co., Fullerton, CA, USA) as well as by the micrometers built into the X –Y tables. The humeral abduction, flexion, and axial rotation were measured by three precision rotary potentiometers. The six-axis force sensor was used to measure the restraining forces and moments exerted onto the humerus caused by translations of the humerus relative to the glenoid (Fig. 1). Glenoid coordinate system: Anatomical axes were defined to be in line with the posterior–anterior (X ), inferior–superior (Y ), and medial–lateral (Z) axes of the glenoid coordinate system (Fig. 2). The þY -axis was directed superiorly from the most inferior edge of the glenoid to the biceps long head origin (Novotny et al., 2000), and þX -axis pointed anteriorly perpendicular to the þY . The þZ-axis pointed laterally for the right shoulder and medially for the left shoulder and perpendicular to the X and Y axes. The origin of the coordinate system was located at the center of the humeral head. Protocol: Before dissecting the shoulder specimen with all muscles intact, the anatomical neutral position of the humeral head was measured by digitizing landmarks on the humerus and scapula using a digitizer (MicroScribe-3D, Immersion Corp., CA, USA), with the arm positioned at 60° GH abduction in the scapular plane. The landmarks were marked by inserting small pins into the bony landmarks. The following bony landmarks were chosen for the scapula and humerus: The most superior point of the acromio-clavicular joint, angulus inferior, angulus superior, angulus acromialis, and trigonum spinae on scapula, and the epicondylus 109 Fig. 2. Anatomical axes of the glenoid coordinate system for the right shoulder. The þY -axis is directed superiorly from the most inferior edge of the glenoid to the long head of biceps origin, and þX -axis points anteriorly perpendicular to the þY -axis. The þZ-axis points laterally for the right shoulder. The origin of the coordinate system is located at the center of the humeral head. The humerus coordinate system (XH ; YH ; ZH ), which was aligned with the force-sensor coordinate system was also given here. medialis, epicondylus lateralis and one arbitrary point on the humeral shaft. After separating the muscles, the center of the humeral head was aligned with the center of glenoid as follows: First, the humeral head was pressed manually by about 20 N compressive load into the glenoid fossa to ensure concentric reduction of the humeral head in the socket (Hawkins and Bokor, 1990) and the compressive load was then released to let the humeral head back to the neutral medial–lateral position; second, the neutral axial rotation of the humerus was located by positioning the bicipital groove about 45° externally rotated relative to the scapular plane and close to the mid-point between full passive internal and external rotation (Warner et al., 1992); third, the above mentioned digitized data was used to correct any malalignment of the humeral head at the neutral position by using the orientation of the local coordinate systems including the absolute distance between the origins of these systems. After experiment, additional landmarks on the humeral head and glenoid surface were digitized to define the local coordinate systems for the humerus, scapula and glenoid (Makhsous, 1999). In selected specimens, the humeral head center was defined by fitting a hemisphere to the humeral head. Before the testing, the shoulder was elevated up and down about 20 times to minimize the viscoelastic effect of the soft tissue. Restraining forces were measured statically when the humerus was translated relative to the glenoid in the posterior–anterior (X ¼ 16 to 16 mm) and inferior– superior (Y ¼ 10 to 5 mm) directions by adjusting the micrometers at the increment of 4.0 (i.e. X ¼ 16, )12, )8, )4, 0, 