* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download IFP Plans_022004
Survey
Document related concepts
Transcript
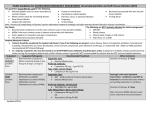
Schedule of covered services (Continued) Benefit description Other services Rehabilitative therapy includes physical, speech, occupational, respiratory and cardiac therapy 5 Chiropractic care (12-visit calendar year maximum) Mental health services for severe conditions 5,7 8,9 Mental health for non-severe conditions5,7,8,10 Durable medical equipment (including foot orthotics) Outpatient prescription drugs 11,12 Filled at participating pharmacy (up to a 30-day supply); not covered at non-participating pharmacies, Filled through mail order (up to a 90day supply) Twice the Level copayment 1. 2. PPO Value Basic 35 In-Network 1 Out-of-Network 2 Negotiated fee until out-of-pocket maximum is met, then covered in full. No benefits until out-of-pocket maximum met, then covered in full 20 visit maximum per calendar year Not covered Not covered $350 + 35% inpatient / 35% $350 + 50% inpatient / 50% Outpatient Outpatient $350 + 35% inpatient/ Negotiated fee until out-of-pocket maximum is met, then covered in full out patient $350 + 50% inpatient / not covered outpatient 50% ($500 calendar year max.) Not Covered $15 Copay (Generic Only) Not covered Of negotiated rate, the rate the Participating or Preferred Provider has agreed to accept for providing a covered service. Percentage is a portion of the covered expense based on (C& R) Customary & Reasonable. You are also responsible for any charges in excess of the covered expense. 3. Mammograms are covered at the following intervals: One for ages 35-39, one every 24 months for ages 40-49, and one every year for age 50 and older. 4. The emergency room and urgent care copay are waived if admitted to the hospital for an emergency. The emergency room and urgent care copay are per visit and do not apply to the out-of-pocket maximum. The calendar year deductible applies to emergency room visits. 5. Certain services require prior certification from Health Net. Without prior certification, benefit reduced by 50%. 6. Maximum Allowable charges are $600 per day. 7. Covered expenses incurred for non-severe mental illness and chemical dependency do not apply to the out-of-pocket maximum. 8. The inpatient/outpatient copay applies to the OOP accumulation and continues to apply once the out-of-pocket maximum is met. 9. The following are considered severe mental illness: schizophrenia, schizoaffective disorder, bipolar disorder, major depressive disorders, panic disorders, obsessive-compulsive disorder, pervasive development disorder or autism, anorexia nervosa, serious emotional disturbances in children under age 18. 10. Non-severe mental illness inpatient maximum payable per day is $300, benefit maximum is 30 days; if covered by the plan, outpatient non-severe mental illness is $30 maximum payable per visit, 20 visits maximum per year. 11. Generic Drugs which are not listed on the Recommended Drug List and Brand Name Drugs are not covered. The Recommended Drug List is a list of the prescription drugs that are covered by this plan. It is prepared by Health Net and given to member physicians and participating pharmacies. Some drugs require prior authorization from Health Net. Also, if your condition requires the use of a drug that is not in the Recommended Drug List, your physician may require the drug through the prior authorization process. Urgent prior authorization requests are handled within 72 hours. For a copy of the Recommended Drug List, call Member Services at the number listed on your ID card or visit our web site at www.healthnet.com. Prescription drug charges do not apply to your maximum out-of-pocket limit. 12. Medical calendar year deductible waived. EFFECTIVE OCTOBER 1, 2004 HEALTH NET LIFE INSURANCE COMPANY INDIVIDUAL & FAMILY PLAN PPO PLANS Principal benefits and coverage matrix — PPO THIS MATRIX IS INTENDED TO BE USED TO HELP YOU COMPARE COVERAGE BENEFITS AND IS A SUMMARY ONLY. THE POLICY SHOULD BE CONSULTED FOR A DETAILED DESCRIPTION OF COVERAGE BENEFITS AND LIMITATIONS. Benefit Description Value Basic 1500 1 In-Network Provider Annual deductible (subscriber only plan) Annual out-of-pocket maximum Lifetime Maximum Visit to physician 3 X-ray and laboratory procedures $1,500 $4,000 combined in-network and out-of-network (includes deductible) $6 million Negotiated fee until OOPM is No benefits until OOPM is met, met, then covered in full then covered in full Negotiated fee until OOPM is No benefits until OOPM is met, met, then covered in full then covered in full Preventive care Routine physical exams, including routine lab and X-ray services Annual OB/GYN exam (breast and pelvic exams, cervical cancer screening and 4 