* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Document
Survey
Document related concepts
Transcript
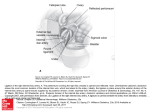
#5 Anatomy مجد معـدي 12/11/2015 َلوه د .محمد ع َّ Anatomy lecture 5 Awn 2015 Anatomy lecture #5 DIGESTIVE SYSTEM 12th /Nov/2015 The last lecture was mainly about the muscles of the abdominal wall & the rectus sheath. We said that the rectus sheath forms in the developmental stages during the 6 th and the 7th weeks (at the emporyological stage ) because of this kind of developing one of its specific characteristics is that its missed inferiorly at the level of the anterio-superior iliac spine. We also talked about the contents of the rectus sheath: two muscles, four blood Vessels (Sup. & Inf. epigastric arteries, Sup. & Inf. epigastric veins), six nerves • This lecture cover the slides (18-33) in the Antero-Lateral Abdominal Wall file & introduction to the ingunal canal. Slides are NOT included. Blood Vessels of Abdominal Wall The doctor explained the blood vessels depending on the origin of the blood vessel. The internal thoracic artery is the artery that descend externally downward (parastrunal) beside the sternum and provide the anterior intercostals artery to the level of the sixth intercostals space where it branch into two arteries : - The musculophrenic artery : which will go to the abdomen. - The superior epigastric artery. Note: The abdominal wall term refer to the antero-lateral abdominal part NOT just the rectus sheath. For example in the rectus sheath there are two arteries and two veins (four blood vessels), while in the antero-lateral abdominal wall in general there are more than four vessels and one of the most important arteries is the superior epigastric artery In the anterolateral abdominal wall region the Superior epigastric artery is the continuation of the internal thoracic artery .once it gets into the abdominal wall it enters the rectus sheath (pass through the posterior sheath and the rectus abdominal muscles.) Because its located behind the rectus sheath it provide will the blood supply to mainly the Transversalis Fascia, the posterior rectus sheath and rectus abdominal muscle ,so all in all it 1 Anatomy lecture 5 Awn 2015 provides the blood supply to the deep superior structures of the abdominal wall even to the umbilical level. The decending thoracic aorta ( which is the largest artery in the body) gives the last three thoracic arteries which are the 10th and the 11th posterior intercostel arteries and the subcostal artery. As they descend they will provide blood supply along with other four lumber arteries which also branches from the descending thoracic aorta. As these 7 blood vessels descend they will pass between the two deepest muscles layers the internal oblique and the transverses abdominal muscles, at the same time they give branches to the superficial structures. The other thoracic arteries provide the superficial anterior abdominal wall. In the last lecture the external iliac artery was mentioned as the artery that will descend at the level of the Inguinal ligament to give the femoral artery. Another important branch of the external iliac artery is the inferior epigastric artery. Above the Inguinal ligament the inferior epigastric artery will arise from the medial aspect of the external iliac artery , as it pass from the medial aspect it will move medially to the deep Inguinal ring ( which is the entrance or the deep opening to the Inguinal canal) when it reach the deep abdominal cavity it will penetrate the transverse fascia to get into the antero lateral abdominal wall, then it will ascend between the transversalis fascia and the rectus abdominas until the level of the arcuate line. At the arcuate line it will enter within the rectus sheath and will bind to it (posteriorly to the rectus sheath, anteriorly to the rectus abdominals). At the level of the umbilical it will anastomosis with the superior epigastric artery. The superior and the inferior epigastric arteries are the main arteries in the antero lateral abdominal wall. 2 Anatomy lecture 5 Awn 2015 In addition to these arteries there are several other arteries for example the deep circumflex iliac artery that also branch from the external iliac artery, the importance of this artery is that it provide blood supply to the deep structures in the inguinal region in the abdominal wall. Notice that all the branches from the external iliac artery are deep branches like the inferior epigastric artery and the deep circumflex artery The other branches are from the femoral artery that we mentioned in the last lecture and early in this lecture its located below the Inguinal region, its branches are superficial not deep like the external iliac artery. The femoral artery will give the superficial epigastric artery which will go to the superficial structures in the anterior wall below the level of the umbilical. So in the lower part of the anterior wall the blood supply to the deep structures ( rectus abdominas and posterior sheath) is by the inferior epigastric however the blood supply to the skin and the superficial fascia is by the superficial epigastric artery. Another artery that provide the superficial structures is the superficial circumflex iliac artery, by this you can notice, there are two circumflex iliac artery to the inguinal region: 1. The deep one arising from the external iliac artery and it provide blood supply to the deep structure in the inguinal region. 