4, 8, 12, 16 mm; a total of nine data points), and 2.5 mm (i.e. Y ¼ 10, )7.5, )5, )2.5, 0, 2.5, 5 mm; a total of seven data points), respectively, at a fixed lateral translation (Z ¼ 0, 2.5, 5 mm) in the neutral position of the humeral head. In this way 9 7 ¼ 63 data points 110 M. Makhsous et al. / Clinical Biomechanics 19 (2004) 107–115 were collected in a posterior–anterior/inferior–superior plane at each fixed lateral position. The order of translation of the humerus along the X and Y axes was randomized at a fixed Z translation. A period of 10 s between two consecutive positions was used to minimize the hysteretic effect of the capsuloligamentous structure during the passive movement. The restraining force was monitored during the passive translations to avoid excessive loading of the joint structure. The experimental protocol was tested using two shoulder specimens in order to find appropriate initial position. It was also tested to find reasonable range of translations along the anatomical axes. In order to evaluate contributions of the passive GH capsuloligamentous structure and active muscle tone contraction to joint stability, the test was repeated with no muscle load (Passive condition) and with 1% maximum muscle force on all muscles or muscle portions proportional to the muscle physiological cross-sectional area (PCSA) (Active condition) (Makhsous, 1999; Morrey and An, 1990), representing the physiological muscle tone contraction (Basmajian and De Luca, 1985; Makhsous et al., 1998; Walsh, 1992) during free arm suspension. For the calculation of the PCSA for individual specimen, we used a set of PCSA (Makhsous, 1999) (Table 1). Data analysis: Forces and moments were transformed from the force-sensor coordinate system into the glenoid coordinate system with components in the posterior– anterior (X ), inferior–superior (Y ) and medial–lateral (Z) directions. Force vector fields were used to characterize the direction and magnitude of the restraining forces applied to the humeral head by the GH capsuloligamentous structure and muscles during the passive movement. At each GH position, shear force measured in the posterior–anterior/inferior–superior (sagittal or X –Y ) plane was illustrated by small arrows with the length and direction corresponding to the force magnitude and direction, respectively. Table 1 The muscle forces (N), mean (SD) Muscle 1% maximal muscle force (N) Deltoid Ant. Deltoid middle Deltoid Post Teres minor Long head of biceps Upper subscapularis Middle subscapularis Lower subscapularis Upper infraspinatus Middle infraspinatus Lower infraspinatus Supraspinatus 6.68 5.28 6.20 2.36 3.28 3.26 3.35 4.59 4.33 4.30 4.66 3.28 (2.10) (3.22) (0.02) (0.55) (0.25) (1.80) (1.05) (1.44) (1.80) (1.39) (1.71) (0.25) The 1% maximal muscle forces (N) for each of the shoulder muscles are based on the data from Makhsous (1999). Stiffness of the GH capsuloligamentous structure and muscles crossing the GH-joint, defined as the ratio of the incremental force required to stretch the passive/active structures over a range of translation (Ki ¼ DFi =DTi , i ¼ (post, ant, inf and sup)), was calculated for each direction of translations starting from the neutral position. A least square regression was used to calculate the slope of the fitted line to the collected data points for each direction of translation. The line of action of the shear force (F) exerted onto the humeral head in the sagittal plane of the glenoid coordinate system was characterized by the directional cosine (DC) as follows: qffiffiffiffiffiffiffiffiffiffiffiffiffiffiffiffi Fx Fy DCx ¼ ; DCy ¼ ; FS ¼ Fx2 þ Fy2 FS FS where FS is the magnitude of the shear force, and Fx and Fy are the restraining force components applied to the humerus along the glenoid X and Y axes, respectively (Zhang