mammography) Prostate cancer screening and exam Immunizations Standard To meet foreign travel or occupational requirements Child preventive care (1 to age 18); checkups, vision and hearing exams Child preventive care Immunizations Allergy testing and injection services Not covered 25% Alcohol detoxification 7 Not covered 25% Not covered Not covered Not covered 25% Not covered 25% Not covered Negotiated fee until OOPM is met, then covered in full No benefits until OOPM is met, then covered in full Maternity and pregnancy Prenatal and postnatal office visits Maternity care in hospital Emergency and urgent care Emergency room (professional and facility charges) Urgent care center (facility charges) 3 Ambulance 3 Inpatient Hospital services (non-emergency care) Physician/surgeon and anesthetics services Organ and bone marrow transplants (nonexperimental and noninvestigational) 2 Out-of-Network Provider Not covered Not covered 25% 25% 25% 25% 25% 25% 25% 50% 25% Not covered 25% 50% 5 3 days per calendar year combined in-and-out-of-network IFP20040718 r EFFECTIVE OCTOBER 1, 2004 HEALTH NET LIFE INSURANCE COMPANY INDIVIDUAL & FAMILY PLAN PPO PLANS Summary of Benefits continued Benefit Description Value Basic 1500 1 In-Network Provider 2 Out-of-Network Provider 3 Hospital and skilled nursing facility (facility charges) 5 Inpatient, semiprivate hospital room or 25% 50% intensive care unit with ancillary services (unlimited, except for mental health and substance abuse treatment) 5 Outpatient surgery 25% 50% 5 Skilled nursing facility 25% 50% (100-day annual limit combined in- and out-of-network) Reproductive health Sterilization 25% not covered Other services Home health services (limited to 60 visits per 25% 50%, $75 maximum payable per calendar year combined in- and out-ofday 3 network) 3 Hospice services 25% 50% Rehabilitative therapy (includes physical, Negotiated fee until OOPM is No benefits until OOPM is met, speech, occupational, respiratory and met, then covered in full then covered in full 3 cardiac therapy) Limited to 20 visits per calendar year combined in- and out-ofnetwork Chiropractic care Not covered Acupuncture Not covered 5 Mental health services for severe conditions 25% Inpatient / Negotiated fee 50% inpatient / No benefits until until OOPM is met Outpatient OOPM is met then covered in full then covered in full Outpatient Mental health services for nonsevere 6,7 conditions 1 2 3 4 5 6 7 8 25% Inpatient / Negotiated fee until OOPM is met then covered in full Outpatient Durable medical equipment (including foot 50% 3 orthotics) ($500 Calendar year max) Corrective footwear ($200 maximum payable 50% 3 per calendar year) 3 Prosthetics and corrective appliances 25% 8 Outpatient prescription drugs Filled at participating pharmacy (up to a 30$15 copay (generic only) day supply); not covered at non-participating pharmacies, Filled through mail order (up to a 90-day supply) Twice the Level copayment 50% inpatient/ not covered outpatient Not covered Not covered 50% Not covered Of negotiated rate, the rate the Participating or Preferred Provider has agreed to accept for providing a covered service. Percentage is a portion of the covered expense based on (C&R) Customary & Reasonable. You are also responsible for any charges in excess of the covered expense. Certain services require prior certification from Health Net. Without prior certification, benefit reduced by 50%. One mammogram for ages 35-39, one every 24 months for ages 40-49, and one every year for age 50 and older. Allowable charges are $600 per day. Treatment of non-severe mental disorders is limited to Participating or Preferred Providers for outpatient services, with the following maximums: 20 outpatient visits, $30 maximum payable per outpatient visit; 30 inpatient days per calendar year; and a maximum allowable limit per day for inpatient services of $300. Covered expenses incurred for non-severe mental illness and chemical dependency do not apply to the out-of-pocket maximum. Generic Drugs which are not listed on the Recommended Drug List and Brand Name Drugs are not covered. The Recommended Drug List is a list of the prescription drugs that are covered by this plan. It is prepared by Health Net and given to member physicians and participating pharmacies. Some drugs require prior authorization from Health Net. Also, if your condition requires the use of a drug that is not in the Recommended Drug List, your physician may require the drug through the prior authorization process. Urgent prior authorization requests are handled within 72 hours. For a copy of the Recommended Drug List, call Member Services at the number listed on your ID card or visit our web site at www.healthnet.com. Prescription drug charges do not apply to your maximum out-of-pocket limit. IFP20040718 r