2. The superficial one which arise from the femoral and provides blood to the superficial structures in the inguinal region ( the skin and the superficial fascia). 3 Anatomy lecture 5 Awn 2015 The innervations of the abdominal wall We discussed the six thoracic nerves in the rectus sheaths last lecture we mentioned a nerve that does not enter the rectus sheath because it’s a lower level which is the first lumber spinal nerve (L1), this nerve is the innervations for the anterio-lateral abdominal region. The first lumber spinal nerve will divide into upper and lower branches which are: (there names start with illio because they come from the iliac region) 1. Illiohypogastric nerve: (the upper branch) named hypogastric because it goes to the hypogastric area. 2. Illioinguinal nerve (the lower branceh) The picture : The borders of the antero lateral abdominal wall : Superiorly : the costal margins Superiorly at the middle: the xiphoid process Inferiorly: the inguinal ligament at the middle: the umbilicus the midline: the lena alba there are seven nerves in the antero-lateral abdominal wall The first nerve from the lower 6 thoracic nerves, provide T7 innervations to the upper part, comes from the most common medial part of the costal cartilage. Provide innervations for the umbilical region, comes from the lower end of the costal margin/ at the lower rib of costal margin. Cover the sensationally the area between the xiphoid process and T8,T9 the umbilical region. T11,T12 Branch in an arcuate manner. As this nerve pass between the transverses abdomens and the L1: internal oblique muscles it divide into two branches: T10 4 Anatomy lecture 5 Awn 2015 Ingiohypogastric nerve: provide the iliohypogastric region and the ilioinguinal region superiorly. Ilioinguinal nerve : this branch will pass through the superficial inguinal ring which is the medial triangular shaped opening and it split into the aponeurosis external oblique. Provide the lower inguinal region and the pubic sympghysis area. clinically when there is a disease or an injury or rupture in one of the abdominal organ or viscera you will not feel pain from this, the pain will go with the anatomical innervations from the diseased organ passing with splanchnic nerve up to the center nervous system then this pain will be referred down with the sensory spinal nerves into the abdominal wall, this is what we call the referred pain. The main areas from referred pain It’s a pain in your abdominal wall but it's actually originating from a visceral source or organ, we consider it as indication for the diseased organ. The diseased organ Where the pain is felt the stomach pain in the epigastric region, this area in innervated by T7 the small intestine and the pain in the umbilical region, cecum and the appendix innervated by T10 the large intestines pain in the iliohypogastric area, innervated by T10 & L1 the bladder pain in the pubic symphysis area, innervated by ilioingunal nerve This is important in the early discovery of the Appendicitis in early stages to detect this inflammation as early as possible before the burst of the appendix. In appendicitis at the early stages the pain will be a referred pain in the umbilical region when the appendix enlarge it will start irritating the parietal peritoneum this will shift the pain to down into lower right inguinal region, it will become a real pain not referred. 5 Anatomy lecture 5 Awn 2015 Surface Anatomy There are several classifications to divide the antero-lateral abdominal wall the general clinicians decided to divide the abdominal wall to make it easier to distinguish the organ the patient complain from. General clinicians use general classification which is to divide the wall into four abdominal quarters (this is the division that you will be using here) in this division we have two lines ( horizontal line and vertical line) and will divide the wall into four quarters (upper right, upper left, lower right, lower left). These two lines are: - the midsagittal line or medial line which divide the abdominal wall into left and right parts. - The horizontal line which we call it transumbilical plane (pass through the umbilicus, located at the level of intervertebral disks between L3 & L4) despite the fact that the area of umbilicus varies sometimes between individuals, it is still within the same limits. By learning this you will be able to distinguish the defected organ so when a patient is complaining from this region and there is pain during palpation in the upper quarter for example you will know that the problem might be in the liver or any organ in this region. However the more common is the division to nine regions by two vertical lines and two horizontal planes: The vertical lines are the midclavicular planes pass from the middle of the clavicle to the med point of the inguinal ligament The horizontal planes the sup costal one at the lowest margin of the costal 6 Anatomy lecture 5 Awn 2015 cartilages of T10 its located at the level of the third lumbar vertebrae L3, the another line is the trans-tubercular plane passes through the tubercles of the iliac crest which are the elevations located at the top area of the iliac bone laterally remember these tubercles are important because they are the insertion area for the illiotebial tract. this plane is at the level of L5. These four lines will divide the abdominal wall into nine regions. We can't say that this classification is