et al., 1998). Considering the 3D total restraining force (FT ), the corresponding directional cosines (DCTx , DCTy , DCTz ) are determined. Fx Fy DCTx ¼ ; DCTy ¼ ; FT FT qffiffiffiffiffiffiffiffiffiffiffiffiffiffiffiffiffiffiffiffiffiffiffiffiffiffiffi FT ¼ Fx2 þ Fy2 þ Fz2 DCTz ¼ Fz ; FT A mixed effect model was used to test the hypothesis that GH stiffness (the response variable) in the anterior, posterior, superior, and inferior directions are not statistically different (P R O C M I X E D , SAS statistical software package). The main effect of direction (the anterior, posterior, superior, and inferior) was assessed in a random effects model that accounted for specimen as a random effect. Stiffness in the different directions from the same specimens was treated as paired samples in the analysis. The Bonferroni correction method was used to adjust the level of statistical significance for testing six pairwise multiple comparisons. This method was also used to test whether muscle loads increased stiffness along each of the four directions, based on paired samples in the specimens. Paired t-test was used to compare the stiffness in each direction between with and without muscle loading conditions. To evaluate the correlation between the GH stiffness at different directions (Kant , Kpost , Kinf and Ksup ), Pearson’s productmoment correlation coefficients (PCC) were calculated between each pair of the directions over all specimens. 3. Results Passive condition: The restraining force varied systematically with the passive posterior–anterior and inferior–superior translations (Fig. 3). The capsuloligaments generated considerable restraining forces at the M. Makhsous et al. / Clinical Biomechanics 19 (2004) 107–115 27% (P ¼ 0:018), 23% (P ¼ 0:049), 10% (P ¼ 0:054) and 8% (P ¼ 0:049) in the posterior, superior, inferior and anterior directions, respectively (Table 3). Multiple comparison of the stiffness between each pair of directions showed that Ksup was significantly higher than Kpost (P ¼ 0:002), Kant (P ¼ 0:002), and Kinf (P ¼ 0:032) at 5 mm lateral translation. Shifting the humerus superiorly with Sup ¼ 5 mm and Lat ¼ 0 mm increased Kpost and Kant significantly by 21% (P ¼ 0:021) and 18% (P ¼ 0:026), respectively. On the other hand, shifting the humeral head inferiorly (Inf ¼ 10 and Lat ¼ 0 mm) significantly increased only Kpost by 30% (P ¼ 0:028). With the humeral head at the extreme anterior translation (Ant ¼ 16 mm) Ksup increased 31% (P ¼ 0:031). extreme translations (Table 2). At the extreme translations, the restraining force pointed along the line of passive translation and towards the neutral position, as indicated by the DCx and DCy (Table 2). The restraining force generated by the capsuloligaments increased linearly (Fig. 4(a) and (b)), indicating constant stiffness (slope of the force–displacement curve). Translating the humeral head superiorly resulted in the highest resistance force and stiffness (P < 0:008) among all the directions. Kinf and Ksup at the zero anteroposterior and lateral translations were higher than Kpost and Kant at the zero superior–inferior and lateral translations (Fig. 4(c) and (d) and Table 3). When the capsuloligaments were stretched laterally by 5 mm, the stiffness of the capsuloligaments increased Inf - Sup (mm) Passive Lat = 0 Y 5 X 0 -5 -5 -10 Active Y 5 0 -10 111 X -10 0 10 -10 0 10 Post-Ant(mm) Post-Ant(mm) Contour(10, 20,...N) Fig. 3. Representative restraining force field as a function of posterior–anterior (X -axis) and inferior–superior (Y -axis) translations and at Lat ¼ 0 mm for the passive, and active conditions. The contour lines are given at 10; 20; 30; . . . N for force field diagrams. The dots indicate the rim of the glenoid surface. The origin in the force field corresponded to the neutrally aligned