* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Testosterone_Case Review
Survey
Document related concepts
Transcript
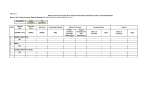
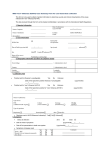
John XXXX DOB: 07/03/YYYY John XXXX – AndroGel/Testosterone Case Review Parameter First name Initial Last name DOB Gender Past Medical History and Risk Factors Social History (Smoking, alcohol, drug use, etc.) Family History Drug Interactions If Any Age at the time of Testosterone use (> or < 65 years) Weight, Height, BMI Details of the patient (At the time of Testosterone use) AndroGel/Testosterone Use Details Findings John D XXXX 07/03/YYYY Male History Of Cardiac Problems: Longstanding hypertension Stroke: No Valve prolapse: No Coronary Artery Disease: No Has he ever been a tobacco user? Yes Period of time smoking: Unknown Heaviness of smoking: 20 pack year exposure Has she quit smoking? Yes When did she quit: 20 years ago DM: (List all family members diagnosed with DM): No Heart Disease: No None 67 years (> 65 years) PDF Ref 14 17 14 14 56 56 Per visit dated 02/14/YYYY; Height: 5 feet, 9 inches Weight: 81 kg Body Mass Index (BMI): 25 kg/m2 Reason for Use: Andropause 20 Topical/Supplemental therapy: Topical 86 86 148, 151153 9, 148, 151-153, 171-174 Start Date: 08/28/YYYY Duration: 08/28/YYYY, 08/29/YYYY, 10/10/YYYY, 10/24/YYYY (Per medical records) Stop Date: Unknown Dosage: AndroGel 5 gm Testosterone lab values (One month prior and after adverse event) *Reviewer's comment: Pharmacy records are not available to know the AndroGel usage details. 09/04/YYYY: Testosterone – 6.6 nmol/L (Ref. range: 6.0-27.0 nmol/L) 33 *Reviewer's comment: Testosterone lab value one month after adverse event is not available for review. Yes 56-61 Diagnosed with Adverse Events (Heart attack/Stroke/DVT/Blood Date of diagnosis: 10/10/YYYY clots/other 1 of 9 John XXXX Cardiovascular events) Whether Testosterone was discontinued? (When and Why) Hospitalization for the adverse event (Admission, length of hospital stay) DOB: 07/03/YYYY Adverse Event Diagnosis: ST-segment Elevation Myocardial Infarction (STEMI) with identified triple vessel Coronary Artery Disease (CAD) and Ventricular Septal Defect (VSD) Did the adverse event occur within 30 days of Testosterone therapy? Yes No *Reviewer's comment: The discharge medications for hospitalization for myocardial infarction contain AndroGel 5 gm. 1st Hospitalization – For STEMI with identified triple vessel CAD and VSD: 10/10/YYYY-10/24/YYYY (15 days) 2nd Hospitalization - For Congestive Heart Failure (CHF): 10/25/YYYY10/28/YYYY (4 days) 171-174 56-61, 8687, 88-92, 100-101, 96-97, 102-103, 185-187 3rd Hospitalization – For refractory CHF: 11/12/YYYY-11/20/YYYY (9 days) 4th Hospitalization – For acute decompensated heart failure: 11/20/YYYY12/02/YYYY (13 days) Complications after Adverse Event Diagnosis Current Condition of Patient (as per last available record) Prior Medical History 5th Hospitalization – For patch dehiscence and VSD: 12/02/YYYY12/08/YYYY (7 days) 10/25/YYYY-10/28/YYYY: CHF 11/12/YYYY-11/20/YYYY: Refractory CHF 11/20/YYYY-12/02/YYYY: Acute decompensated heart failure 12/02/YYYY-12/08/YYYY: Patch dehiscence and VSD 06/05/YYYY: Patient denies chest pain, SOB and Paroxysmal Nocturnal Dyspnea (PND). Prescribed Nitro-Glycerin for CAD/CHF. Past Medical History: Longstanding hypertension, gout 86-87, 8892, 100101, 96-97, 102-103, 185-187 11 56, 86, 151 Past Surgical History: Umbilical hernia repair, colonoscopy Social History: As on 10/28/YYYY: Former smoker – 20 pack year exposure, quit 20 years ago; Excess alcohol consumption, drinking as much as 10-12 drinks in the past per day, but has been abstinent of alcohol for the last year Family History: Non-contributory Allergy: Beer only insofar AndroGel/Testosterone Intake Details (From Pharmacy Bills) Not available *Reviewer's comment: Pharmacy records are not available to know the AndroGel usage details. Duration Medication Prescribed By 2 of 9 Dispensing