* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Basic Bacterial Culture and Identification
Quorum sensing wikipedia , lookup
Microorganism wikipedia , lookup
Antimicrobial surface wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Antibiotics wikipedia , lookup
Marine microorganism wikipedia , lookup
Triclocarban wikipedia , lookup
Human microbiota wikipedia , lookup
Bacterial taxonomy wikipedia , lookup
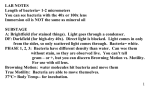
Page 1 of 10 Basic Bacterial Culture and Identification Mary T. Johnson, Ph.D. Culture of Normal Flora Organisms MATERIALS: • • • • Sterile cotton swab Bacteriological loop Nutrient Agar plates Biohazard discard container STUDENT DIRECTIONS: 1. Carefully swab the selected skin surface site in an area approximately 4 cm in diameter. Swab thoroughly, rotating the swab to ensure that a good inoculum has been obtained. 2. Transfer the bacteria to the agar culture dish by touching the swab to the agar surface in a single spot. Once you feel confident that a good inoculum has been transferred, the swab can be discarded in the biohazard container. 3. With the inoculating loop, proceed to streak in a second and third streak pattern (see illustration). Briefly, isolate bacterial colonies by pulling several streaks out from the original swab inoculum site. Use the method shown above to avoid tearing the agar. Basic Bacterial Culture and Identification Page 2 of 10 4. Incubate the plate at 37oC for 24-48 hours. 5. Test the colonies that have grown by Gram staining; identify Staphylococcus aureus colonies by testing Gram-positive cocci using a specific latex agglutination reagent that binds to Staphylococcus aureus. Pure Culture Techniques Microbiologists have developed special techniques and equipment to isolate and grow pure cultures of microorganisms that are free from contaminating forms. This exercise is designed to give the student an introduction to these special techniques. It is important that techniques be practiced until some degree of skill is developed. Pure cultures are essential when identifying unknowns. During the course of the semester, each student will be expected to develop independently a patient-oriented case to correlate with each of 4 separate bacterial isolates. It is important, therefore, to maintain unique isolates in pure culture to be submitted with each case summary. Further instruction will be given during later labs. THE STREAK PLATE TECHNIQUE The procedure of streaking a plate with an inoculating loop is used to spread millions of cells over the surface of a solid medium so that some individual cells are deposited at a distance from all others. These cells grow and reproduce, forming an isolated colony. One or more colonies will be well separated from all others and represent a source of a pure culture. The procedure is similar to the one used for streaking from the collection swab. MATERIALS: • • • • Streak plates from the previous lab session Nutrient agar plates (NA) Bunsen burner Bacteriological loop Basic Bacterial Culture and Identification Page 3 of 10 STUDENT DIRECTIONS: Examine the streak plates prepared during the previous lab period and locate a number of well-isolated colonies. Now you must transfer a portion of each colony to a separate agar slant. To "pick" a colony you will be using an inoculating loop. Sterilize the loop in the burner flame, let cool 3-5 seconds then touch the end of the loop to the isolated colony, picking up the microorganisms from the colony. Now re-cover the streak plate and pick up one NA plate. You will now be holding the inoculating loop in your right hand and the fresh NA plate in your left (lefties reversed). Remove the lid from the plate, place the inoculating loop at one edge of the plate and with a sweeping stroke, inoculate the agar using the same tri-streak method as used for the initial isolation. Replace the lid. Flame the loop and proceed to inoculate another plate from different colonies. Try to use colonies that are visibly different in morphology. Incubate the plates in the 37oC incubator until the next class period. There is nothing difficult about picking colonies and inoculating slants, but you must avoid contamination. TESTS FOR SUSCEPTIBILITY TO ANTIMICROBIAL AGENTS Bacteria generally can be grouped with respect to antibiotic susceptibility. Gram positive bacteria are more permeable to many of the most common antibiotics, probably because they lack the outer membrane of the Gram negatives. This makes them more susceptible as a group to the actions of antimicrobial agents. However, generalizations concerning susceptibility and resistance are difficult to make because of the vast differences in bacterial species. In addition, the emergence of new antibiotic resistant strains in particular environments makes it increasingly important