position between the humeral head and glenoid. The arrows represent the resistance forces induced by the passive displacements. The length and direction of the arrows represent the magnitude and direction of the resistance force, respectively. Table 2 The magnitude of shear force (FS ) and the corresponding directional cosines (DCx and DCy ) in Mean (SD) Load condition Position (mm) FS (N) Passive Lat ¼ 0 Ant ¼ 16 Post ¼ 16 Sup ¼ 5 Inf ¼ 10 Ant ¼ 16, Sup ¼ 5 Post ¼ 16, Sup ¼ 5 Ant ¼ 16, Inf ¼ 10 Post ¼ 16, Inf ¼ 10 34.9 34.9 46.1 38.6 57.1 52.9 51.1 54.3 (23.3) (16.6) (17.3) (15.5) (20.5) (18.4) (21.0) (16.5) Lat ¼ 0 Ant ¼ 16 Post ¼ 16 Sup ¼ 5 Inf ¼ 10 Ant ¼ 16, Sup ¼ 5 Post ¼ 16, Sup ¼ 5 Ant ¼ 16, Inf ¼ 10 Post ¼ 16, Inf ¼ 10 53.8 52.5 50.9 47.9 76.2 71.0 75.0 70.5 (19.2) (29.1) (26.6) (14.5) (19.1) (17.3) (16.5) (14.6) Active P 0.003 0.069 0.165 0.132 0.029 0.036 0.023 0.008 DCx DCy )0.96 0.94 0.09 )0.13 )0.68 0.68 )0.84 0.65 (0.07) (0.06) (0.24) (0.14) (0.23) (0.22) (0.10) (0.19) )0.16 )0.07 )0.97 0.98 )0.63 )0.66 0.52 0.72 (0.16) (0.38) (0.04) (0.02) (0.12) (0.28) (0.16) (0.19) )0.96 0.96 0.05 )0.22 )0.80 0.75 )0.69 0.58 (0.05) (0.04) (0.22) (0.20) (0.16) (0.11) (0.07) (0.10) 0.02 )0.17 )0.98 0.93 )0.50 )0.64 0.72 0.80 (0.24) (0.28) (0.03) (0.09) (0.12) (0.13) (0.06) (0.08) The FS , DCx and DCy exerted onto the humeral head at the extreme translations in the sagittal plane, i.e. anterior (Ant ¼ 16 mm), posterior (Post ¼ 16 mm), superior (Sup ¼ 5 mm), inferior (Inf ¼ 10 mm), anterosuperior (Ant ¼ 16, Sup ¼ 5 mm), posterosuperior (Post ¼ 16, Sup ¼ 5 mm), anteroinferior (Ant ¼ 16, Inf ¼ 10 mm) and posteroinferior (Post ¼ 16, Inf ¼ 10 mm), and at Lat ¼ 0 mm under the passive and active conditions. P -values were given for differences between the passive and active load conditions. M. Makhsous et al. / Clinical Biomechanics 19 (2004) 107–115 F (N) 112 80 40 0 -8 -400 8 -80 X (m m ) post ant -16 (a) K (N/mm) 8 6 * P<0.001 + 4 16 -10 -5 (b) 8 * P<0.001 6 P=0.011 50 25 0 -25 0 -50 Y (mm) inf 5 sup * P<0.008 + * 4 2 2 0 Y=0 Kpost (c) 0 Kant (d) X=0 Ksup Kinf Fig. 4. Representative force–displacement relationship of the GH-joint at Lat ¼ 0 mm: (a) in the anterior (þX ) and posterior (X ) directions at zero superior–inferior translation (Y ¼ 0); (b) in superior (þY ) and inferior (Y ) directions at zero posterior–anterior translation (X ¼ 0). Passive stiffness (over six specimens) at Lat ¼ 0 mm: (c) Kpost and Kant at the zero inferior–superior translation (Y ¼ 0 mm); (d) Kinf and Ksup at zero posterior–anterior translation (X ¼ 0 mm). No muscle load was applied during the test. The P -values were given when the stiffness was compared to Ksup () or to Kinf (+). Table 3 GH-joint stiffness (K): mean (SD) Loading conditions (starting) (mm) Kant Kpost Ksup Kinf Absolute Change Absolute Change Absolute Change Absolute Change (N/mm) (%) (P) (N/mm) (%) (P) (N/mm) (%) (P) (N/mm) (%) (P) – – 0.049 0.026 0.278 2.89 3.66 3.50 3.76 – 27 21 30 – 0.018 0.021 0.028 5.83 (0.92) 7.18 (2.10) – 23 – 0.049 4.32 (1.07) 4.77 (0.87) – 10 – 0.054 7.65 (1.39) 7.77 (1.86) 31 33 0.031 0.080 4.52 (2.42) 5.26 (0.93) 5 22 0.419 0.067 6.81 (1.79) 7.47 (1.60) 17 10 0.048 0.029 4.93 (1.08) 5.67 (1.36) 14 15 0.047 0.174 8.32 (1.98) 7.77 (1.41) 22 14 0.031 0.138 5.60 (0.95) 5.59 (0.92) 13 13 0.083 0.039 Passive Lat ¼ 0 Lat ¼ 5 Lat ¼ 0 Lat ¼ 0 Lat ¼ 0 Lat ¼ 0 (0) (0)a (Sup ¼ 5)a (Inf ¼ 10)a (Ant ¼ 16)a (Post ¼ 16)a 3.67 3.97 4.32 3.85 Active Lat ¼ 0 Lat ¼ 5 Lat ¼ 0 Lat ¼ 0 Lat ¼ 0 Lat ¼ 0 (0)a (0)b (Sup ¼ 5)b (Inf ¼ 10)b (Ant ¼ 16)b (Post ¼ 16)b 4.32 4.32 4.50 4.31 (1.32) (1.62) (1.45) (1.74) (1.17) (1.74) (1.44) (1.59) 8 18 5 18 0 4 0 0.026 0.496 0.139 0.489 3.60 4.02 3.62 3.99 (0.79) (1.04) (1.24) (1.11) (1.15) (1.31) (1.38) (1.18) 24 12 1 11 0.014 0.076 0.442 0.050 The absolute values (N/mm; first column) and changes (%; second column) in the K for different loading conditions (passive and active), different directions (the anterior, posterior, superior and inferior), and with the humeral head at the neutral position and at the extreme translations (Ant ¼ 16, Post ¼ 16, Sup ¼ 5 and Inf ¼ 10). The starting position of the GH-joint is given under loading conditions, for example the 1st row shows the stiffness values across the range of anterior, posterior, superior and inferior translations at fixed lateral displacement (Lat ¼ 0). The P -values were given when the stiffness was compared to passive condition at Lat ¼ 0a or to active condition at Lat ¼ 0b . a Relative to passive condition at Lat ¼ 0. b Relative to active condition at Lat ¼ 0. Active condition: Loading the muscles at 1% of their maximal forces increased the restraining forces considerably, as indicated by the shrinkage of the contour curves and the faster rise of the restraining forces with the passive displacements (Fig. 3). Compared with the passive condition, FS increased 54% (P ¼ 0:003), 34% (P ¼ 0:029), 34% (P ¼ 0:036), 47% (P ¼ 0:023), and 30% (P ¼ 0:008) in the anterior, anterosuperior, posterosuperior, anteroinferior, and posteroinferior directions (Table 2), respectively. The FT at the active condition was increased by 62% (P ¼ 0:024) and 62% (P ¼ 0:016) in the anterior and posterior directions, respectively. Active tone contraction of muscles crossing the GHjoint increased Kpost , Kant , Ksup and Kinf significantly by 24% (P ¼ 0:014), 18% (P ¼ 0:026), 17% (P ¼ 0:048), and 14% (P ¼ 0:047), respectively, when the muscles crossing the GH-joint were loaded (Table 3). Under the active M. Makhsous et al. / Clinical Biomechanics 19 (2004) 107–115 condition, Ksup (6.81 N/mm) was significantly higher than Kinf (4.93 N/mm, P ¼ 0:034), Kant (4.32 N/mm, P ¼ 0:005), and Kpost (3.60 N/mm, P < 0:001). Laterally stretching the capsuloligaments 5 mm with active muscle loading increased Ksup by 10% (P ¼ 0:029). Ksup was significantly higher than Kpost (P ¼ 0:002) and Kant (P ¼ 0:005) (Table 3). Moving the humerus to the extreme anterior and posterior positions increased Ksup by 22% (P ¼ 0:031) and Kinf by 13% (P ¼ 0:039), respectively. GH Stiffness in the different directions were (P < 0:001) correlated to each other significantly (Table S1 supplementary data). The GH stiffness under active condition had significantly higher correlation (PCC > 93%) than that at the passive condition (PCC > 90%). 4. Discussion The study provides us quantitative characterization of the functionally relevant multi-axis stiffness provided by the GH capsuloligamentous structures and active structures along the posterior, anterior, inferior and superior directions, and at different lateral humeral positions. The multi-axis stiffness was evaluated in the same shoulder specimens so that the stiffness properties along different axes were closely matched to each other for each shoulder specimen. GH stiffness in the superior, inferior, anterior, and posterior directions are correlated to each other but are different in amplitude. Evaluation of stiffness in all four anatomical directions in the same specimens closely matched the stiffness properties among the different axes for each shoulder specimen, which minimized the experimental error associated with specimen variations and provides us a functionally relevant multi-axis characterization. The 60° GH abduction at the neutral axial rotation was chosen in this study, which was found to be a position with large GH laxity in all directions (Halder et al., 2001a; Debski et al., 1999b; Warner et al., 1992; Harryman et al., 1990). The translations used in the experiment were not excessive. Even larger GH displacements ( P 20 mm) were used by some investigators, which