not used we use it for example: The right area is called the right hypochondria ( below cartilage which refer to the costal cartilage here) is the area where we will find the gallbladder to be specific at the tip of the 9th costal cartilage is the fungus of the gallbladder. Notice the right lumber and the right lingual area (named Inguinal because its close to the ingunal ligament) in the meddle we have epigastric/stomack area below the sup costal plane in the middle there is the umbilical region (in the umbilical region you can find the small intestines mainly the jejunum and the ilium, notice also the pubic/hypogastric below the stomach and below the trans-tubercular plane. On the left notice the left hypochondilic , left lumber and left Inguinal region. beside these divisions, there is a very important plane you have to know about because of its clinical importance which is the transpyloric plane. physicians use this plane as a landmark. Its named transpyloric plane because it pass through the pylorus of stomach. its located at the level of L1 vertebrae and usually from the tip of the ninth costal cartilage to the other 9th costal cartilages so to find it just follow the costal margin of the 9th costal cartilage if you find this difficult you can distinguish it by the linea semilunaris, where the linea semilunaris is crossing this is the area of the ninth costal cartilages. Because this plane is a horizontal line and pass through several important structures and easy to palpate over it and demarcate. 7 Anatomy lecture 5 Awn 2015 What are the structures that can be identified by the transpiorenic plane? (From right to left) Put your fingers on the costalcartilage and ask the patient to take a deep breath the first thing you can palpate at the tip of the 9th costal cartilage is the fungus of the gallbladder, if the patient Note: feels a deep pain because we are pressuring The hilum means the entrance / over this area this means the patient is where the roots of the organ enter having an inflamed gallbladder. This is how or leave . in the kidney we have you palpate to do a cholecystectomy. medial hilum where the roots pass(the roots here are the renal Secondly it will pass pylorus of stomach. arteries, renal veins, the uretar) so Thirdly it will pass by the neck of the in any organ you will have a hilum pancreases ( any pain in this area indicate and a root. mostly pancreases tumors). Then it will pass through the duodenum jejunum junction. Finally it will pass through the hilum of the kidney . Abdominal Surgical Incisions Surgeons use various incisions to gain access to abdominal cavity, the surgical incisions are not much used nowadays, but they are still important during the exploratory operations The most common replacement these days is the laparoscopic surgery (using a laparoscope) in this kind of surgery we do three small openings. What is the difference between the laparoscopies surgery and the endoscopic surgery? The laparoscopic we make artificial three small openings In endoscopic surgery we enter through a natural opening in the body (nasal opening, oral opening,…..) The basic principles and roles to follow during the Surgical Incisions: 1. Provide adequate exposure: to gain a proper access you have to provide an adequate exposure in the proper location, in some surgeries you will have to work in an area of inflammation or tumors it doesn’t make any sense to open small opening of 1 cm, for example if you are working on the 8 Anatomy lecture 5 Awn 2015 liver you should open an adequate opening in the left side in the left hypochondria. 2. Avoid damage to major vital structures : open as much as you can as long as you are not harming other structures or vital structures which are the VAN structures ( Veins, Arteries, Nerves). By now you already know that the nerves goes more or less horizontally so cutting the anterior and antero-lateral abdominal wall vertically is not allowed (because by this you will cut the whole innervations) except in the midline because in the midline at the linea alba there are only fibrous tissue no innervations . so all in all always pay attention to how the orientation or the direction of the VAN to avoid damage them. 3.provide the best possible cosmetic effect: you have to follow the dermatome to provide a scar healing which is easy sometimes. Sometimes because of the severity of the disease the surgeon has to do more effort. Common surgical incisions: The common surgical incisions are divided into two types: 1) The vertical incisions: not the common, they are three in number but only two are used • the midline or the median incisions 2) The transverse or oblique incisions: • Kocher’s (Sub costal) Incision • McBurney’s Incision Median (Midline) Incisions common to use, it for exploratory operations when you want a large abscess for a sever tumor or sever infection in one organ and you want to remove it like the removal or transplantation of the liver. Why is this incision used? Because at the midline (at the linea aspera) there is less blood supply and its easy to cut and stretch the linea aspera. 