Pharmacy PDF Ref John XXXX Not available DOB: 07/03/YYYY Not available Not available Not available Not available Missing Medical Record: What Records are Needed Pharmacy records Hospital/ Medical Provider Date/Time Period Why we need the records? Is Record Missing Confirmatory or Probable? Unknown 08/28/YYY Y10/24/YYY Y To know the exact duration of AndroGel use Confirmatory Hint/Clue that records are missing Medical records have evidence for AndroGel use Detailed Chronology DATE PROVIDER 01/06/YYY Multiple YProviders 09/04/YYY Y 10/10/YYY Provider/Hosp Yital 10/24/YYY Y OCCURRENCE/TREATMENT Multiple visits for umbilical hernia: 08/28/YYYY: Patient is diagnosed to have andropause. Prescribed AndroGel pump 5 gm, scheduled 30 days. (PDF Ref: 9) 09/04/YYYY - Labs: (PDF Ref: 33) Testosterone – 6.6 nmol/L (Ref. range: 6.0-27.0 nmol/L) Hospitalization for acute ventricular septal defect complicating inferior ST elevation Myocardial Infarction (MI): Admission diagnosis: ST-segment Elevation Myocardial Infarction (STEMI) with identified triple vessel coronary artery disease and Ventricular Septal Defect (VSD) Secondary diagnoses: ST elevation MI 10/10/YYYY (Late presentation), cardiogenic shock. Gout - Takes Allopurinol for maintenance Hypertension Remote smoker Interventions and major investigative procedures: 10/10/YYYY: Coronary Artery Bypass Grafting (CABG) times 3; Left Internal Mammary Artery (LIMA) to Left Anterior Descending (LAD), Saphenous Vein Graft (SVG) to diagonal one and Obtuse Marginal (OM) and infarct to VSD with VSD repair with pericardial patch. 10/20/YYYY: Left elbow X-ray shows no acute fracture or dislocation post fall. 10/21/YYYY: Postoperative chest X-ray reveals bibasilar atelectasis with small bilateral pleural effusions. 10/22/YYYY: Postoperative echocardiogram to assess VSD shows a 1.0 cm residual VSD and residual tissue around the VSD site. During his hospital stay this patient was transfused with 4 units of frozen plasma, 1 unit of pooled platelets and 1 unit of Packed Red Blood Cells (PRBCs). Course in hospital: Patient presented on 10/10/YYYY with a late presentation inferior 3 of 9 PDF REF 22-23, 25-28, 3-6, 180181, 79, 14, 33 56-57, 35-36, 62-63, 66-75, 108115, 83, 182, 5861 John XXXX DATE PROVIDER DOB: 07/03/YYYY OCCURRENCE/TREATMENT PDF REF ST elevation MI and heart failure. Investigations revealed triple vessel Coronary Artery Disease (CAD) and a VSD. The patient was taken to the Operating Room (OR) on 10/10/YYYY. He underwent CABG and VSD repair with Dr. Xxxx. The procedure was well tolerated. This patient had a prolonged stay in Cardiovascular Intensive Care Unit (CV ICU). He remained there until postoperative day #6. His issues there included: Intraaortic balloon pump which was inserted preoperatively was removed on postoperative day #1. Patient was intubated until postoperative day #2. Patient was received to CV ICU on Milrinone, Levophed and Vasopressin. All were discontinued by postoperative day #3. Patient was fluid volume overloaded requiring treatment with BiPAP and diuresing. This patient was in a junctional rhythm from postoperative day zero to postoperative day #2. He then reverted to a sinus rhythm and remained in sinus rhythm throughout the course of his stay. The patient was transferred to the Cardiac Surgery ward on postoperative day #6. The patient had some confusion on postoperative day #7. It was identified that he had not been sleeping well. He was treated with Seroquel. This improved his sleep wake pattern and resolved his hallucinations and confusion. This was continued for a duration of three days. This patient remained in sinus rhythm throughout his postoperative course. He remained on telemetry until postoperative day #8. This patient was found to have a systolic ejection murmur on postoperative day #11. Echocardiogram was repeated and showed a small residual VSD of 1.0 cm. As the patient was asymptomatic it was not felt that any intervention was required at this time. The