* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download diarrheal diseases
Survey
Document related concepts
Transcript
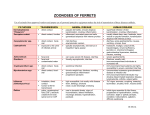
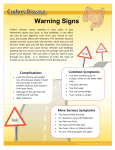
16/03/2015 DIARRHEAL DISEASES Dr. Syed Waleem Pasha Assistant Professor Dept. of Medicine • Three lecture series • 1st (16/3/2015) – Acute diarrhea – general & viral diarrhea • 2nd – Specific causes of diarrhea – bacterial • 3rd – Specific causes of diarrhea – bacterial and protozoal Objectives • Definition • Acute diarrhea • Causes – Infectious vs noninfectious • Epidemiology • Clinical features • Management – Fluid therapy • Brief note on chronic diarrhea Normal stool • Frequency • Consistency • Quantity • Frequency: 3/day to 1every third day • Consistency: porridge-like to hard and pellety • Quantity: <200 g/day Diarrhea - definition • Different for different people • Increased frequency • Loose or watery consistency • Increased quantity >200 g/day Duration of diarrhea • Acute diarrhea – <2 weeks • Chronic diarrhea – >4 weeks • Persistent diarrhea – 2-4 weeks Acute diarrhea • gastoenteritis vs food poisoning Causes • Infections – Toxin-mediated • Bacillus cereus • Staph enterotoxin • Clostridial spp enterotoxin – Infective • • • • • • • • Rotavirus Campylobacter Salmonella E.coli Shigella Clostridium difficlie Norovirus Cholera - Protozoal • Giardiasis • amebic dysentery • Cryptosporidium • Isospora • Microsporidium -Systemic illness • Sepsis • Meningococcal sepsis • Pneumonia • Malaria Causes - contd • Noninfectious – Gastrointestinal • Acute diverticulosis • IBD • Malignancy – Metabolic upset • • • • Ketosis VIP Carcinoid Uremia – Drugs and toxins • • • • • NSAIDs Cytotoxic agents Antibiotics Plant toxins Heavy metals Bloody diarrhea Infectious Noninfectious Campylobacter Diverticular diseases Shigella Rectal or colonic malignancy Non-typhoidal salmonella IBD EHEC Bleeding hemorrhoids EIEC Ischemic colitis Clostridium difficile intussusception Vibrio parahemolyticus Entameba histiolytica Epidemiology • • • • • Major cause of morbidity and mortality Infants and young children/ elderly MC cause: infection Fecal-oral transmission Fomites/ contaminated hands/ food/ water Clinico-pathological correlation • Diarrhea – – – – Volume: small vs large intestinal involvement Watery: secretory, toxin mediated Blood: invasive, cytotoxic Mucus • Vomiting: upper GI involvement • Fever: invasive • Incubation period Clinical history • • • • • • Suspect food Duration and frequency Blood in stool Abdominal pain and tenesmus Fever Incubation period – <18 hours: toxin – >5 days: protozoa/helminths Physical examination • Dehdration – Skin turgor/ mucous membranes – Blood pressure – Urine output • Severity Investigations • Stool examination – Blood – Leucocytes – Parasites – Culture • Blood counts • Electrolytes • Renal functions Treatment • Isolation • Principles: – Fluid replacement – Antimicrobial therapy – Adjunctive antidiarrheal therapy Fluid replacement • Most important and life saving • Fluid lost is isotonic • Absorption of electrolytes from intestine is active, needs energy • ORS • IV fluids • Amount of fluid – Replacement of established losses – Replacement of ongoing losses – Replacement of normal daily requirement ORS Fluid Na K Cl KCalories/l WHO 90 20 80 54 Dioralyte 60 20 60 71 Pepsi 6.5 0.8 - 400 Orange juice 0.2 49 - 400 Breast milk 22 36 28 670 Fluid replacement • Replacement of ongoing losses – Average: 200 ml of isotonic fluid/ stool – One sachet of ORS: 200 ml – One sachet per diarrhea stool is appropriate and effective • Replacement of normal daily requirement – Minimal daily requirement: 1-1.5 L • Replacement of established losses – Diarrhea, vomiting – ORS/ iv fluid Antimicrobial therapy • Shortens the illness by 1 day • Potential for antimicrobial resistance • Salmonella: increase the stool carriage time • EHEC: complicates HUS • Indications: – – – – Shigella dysentery Cholera Severe diarrhea Certain clinical condns Severity markers in AGE • Chronic conditions – Age>65 – Diabetes mellitus – Rheumatoid or other autoimmune diseases – Chronic renal disease – Valvular heart diseaase – Acquired or secondary immunodeficiency – Any internal prosthesis • Current drug therapy – – – – – Diuretic therapy ACE inhibitor therapy Corticosteroid therapy Cytotoxic therapy PPI/ H2 blockers •Current illness - Number of stools per 24 hours - Blood per rectum - Abdominal pain - Associated systemic toxicity Antimotility, antisecretory, antidiarrheal drugs • Not recommended or contraindicated in infective diarrhea Chronic diarrhea • More than 14 days • Most causes: noninfective • Infective causes: – Giardia lamblia – Strongyloidiasis – EPEC – HIV enteropathy – Intestinal flukes Viral diarrhea • Rotavirus – – – – – – Major cause in young children 30-50% of diarrheal admissions; 10-20% of diarrheal deaths Endemic in developing countries; Winter epidemics Person to person spread, hospital Incubation period of 48 hrs Infects enterocytes, decreases surface area for absorption and loss of enzymes on brush border –Watery diarrhea, vomiting, abdominal pain, fever – – – – Diagnosis: stool – enzyme immunoassay kits Self limiting Hydration Rotavirus vaccine; good protection but risk of intussusception Viral diarrhea • Norovirus (Norwalk agent) – – – – – Outbreaks related to food handlers Endemic gastroenteritis Feco-oral transmission If vomiting: aerosol spread Incubation period 48 hrs –Nausea+, predominant vomiting, little diarrhea • Calcivirus: Seasonal diarrhea • Astrovirus • Adenovirus serotype 40 &41 Thank you