to adequately monitor resistant strains. On a global scale, outbreaks of Shigella, E. coli and Salmonella carrying drug-resistance plasmids have emphasized the need to monitor drug resistance within populations and to make this information widely available. KIRBY-BAUER DISC METHOD One simple and commonly used assay for microbial susceptibility is the disc diffusion or Kirby-Bauer method, which will be demonstrated. Antibioticimpregnated discs release antibiotic into the surrounding medium when placed on the surface of solid agar. Untreated agar plates are inoculated with test microorganisms and antibiotic discs are placed on the agar surface. Disc diffusion is a qualitative method based on an approximation of the effect of Basic Bacterial Culture and Identification Page 4 of 10 antibiotic on bacterial growth on a solid medium. A zone of growth inhibition around the antibiotic disc will occur if the organism is susceptible to the antibiotic. As the distance from the disc increases, there is a logarithmic decrease in antibiotic concentration. Standardized regression curves have been developed that correlate inhibition zone size to the minimum inhibitory concentration of the antibiotic. However, even though it is the most common test for antimicrobial effectiveness, not all bacteria can be tested using disc diffusion. MATERIALS: • • • • • • Bacterial cultures Sterile loops Antibiotic discs Agar plates Bunsen burner Striker STUDENT DIRECTIONS: 1. Light the bunsen burner and let it burn for five minutes to create a clean work environment. 2. With an inoculating loop, pick one colony from the plate you inoculated during the previous class. You will use it to grow a lawn of tiny bacterial colonies. 3. Use the loop to distribute the bacteria completely over the surface of the agar. Where you previously needed to streak for isolated colonies, now you are streaking for maximum distribution over the surface of the agar. Turn the plate 90o and streak the entire surface again. 4. Repeat step #3 until you are satisfied with the amount of bacteria you have deposited on the agar. 5. Use the antibiotic disc dispenser to release several discs onto the agar Basic Bacterial Culture and Identification Page 5 of 10 surface. Press down with another bacteriological loop to secure. 6. Observe the growth pattern after at least 24 - 48 hours of growth (standard read time is 48 hours). MINIMUM INHIBITORY CONCENTRATION (MIC) and MINIMUM BACTERICIDAL CONCENTRATION The minimum inhibitory concentration (MIC) method uses doubling dilutions of antibiotics solubilized in bacteriological medium to assess the susceptibility of specific bacteria to the antimicrobial agents selected. The MIC test measures the lowest concentration of an antibiotic that inhibits the visible growth of test microorganisms. In practice, microtiter plates containing prediluted antibiotics in lyophilized form are reconstituted and incubated along with test bacteria. Once an MIC has been performed a minimum bactericidal concentration (MBC) can subsequently be determined. The MBC is set up with subcultures made from each MIC well that appears visually clear. The MBC is the concentration of antibiotic included in the first tube from which colonies calculated as less than 99.9% growth is recovered. Basic Bacterial Culture and Identification Page 6 of 10 Comparison of Kirby-Bauer and MIC test results: Bacterial Staining THE GRAM STAIN The Gram stain exploits the basic differences in the outer layers of bacteria so that certain bacterial groups retain the initial stain while others readily lose this dye during the decolorization process. Bacteria that decolorize will be stained the color of the counterstain. The first two clues to the identification of any bacterium is the shape of the organism and the Gram staining characteristic. In fact, in some situations need no further information is needed (at least at the beginning) and you will come across microbiologists referring toan isolated organism as a "Gram-negative rod" or a "Gram-positive coccus". With more experience in microbiology, this information actually tells you a great deal about the genus to which the organism belongs. MATERIALS: • • • Gram stain solutions Microscope slides Agar plate cultures of Escherichia coli and Staphylococcus aureus STUDENT DIRECTIONS: To perform the Gram stain, a good smear is absolutely essential. Too thick a smear will produce a slide giving false positive reactions. Too thin a smear will require lots of time seeking organisms on the slide. Basic Bacterial Culture and Identification Page 7 of 10 1. Prepare a good smear • • • • Place one drop of water on a microscope slide. With an inoculating loop, pick one colony; place colony in the drop of water and make a milky suspension. Allow the smear to air dry. Heat-fix the smear by passing the slide over the burner flame several times. Take care not to overheat (overheating will lyse the cells). Test the temperature by placing the slide on the back of your hand. If it’s too hot for your hand, it’s too hot for the bacteria. 