patient was advised to monitor for signs of heart failure. He was advised to weigh himself daily, monitor for peripheral edema and shortness of breath. The patient has no dizziness at the time of discharge and again did not have any arrhythmias while in hospital. I have requested this patient see Dr. Xxxx in approximately one week with a repeat echo. The patient’s only other postoperative issue was that of gout. He had an acute gout attack of the left forefoot. He was treated with Colchicine and had quick resolution of his symptoms. This patient is anticoagulated for six months for a VSD patch. Target INR is 2.0 to 3.0. INR at the time of discharge is 3.1. Patient is being discharged home to the support of his family on postoperative day #14, 10/24/YYYY. 10/25/YYY Provider/Hosp Yital 10/28/YYY Y Most responsible diagnosis: Triple vessel coronary artery disease and VSD. Hospitalization for congestive heart failure: History reviewed. Patient was discharged last Thursday after he had an inferior MI and within a few hours was readmitted through the Emergency Department (ED) at XYZ 4 of 9 37-39, 84, 8687 John XXXX DATE PROVIDER DOB: 07/03/YYYY OCCURRENCE/TREATMENT PDF REF Memorial Hospital with Congestive Heart Failure (CHF), has diuresed over the last three days with good response. (ED reports are not available). He says he is feeling back to normal. He has had no arrhythmias documented, no chest pains. His troponin has declined from his previous infarct. No secondary bump. His ECG has shown evidence for his inferior MI but no acute changes. On examination, blood pressure is 100/60, heart rate is 65. He is in a sinus rhythm. Chest examination reveals diminished air entry to both bases but I did not hear any crackles or wheezes. Heart sounds reveal a harsh systolic murmur at the left sternal border, heard throughout the precordium, also into the back. There are no diastolic murmurs heard. Jugular Venous Pulse (JVP) is at the sternal angle with a negative Hepatojugular Reflux (HJR). The sternal and leg wound sites appear to be healing. 10/28/YYYY – Discharge summary: Patient’s Echocardiogram (ECG) shows grade IIIII Left Ventricular (LV), Ejection Fraction (EF) 40% with inferior wall severe hypokinesis, mild global hypokinesis, about a 1 cm residual VSD with a QP QS of 1.7. No pericardial effusion but left pleural effusion is still noted. Pulmonary pressures are mildly elevated. Right Ventricular Systolic Pressure (RVSP) is in the mid 40-45 range. His ECG shows evolving changes of his inferior MI but no acute changes. There were no arrhythmias documented. His renal function has tolerated the bump up of the diuresis. 11/01/YYY Provider/Hosp Y ital His chest X-ray is showing some resolution of his congestive heart failure. His blood work did show him to be anemic, hemoglobin was 10.3. He is therapeutic with an INR of 2.4 on adjusted dose Warfarin, having received 1 mg of Warfarin today. He has diuresed well and is doing well. The congestive heart failure could be representative of his recent MI, LV impairment, residual VSD and volume overload there-from. This does not represent a secondary acute ischemic event. He is eager for discharge home and as he is clinically stable, discharged to home today. He has been put on Nitro-Dur 0.4 mcg patch. He has been reminded to carry Nitro and to seek medical attention for any refractory symptoms. Subsequent followup has been organized and cardiac rehabilitation through my office. Follow-up visit status post MI, CABG and VSD: 10 Patient complains of shortness of breath and chest pain. 11/12/YYY Provider/Hosp Yital 11/20/YYY Y Assessment and plan: MI and VSD – Follow-up in 2 weeks. Hospitalization for refractory CHF: Course in hospital: Patient presented to Emergency Room (ER) on 11/12/YYYY because of acute onset Shortness of Breath (SOB) associated with cough and generalized weakness. He was put on a strict 1.5 grams salt and 1.5 liters fluid restricted diet and was diuresed with Intravenous (IV) Lasix and