was believed not likely to damage the specimens during repeated testing (Harryman et al., 1990; Helmig et al., 1993). In addition to the reported lateral translations (Z ¼ 0, 2.5, 5 mm), the GH-joint was also translated to Z ¼ 2:5 mm. The GH-joint could not be translated more than 3–4 mm at this position due to glenoid bony constraint. In order to avoid potentially overloading the joint structure, the restraining force was monitored during displacements in our study. The range of peak resistance force (Fi ) observed at the extreme position of the translations in the sagittal plane of the glenoid surface in our study were 32–90 N, 28–80 N, 35– 62 N and 33–70 N for the anterior, posterior, superior and inferior displacements, respectively. 113 Within the range of load tested, the resistance force increased approximately linearly with the displacement with the relationship characterized by the corresponding stiffness. A linear relationship between the force and displacement was reported previously during clinical examination of the GH-joint (McQuade et al., 1999) and during in vitro anterior–posterior loading of the GHjoint capsule (Debski et al., 1999b). Larger translations and lower stiffness were observed in the anterior–posterior directions than that in the superior–inferior directions, possibly related to the shapes of the glenoid and the labrum, which are more curved in the superior–inferior direction than in the anterior–posterior direction (McPherson et al., 1997). In a study of stability ratios (Halder et al., 2001b), the humeral head was found to be more stable in the superior–inferior direction than in the anterior–posterior direction with the reason given as the deeper glenoid labral concavity in the inferior–superior direction than that in the posterior–anterior direction. Comparisons of the stiffness in the posterior–anterior or inferior–superior axes indicated that the GH stiffness was higher in the superior and anterior directions than that in the inferior and posterior directions, respectively. In a study of the static capsuloligamentous restraints to superior–inferior translation, higher stability was found in the superior direction than in the inferior direction at three positions of GH abduction (0°, 45°, 90°) (Warner et al., 1992). The higher superior stiffness of the capsuloligaments may be helpful in preventing the impingement of the humeral head into the coracoacromial arch. Compared with the passive condition at zero lateral displacement, the stiffness was significantly increased for all directions of translations with physiological load indicating higher joint stability in all directions. Moreover, under active condition, no significant difference was found among the GH stiffness in the inferior, anterior and posterior directions. The stiffness increased relatively more quickly where the passive joint stiffness was relatively low, i.e. for Kpost (increased 24%) and Kant (increased 18%). This was consistent with the previous finding (Debski et al., 1999a) that the tension in the muscles crossing the GH-joint increased significantly more the posterior stability than the anterior stability. The active condition used in this study resembled the condition under which a clinical static stability test is usually performed. In these tests, although the patient is asked to be as relaxed as possible, the muscle tone always exists even without voluntary contraction (Matsen et al., 1990). The results suggested that low-level muscle activity, representing physiological muscle tone contraction, is important and effective in stabilizing the GH-joint (Makhsous et al., 1998; Kumar and Balasubramaniam, 1985; Moseley and Overgaard, 1962; Symeonides, 1972). The muscle tone contraction is 114 M. Makhsous et al. / Clinical Biomechanics 19 (2004) 