2. Flood the slide with crystal violet stain and leave for 1 minute. 3. Pour off the crystal violet stain, wash with water, and flood the slide with Gram’s iodine solution. Allow a contact time of 1 min. 4. Gently rinse the slide with water from a squirt bottle. 5. Blot the slide dry to remove excess water with a Kimwipe. 6. Holding the slide on a slant, flood the slide with the combination 95% acetonealcohol/safrinin solution, watching for the dye to continue washing from the cells. As soon as most of the crystal violet dye stops leaching from the cells, gently wash the slide in water to stop the decolorization process. Be careful not to overdo this step. 7. Blot the slide dry or allow to air dry. The critical step is #6, the decolorization process. In all probability it will take some practice to train your eye to detect when the dye has stopped leaching from the cells. Too thick a smear will protect cells lying beneath the top cells from becoming decolorized. In this case a Gram negative organism will appear Gram positive. Many Gram-positive cultures will appear Gram-negative or Gramvariable if the cells are over-decolorized. Is it very likely that Gram-negative cocci would be cultured from a normal skin swab? You should start this exercise by preparing a slide with 2 smears, one from a Gram positive coccus (off your normal flora plates) and the Gram negative rod (Escherichia coli). The presence of the two smears adjacent to one another will not affect the Gram stain, but it will let you see the difference in decolorization between the two organisms. After staining one slide, examine the results under the microscope using the oil immersion objective. If you fail to see the red-pink rod-shaped Escherichia or if the cocci are not a deep purple, try the stain again with another slide--this time correcting the decolorization step (longer or shorter). A Candida albicans culture is also interesting to examine in comparison with Gram-positive bacteria. Basic Bacterial Culture and Identification Page 8 of 10 Other Bacterial Staining Methods THE ACID-FAST STAIN The property of acid-fastness, which is detected by the acid- fast stain, is primarily of clinical application to detect members of the genus Mycobacterium. M. tuberculosis, the etiologic agent of tuberculosis, is the most common pathogen of this group. Other microorganisms, particularly the Nocardia, can be identified by their acid-fast characteristic. The term acid-fast is derived from the resistance displayed by acid-fast bacteria to decolorization by acid once they have been stained by another dye. Cultures provided: MATERIALS: • • • • Mycobacterium phlei culture Prepared Kinyoun carbol fuchsin stain 3.0% acid-alcohol (70% ethanol containing 0.5% hydrochloric acid) Methylene blue counterstain STUDENT DIRECTIONS: 1. Prepare a bacterial smear in the conventional manner (as for Gram-staining), air-dried and heat fixed. Flood the smear with Kinyoun carbol fuchsin reagent and allow to remain in contact for at least 5 min. Do not allow the stain to dry out Basic Bacterial Culture and Identification Page 9 of 10 - add more if needed. 2. Rinse the excess stain off with deionized water from the squirt bottle. Tilt the slide to drain water. 3. Decolorize the smear with acid alcohol until the color no longer runs from the smear. It is difficult to overdecolorize acid-fast bacteria. 4. Wash the smear with deionized water (use the squirt bottle). 5. Counterstain for 30 sec -- 1 min. with 1% methylene blue. 6. Rinse thoroughly, blot dry, and examine under oil immersion. 7. Study the stained preparation using the light microscope. A blue-stained mass can usually be found on low-power. Examine the mass with the oil-immersion lens. On high power, acid-fast bacteria will appear an intense, crimson red (retaining the carbol fuchsin), while the remaining material will be blue from the counterstain. THE METHYLENE BLUE STAIN The Methylene Blue Stain is considered to be a simple stain, in contrast with the Gram and Acid-Fast Stains, which require a counterstaining step. Methylene Blue Stain is especially useful for observing metachromasia in bacterial species such as Corynebacteria. MATERIALS: • 1% Methylene blue stain solution • Glass microscope slides • normal flora cultures STUDENT DIRECTIONS:Prepare a bacterial smear, as above. 1. Flood with methylene blue solution. 2. Leave stain in contact with the smear for 30 sec -- 1 min. 3. Rinse thoroughly, blot dry, and examine under oil immersion. Basic Bacterial Culture and Identification Page 10 of 10 Basic Bacterial Culture and Identification