9 Anatomy lecture 5 Awn 2015 However the risk here is that if the surgeondon’t line the edges of the linea aspera probably because of the pour blood supply an ischemic necrosis might develop after the surgery. The medial incisions are three types : 1- The upper median incision : from the xiphoid to the umbilical 2- The lower median incision : from the umbilical to the pubic symphysis 3- The complete median incision : used mainly for the exploratory operations and transplantation of large organs. Paramedian Incision: Usually 2-5 cm lateral to the midline. Usually for small organ transplantations that happen on the left side for example working on the spleen or the kidney. How we use this incision for the kidney transplantation? First We open a lower paramedian incision then we put the transplanted kidney (the healthy kidney) in the iliac fossa over the iliac muscles, the surgeon cut the ureter and stitch it to it the surgeon do not remove the diseased kidney we always leave it as it is also the surgeon do not interfere with the renal arteries and renal veins he put tubes from the healthy kidney to the external iliac directly. When the surgeon wants to do a paramedian incision he does not cut the whole abdominal wall. First he cut the skin then the superficial fascia then the deep fascia (anterior rectus sheath) he continues the cutting until he reaches the rectus abdominas because if he continues the cutting he will cut the rectus abdominal longitudinally which will lead to cut the nerves and the medial side of the muscle will undergo necrosis because by this he will cut the blood supply to the medial part of the rectus abdominal and the innervations ( thoracic spinal nerve). 10 Anatomy lecture 5 Awn 2015 What the surgeon do instead of cutting The surgeon do a paramedical cut until he reach the rectus abdominas muscle he don’t cut it he use a retractor to reflect the rectus abdominas laterally with the anterior rectus sheath. After that he continuo cutting posteriorly the rectus sheath to get into the extra paretonuim fat. Note: There is an incision called pararectus incision or the semilunar incision, its very risky and not operated any more. Kocher’s (Subcostal) Incision: Its an incision in the right side usually to a 0.5 cm below the costal margin. Used in cholecystectomy Even though laparoscopic surgery are used a lot these days they cannot by used if the gallbladder is severely pain or bursted so we use open surgery using kocher's incision. This incision is 2.5 cm below the costal margin and its not straight the surgeon follow the costal margin. Kocher is referring to Emil Theodor Kocher its very important to know about this scientist specially in the surgery. He wasn’t only the first Swiss citizen to win the noble prize he was also the first surgeon to win the Nobile prize. He won the Nobel prize for his procedure on the thyroid gland and for developing an antiseptic method by this method he reduced the risk of surgical infections for less than 1% in his surgery (the antibiotics was not used yet). He is famous for one of the surgical instruments he used the "homeostatic forceps" or "kocher's forceps" still used nowadays in surgery rooms the new instruments like the electrocautery procedure have reduced the use of these old instruments. 11 Anatomy lecture 5 Awn 2015 The kocher's forceps is a serrated adages forceps with interdigitating teeth at the tips, its used to ligate the blood vessels during the operation so if you want to cut an artery first you have to put the kocher's forceps one before and one after to completely close the arterial blood movement in the artery by this you can close between them. McBurney’s Incision It is an oblique incision on the spino- umbilical line, the other scientific name is gridiron incision. For open appendectomy. What is the spino- umbilical line? Spino- umbilical is a straight line connect between the anterior superior iliac spine with the umbilical so in the spinoumbilical line if you go one third from the spine and two third from the umbilical and do a cut you are at this point at the base of the appendix ( we need the base of the appendix not the apex to do a cut in the appendix, in this kind of surgery we remove all the appendix and don’t leave anything unlike the kidney transplantation) so this area is called McBurney's bond. the McBurney's incision was described by the American surgeon Charles Heber McBurney. We call the incision At McBurney's bond the McBurney's incision and the gridiron incision but you can do the gridiron incision at any region in the body. what is Gridiron incision? This term can be used in different regions in the body. Gridiron incision is what is called in surgery the muscle splitting incision when you have muscle fibers directed in different orientation like in the costal muscles (external intercostals muscles and internal intercostals muscles and the transverses thoracic muscles). Another example is the muscles in the abdomen (external oblique and internal oblique and transverse abdominal). 