107–115 difficult to measure and it is not available in the literature. A pilot study was done (Makhsous et al., 1998) to identify muscle tone contraction with 90° and 45° of humeral abduction in the scapular plane. The muscle tone was found to be within 1–7% of the maximum muscle contraction and in this study the lowest muscle tone level was used. When the humeral head is translated laterally, the capsule and ligaments were stretched as indicated by the higher GH stiffness (Table 3) and restraining force (Table S2 supplementary data) for all the direction. Current established GH-joint models in the literature usually allow unrestricted translations in the medial– lateral direction when the humerus was moved in the posterior–anterior or inferior–superior directions to evaluate GH laxity (Halder et al., 2001a; Weiser et al., 1999; Debski et al., 1999b). In this study, we took a different approach and evaluated multi-directional GHjoint stiffness at several fixed medial–lateral positions, with the multi-axis resistance force acted on the humeral head by passive and active restraints measured by a sixaxis force sensor at a fixed medial–lateral position. In other words, we measured the multi-axis resistance force at controlled GH positions and used the force–displacement relationship to characterize the multi-axis GH stiffness. To avoid excessive load to the glenoid, the resistance force was limited/controlled to be within a pre-specified range. Furthermore, the resistance force in the medial–lateral as well as other directions at controlled GH positions provides useful information on the stabilizing contributions of the passive and active structures including the labrum and glenoid. The study provided quantitative measures of the GH stiffness in all anatomical directions obtained from the same specimens. This helps us understand the roles of the capsuloligaments and muscles in GH stability, analyze GH injury, and develop more accurate mathematical models of the GH-joint. A better understanding of the different but interrelated passive and active GH stiffness evaluated along multiple axes may help us interpret the results of multi-axis laxity tests and evaluate shoulder laxity at different conditions. Low-level muscle tone activity was effective in stabilizing the GHjoint as it made the joint stiffer along all the axes with reduced difference among the different directions. Further work needs to be done to characterize contributions of the individual structures (muscles and ligaments) and the influence of arm positions over a large sample of specimens, which were limitations of the above study and should be addressed in further studies. Acknowledgements The project was supported in part by Arthrex, Inc. (LZ), NIH (LZ), and Falk Medical Research Trust. We would like to thank Maria D. Knoll, PhD, for her assistance on the statistical analysis. References Basmajian, J.V., De Luca, C.J., 1985. Muscle alive: Their functions revealed by electromyography. Williams & Wilkins, Baltimore. Blasier, R.B., Soslowsky, L.J., Malicky, D.M., Palmer, M.L., 1997. Posterior glenohumeral subluxation: active and passive stabilization in a biomechanical model. J. Bone Joint Surg. 79-A, 433– 440. Debski, R.E., Sakone, M., Woo, S.L.-Y., Wong, E.K., Fu, F.H., Warner, J.J., 1999a. Contribution of the passive properties of the rotator cuff to glenohumeral stability during anterior–posterior loading. J. Shoulder Elbow Surg. 8, 324–329. Debski, R.E., Wong, E.K., Woo, S.L.-Y., Sakane, M., Fu, F.H., Warner, J.P., 1999b. In situ force distribution in the glenohumeral joint capsule during anterior–posterior loading. J. Orthop. Res. 17, 769–776. Halder, A.M., Halder, C.G., Zhao, K.D., O’Driscoll, S.W., Morrey, B.F., An, K.N., 2001a. Dynamic inferior stabilizers of the shoulder joint. Clin. Biomech. 