addition of Metolazone. Advise was given by Dr. Pppp for this patient’s management and since he did not respond much to the diuretics resulting in creatinine creeping up from 148 to 170, bicarbonate increasing from 27 to 38 and a moderate luck with urine output his case was discussed with Dr. Xxxx who transferred him over to ABC Hospital and reevaluated him for the ventricular septal detect, which was most likely contributing to his refractory heart failure. He did have elevated Liver Function Tests (LFTs) with an alkaline phosphatase 5 of 9 88-92, 44-45, 100-101 John XXXX DATE PROVIDER DOB: 07/03/YYYY OCCURRENCE/TREATMENT PDF REF of 298, Alanine Transaminase (ALT) of 228, Aspartate Transaminase (AST) of 98. This bump in the liver enzymes is most likely secondary to congestion from his heart failure. A chest X-ray showed unchanged stable bilateral airspace disease and pleural effusions. During this hospitalization, he did complete a 7-day course of Levaquin and had mild elevation in his white count 13.6; however, his symptoms did not support the diagnosis of pneumonia. I would leave it for the Physicians to decide in ABC whether they want to treat him with another round of antibiotics. After discussing with Dr. Xxxx, his Coumadin was discontinued and he was bridged on Tinzaparin for a possible surgical intervention in the near future. He was discharged on Ferrous Gluconate 300 mg, Lasix 60 mg and Aspirin 81 mg. 11/20/YYY Provider/Hosp Yital 12/02/YYY Y Final diagnosis: Refractory CHF secondary to recent MI resulting in VSD Hospitalization for acute decompensated heart failure: Admitting diagnosis: Acute decompensated heart failure Secondary diagnosis: Significant large residual VSD with a left-to-right shunt Interventions and major investigative procedures: Patient had a 2-D echo that revealed grade I to II out of IV Left Ventricular (LV) function, septal bounce. Basal inferior aneurysmal area. Remaining LV had normal function. The LV was dilated. The Right Ventricle (RV) was hypokinetic and dilated. There was a VSD with a left-to-right shunt, evidence of bilateral pleural effusion, query echodense structure near the Left Ventricular Outflow Tract (LVOT). They wondered if this was part of the VSD closure. His RVSP was 44 mmHg. The CT of his chest 11/26/YYYY showed mixed air space disease and ground glass density in both upper lobes which may be due to edema and infection. Bilateral pleural effusions, larger on the left side with left lower lobe atelectasis. He also had a Transesophageal Echocardiogram (TEE) performed on 11/28/YYYY which showed aortic sclerosis, mild Mitral Regurgitation (MR), mild Tricuspid Regurgitation (TR), RVSP was 46 to 50 mm Hg, the VSD patch was visualized just below the AV valve near the LVOT, and there was evidence of a large residual left-toright shunt. Most responsible diagnosis: Acute decompensated heart failure secondary to a 3 cm hemodynamically significant VSD Post-admit comorbidities: Include refractory heart failure as well as concerns for embolic phenomenon as he did develop black spots in his nail beds of the fingers bilaterally which was felt to be compatible with embolic phenomenon likely from the pericardial patch tissue now in the LV and LVOT as described. He has been on fulldose Enoxaparin during his admission. Summary: Patient remains on a Lasix infusion but has had refractory heart failure. Dr. Xxxx spoke with Dr. Eric Xx at General Hospital for consideration of a percutaneous closure and therefore he was transferred to General Hospital (TGH) today for an 6 of 9 96-97, 9395,9899, 102103 John XXXX DATE PROVIDER 12/02/YYY Provider/Hosp Yital 12/08/YYY Y 12/09/YYY Provider/Hosp Yital 01/01/YYY Y DOB: 07/03/YYYY OCCURRENCE/TREATMENT opinion regarding this matter. He will be admitted under Dr. Vlad xxxxin the Coronary Care Unit (CCU) at General. Once their assessment is done he will be repatriated back to our hospital for discharge planning. Hospitalization for patch dehiscence and VSD: PDF REF 