12 Anatomy lecture 5 Awn 2015 this name come from the Gridiron frame that’s used in fixing or repairing the ships once they put the ship in this thing it will has horizontal and longitudinal and vertical frames around the ship these frames run perpendicular to each other. this is similar to the orientation of the muscles fibers in the Gridiron incision. We use this incision to prevent losing the muscles like the oblique muscles if you cut the area horizontally you will cut the fibers of the muscles so we lose the muscle. In this incision if we want to remove the appendix, we cut the oblique muscles following the orientation of the fibers then we retract the muscle , then we will cut the internal oblique muscles the second incision should be perpendicular to the first incision, then we retract the internal oblique muscles then we cut the transverse muscles horizontally the third incision should be perpendicular to the second incision, we produce the gridiron incision by producing perpendicular incisions. then you will get into the abdominal cavity then you reflect the cecum (because appendix is most of the time retrocecul -behind the cecum)then you remove the appendix. (please check for it in other sources because it wasn’t clear from the record). Pfannenstiel (Suprapubic) Incision: -The smile incision / c-shaped incision / funnel steal incision. -it is Transversed but slightly curved incision & 5 cm above the pubic. -It’s the most commonly used incision because its used in common surgeries like the Caesarean section (in delivery) ,c-section surgeries, its also used in hysterectomy in some cases of tumors and when we want to remove the uterus , we use it in urinary bladder diseases and in prostate surgery in males. The describer of this incision Hermann Johannes Pfannenstiel while he was performing his incision for a woman that have an ovarian abscess he 13 Anatomy lecture 5 Awn 2015 injured his finger and because the antibiotics wasn’t discovered yet he died from septicemia, he was only 47. Inguinal Region the second abdominal wall PowerPoint presentation In the last lecture the doctor explained the formation of the Inguinal canal, he explained also the three openings, the superficial ring in the external oblique and the tearing in the aponeurosis, the arching fibers of the internal oblique and the higher arching fibers of the transverses abdomenas muscles. Then when the testes descend within its structure they will pull the transeversalis facsia with it. It will pass behind the transversus abdominis (which origin is the lateral 3rd of the inguinal ligament), then it will pass through the internal oblique (which is from lateral half to lateral two 3rds),this will make the lowest fibers of internal oblique in touch with the transversalis fascia, all in all, transversalis fascia which is covering the testes will also touch the internal oblique fibers and take them because this is during the embryological development, so as the fibers form to become the cremaster muscle, and lastly it will pass through the triangular split, but it's not yet complete so when the testis pass it will take the remaining fibers and matrix with it and this is how the spermatic fascia forms . When speaking about the structure of the inguinal ligament remember the word "MALT" (from up to down): -M: the roof is Muscles (the lower arching fibers of transversus abdominis and the lower arching fibers of internal oblique). -A: anteriorly is the Aponeurosis of external oblique. 14 Anatomy lecture 5 Awn 2015 -L: below is the inguinal Ligament. -T: posteriorly is the Transversalis fascia. There are two important structures related to this: The conjoint tendon: when the two fibers coming into the pubic symphysis which is too small, so the fibers interdigitate with each other and insert into the pubic symphysis by this they become the conjoint tendon. Note : these fibers will not became aponeurosis because aponeurosis is thin flat tendon. The lacunar ligament which is producing a lacunae. The doctor explained is a small part of the inguinal ligament fibers that reflect this ligament at min 47.5 using a papers I from the pubic tubercle and attach to the pubic ramus couldn’t explain it superiorly. Its important because as its reflected it will here provide a canal or opening called the femoral ring, demarcated laterally by the femoral vein, medially by the lacunar ligament, anteriorly by the inguinal ligament, and posteriorly by the pubic ramus. Through this femoral ring, the lymphatics (superficial inguinal lymph nodes) will pass up from the thigh into the external iliac lymph nodes in the abdominal cavity, so it’s a lymphatic passage. However, the lymphatic vessels are very small on diameter, so mostly the canal is empty. Now the fascia of the abdominal wall like transversalis and iliacus fascia, once lymphatics expand down into the thigh, they will take it with them so they will produce something called femoral canal which extends just 1 cm, and the upper opening of it is the femoral ring which is the opening into a small tube of fascia. 15 Anatomy lecture 5 Awn 2015 Its very important during hernia, if there’s an increased strain in the abdomen, during defecation or parturition in female, a small part of the intestine can pass through the femoral ring downwards as the abdominal pressure is increasing. We call This hernia femoral hernia, and it is more common in females because the ring is wider, because of the wider pelvis. this femoral ring is very rigid since its surrounded by tough structures (laterally the femoral ring, medially the lacunar ligament, anteriorly the Inguinal ligament, posteriorly bones) , so once the intestine passes through it, most of the time it cannot get back, this is why its called irreducible hernia. If the hernia was above the inguinal ligament through the superficial inguinal ring, its called inguinal hernia, while the femoral hernia is below the inguinal ligament, this is distinguished clinically by palpation all the way over to reach the pubic tubercle which is bony prominence, if the neck of the hernial sack was above and medial to the pubic tubercle its inguinal hernia, if it was below and lateral its femoral hernia. Good luck Majd Nabil Mo'adi 16