16, 138–143. Halder, A.M., Kuhl, S.G., Zobitz, M.E., Larson, D., An, K.N., 2001b. Effects of the glenoid labrum and glenohumeral abduction on stability of the shoulder joint through concavity-compression. J. Bone Joint Surg. Am. 83-A, 1062–1069. Harryman, D.T.I., Sidles, J.A., Clark, J.M., McQuade, K.J., Gibb, T.D., Matsen, F.A., 1990. Translation of the humeral head on the glenoid with passive glenohumeral motion. J. Bone Joint Surg. Am. 72, 1334–1343. Hawkins, R.J., Bokor, D.J., 1990. In: , Matsen III, F.A. (Ed.), The Shoulder, vol. 1. W.B. Saunders Co., Philadelphia, pp. 149– 177. Helmig, P., Sojbjerg, J.O., Sneppen, O., Loehr, J.F., Ostgaard, S.E., Suder, P., 1993. Glenohumeral movement patterns after puncture of the joint capsule: an experimental study. J. Shoulder Elbow Surg. 2, 209–215. Kumar, V.P., Balasubramaniam, P., 1985. The role of atmospheric pressure in stabilizing the shoulder. An experimental study. J. Bone Joint Surg. Am. 67B, 719–721. Makhsous, M., 1999. PhD Thesis, Department of Polymetric Materials, Chalmers University of Technology, Gothenburg, Sweden, ISBN 91-7197-7810-7190. Makhsous, M., Palmerud, G., Ericson, K., H€ ogfors, C., 1998. Influence of tonus, elastic stress and submaximality in static contraction of shoulder muscles. Studia I Monografie AWF we Wroclawiu 55, 41–48. Malicky, D.M., Soslowsky, L.J., Kuhn, J.E., Bey, M.J., Mouro, C.M., Raz, J.A., Liu, C.A., 2001. Total strain fields of the antero-inferior shoulder capsule under subluxation: A stereoradiogrammetric study. J. Biomech. Eng. 123, 425–431. Matsen III, F.A., Thomas, S.C., Rockwood Jr., C.A., 1990. In: Matsen III, F.A. (Ed.), The Shoulder, vol. 1. W.B. Saunders Co., Philadelphia, pp. 526–560. McPherson, E.J., Friedman, R.J., An, Y.H., et al., 1997. Anthropometric study of normal glenohumeral relationships. J. Shoulder Elbow Surg. 6, 105–112. McQuade, K.J., Shelley, I., Cvitkovic, J., 1999. Patterns of stiffness during clinical examination of the glenohumeral joint. Clin. Biomech. 14, 620–627. Morrey, B.F., An, K.-N., 1990. Biomechanics of the shoulder. In: Rockwood Jr., C.A., Matsen III, F.A. (Eds.), The Shoulder, vol. 1. pp. 208–245. M. Makhsous et al. / Clinical Biomechanics 19 (2004) 107–115 Moseley, H.F., Overgaard, B., 1962. The anterior capsular mechanism in recurrent anterior dislocation of the shoulder. J. Bone Joint Surg. Br. 44, 913–927. Novotny, J.E., Beynnon, B.D., Nichols, C.E., 2000. Modeling the stability of the human glenohumeral joint during external rotation. J. Biomech. 33, 345–354. Soslowsky, L.J., Malicky, D.M., Blasier, R.B., 1997. Active and passive factors in inferior glenohumeral stabilization: a biomechanical model. J. Shoulder Elbow Surg. 6, 371–379. Symeonides, P.P., 1972. The significance of the subscapularis muscle in the pathogenesis of recurrent anterior dislocation of the shoulder. J. Bone Joint Surg. Br. 54, 476–483. Ticker, J.B., Warner, J.J.P., 2000. Selective capsular shift technique for anterior and anterior–inferior glenohumeral instability. Clin. Sports Med. 19, 1–17. 115 Walsh, E.G., 1992. Muscles, Masses and Motion. The Physiology of Normality, Hypotonicity, Spasticity and Rigidity. Blackwell Scientific Publications Ltd., New York, Oxford. Warner, J.P., Deng, X.H., Warren, R.F., Torzilli, P.A., 1992. Static capsuloligamentous restraints to superior–inferior translation of the glenohumeral joint. Am. J. Sports Med. 20, 675–685. Weiser, W.M., Lee, T.Q., MaMaster, W.C., McMahon, P.J., 1999. Effects of simulated scapular protraction on anterior glenohumeral stability. Am. J. Sports Med. 27, 801–805. Zhang, L.-Q., Butler, J.P., Nishida, T., Nuber, G.W., Huang, H., Rymer, W.Z., 1998. In vivo determination of the direction of rotation and moment–angle relationship of individual elbow muscles. J. Biomech. Eng. 120, 625–633.