185-187 Patient was transferred to TGH for consideration of percutaneous VSD repair. Unfortunately after careful review of his clinical status, cardiac MRI and CT by the Interventional Radiologists here he was not deemed a candidate for percutaneous procedure. Cardiovascular Surgery was also consulted and it was thought it would be best for the original Surgeon to operate at ABC who was agreeable to this. During his stay at the CCU at General he showed signs of increasing heart failure 3:1 right to left shunt and high wedge pressures. He was treated with Nipride, Milrinone and Lasix infusions. He also developed delirium and confusion during his stay. CT head did not show anything acute to explain his confusion. Follow-up instructions: VSD dehiscence: For repair at ABC where he has been accepted. Patient is being transferred with infusions of Milrinone, Lasix infusion and Nipride via air ambulance. Metolazone was also added for management of his heart failure. Hospitalization for VSD: Admitting diagnosis: VSD Interventions and major investigate procedures: 12/10/YYYY: Redo VSD repair for dehiscence of old VSD patch, repair of left false aneurysm and repair of right femoral artery. 12/10/YYYY: CT head shows a normal exam. 12/12/YYYY: Feeding tube insertion. 12/20/YYYY: Thoracentesis for 425 mL on the right side. 12/20/YYYY: CT chest shows good opposition of sternal fragments with intact sternal wires. 12/23/YYYY: Postoperative echo shows a small residual VSD. QT/QS is 0.9. 12/30/YYYY: Postoperative chest X-ray reveals moderate atelectasis at the right lung base with a residual moderate pleural effusion which is unchanged since previous thoracentesis. During his hospital stay this patient was transfused with 11 units of packed red blood cells, 4 units of frozen plasma, 1 unit of pooled platelets, 1 unit of platelet apheresis, 10 units of pooled cryoprecipitate. Course in hospital: Patient underwent redo VSD repair, repair of the left ventricle for false aneurysm and repair of the right femoral artery on 12/10/YYYY. The operative course was well tolerated. The patient had a prolonged stay in CV ICU. His stay was prolonged secondary to: Postoperative bleeding requiring transfusions. Prolonged intubation. This patient was not extubated until postoperative day #8. Small bowel feeding tube inserted on postoperative day #2 for nutritional 7 of 9 189194, 116, 200, 121122, 117-120 John XXXX DATE DOB: 07/03/YYYY PROVIDER OCCURRENCE/TREATMENT support while still intubated. Postoperative delirium. The patient was agitated and had a very slow neurological progress. Neurologically he was improving by postoperative day #8. Postoperative atrial fibrillation treated with Amiodarone and Metoprolol. The patient was transferred to the Cardiac Surgery ward on postoperative day #9. This patient continued to have a significant delirium. He was seen by the Geriatric Service as well as Psychiatry. The patient’s family had a concern that given his history of bipolar diagnosis that this was something more than a delirium. Neither the Geriatric nor Psychiatry team felt this was anything other than delirium. The patient had no signs of infection. He had good effect with treatment with Seroquel. His hallucinations resolved. His intermittent episodes of confusion also resolved. By the time of his discharge there were no concerns regarding ongoing delirium from the Nursing Staff, the patient or his family. It was recommended the patient remain on Seroquel. This has been continued in the home environment with request for followup with Dr. Ssss for weaning and discontinuing as appropriate. This patient is anticoagulated for his VSD. This should continue for 3 months. He did have some intermittent atrial fibrillation while in hospital. Reassess his rhythm prior to discontinuing Warfarin therapy. He has maintained a therapeutic INR in hospital on 2 mg of Warfarin daily. This patient had hypernatremia on initial transfer to the Cardiac Surgery ward. This resolved and his sodium was 142 at the time of his discharge. This patient did initially have a sternal click. This was not appreciated by the time of his discharge. The patient however did have dehiscence of his distal sternal incision. At the time of his discharge he was receiving Vac therapy. There were no signs of infection and cultures had been negative. He is not on antibiotic therapy at the time of his discharge. Home Care Services have been requested to monitor the incision and complete dressing changes. Vac/negative pressure wound therapy has been requested in the community. This patient did have a significant right pleural effusion in hospital. This was diuresed on postoperative day #10 for 425 mL. He was left with a residual moderate sized right pleural effusion. By serial chest X-ray this was not increasing in size. This patient’s postoperative echo did show a small residual VSD. This was reviewed by Dr. XXXXX and Dr. XX. The results were then communicated to Dr. Xxxx. It was felt that this residual VSD was “insignificant.” Dr. Xxxx has identified that no specific followup is required. Specifically no urgent office assessment or echocardiogram is required at this time. It was relayed to the patient and his spouse. They know to continue to monitor for any signs of failure which could be due to LV dysfunction, or VSD. They also note to monitor for any signs of worsening shortness of breath due to his pleural effusion. This patient was discharged home on postoperative day number 22, 01/01/YYYY. He has been referred to the Cardiac Rehabilitation Program at St. Mars’s General Hospital. 8 of 9 PDF REF John XXXX DATE PROVIDER 01/02/YYY Provider/Hosp Y ital 01/10/YYY Multiple YProviders 06/05/YYY Y DOB: 07/03/YYYY OCCURRENCE/TREATMENT Recommendations: This patient requires anticoagulation with Warfarin/Coumadin for 3 months for a VSD repair. He also had intermittent atrial fibrillation postoperatively. Target INR is 2.0 to 3.0. INR at the time of discharge is 2.6. He has been instructed to take Warfarin 2 mg orally daily. His postoperative echo shows a small residual VSD. QP/QS is essentially normal. Dr. Xxxx has identified this VSD to be “insignificant.” Patient is aware of symptoms to monitor for and to seek medical attention should these develop. He has a moderate right pleural effusion. This is residual post thoracentesis. The patient is asymptomatic at the time of his discharge. He is aware to monitor for signs of shortness of breath and to contact his Physician for assessment should this develop. He has a sternal incision which has dehisced at the distal portion. I have requested Vac/negative pressure wound therapy in the home setting. Should there be any concerns regarding the heating of this wound, the patient should followup with Dr. Xxxx. He is on Furosemide and Spironolactone for LV dysfunction. He is on Seroquel and should have intermittent ECG assessments for QT prolongation. I would request that the Family Physician provide the patient with a requisition for this as it was not provided Medication sheets: Aspirin – 81 mg Warfarin – 2 mg Multiple visits status post CABG and VSD repair: @ 01/10/YYYY: Patient complains of occasional chest pain, but denies SOB. @ 01/14/YYYY: Patient is recovering slowly and as expected. He is required to use a walker. He is unable to bend or stoop and requires assistance in dressing. He is unable to bath on his own and requires the assistance showering. @ 02/13/YYYY: Cardiac Rehabilitation: Patient is on Warfarin, will discontinue Aspirin. Will reassess LV function in 3 months. If EF still less than 30%, may be a candidate for Automatic Implanted Cardioverter Defibrillator (AICD). @ 03/18/YYYY: Patient denies chest pain and SOB. @ 06/05/YYYY: Patient denies chest pain, SOB and Paroxysmal Nocturnal Dyspnea (PND). Prescribed Nitro-Glycerin for CAD/CHF. *Reviewer's comment: Further medical records after 06/05/YYYY are not available to know the progress of the patient. 9 of 9 PDF REF 132 10, 147, 20, 11