* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Childhood Obesity Nottingham City Joint Strategic Needs
Survey
Document related concepts
Food choice wikipedia , lookup
Stunted growth wikipedia , lookup
Epidemiology of metabolic syndrome wikipedia , lookup
Human nutrition wikipedia , lookup
Thrifty gene hypothesis wikipedia , lookup
Abdominal obesity wikipedia , lookup
Diet-induced obesity model wikipedia , lookup
Obesity and the environment wikipedia , lookup
Childhood obesity wikipedia , lookup
Obesity in the Middle East and North Africa wikipedia , lookup
Transcript
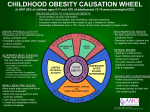
Childhood Obesity Nottingham City Joint Strategic Needs Assessment April 2010 Introduction Obesity results from an ‘energy imbalance’ - in adults, obesity occurs from taking in more energy than used. Getting the balance right in children is more complex as growth is only possible if energy intake (food and drink) exceeds energy output (resting metabolic rate and activity). If there is more than required for appropriate growth the excess energy will become excess fat. However, the underlying causes of this energy imbalance which result in weight gain are complex. Behavioural, psychological, social, cultural and environmental factors are thought to determine the increasing prevalence of obesity seen throughout the world. - - Obesity has been rising rapidly in children in England over the past 20 years (Ridler et al, 2009) the proportion of children classified as obese nearly doubling for children aged 4-5 years and increasing more than three fold for children aged 10-11 years (Ridler et al 2009). Nottingham has above average rates of child obesity when compared to the East Midlands and England and is ranked 127th out of 155 local NHS areas. Obese children are at increased risk of psychosocial problems, including reduced self-esteem and increased risk of depression and social isolation (Doak et al, 2006). Obese children are at risk of becoming obese adults reducing life expectancy by an average of 9 years through a greatly increased risk of heart disease, cancer, diabetes and high blood pressure (APHO, 2005). Adult obesity, physical activity, diet and nutrition and paediatric nutrition (see pregnancy and maternities) are considered elsewhere. Key issues and gaps - The prevention of childhood obesity requires a broad multifaceted partnership approach as outlined in the national strategy to tackle obesity Healthy Weight, Healthy Lives. Obesity is strongly associated with deprivation. In Nottingham where 81% of children fall in the first 3 deprivation deciles, this is a significant contributing factor. The family environment has a strong influence on a child’s development, their eating and activity habits, and predisposition to overweight. Nottingham has high rates of adult obesity increasing the risk of child obesity. Relatively higher rates of child obesity in the 10-11 years age group and falling rate in 4-5 years age group suggest that work in primary school age children should be one of the areas to focus attention locally. There is a low uptake of targeted weight management services relative to need within the care pathway. Current capacity of targeted weight management services does not meet the identified need for the 5 – 13 years age group. Data analysis is required to understand local obesity prevalence amongst children with learning disabilities and Looked After Children. Evidence of effectiveness of interventions to tackle obesity is lacking and more research is required to understand underlying causes. Interventions should therefore be rigorously evaluated. Page 1 of 16 Recommendations for consideration by commissioners - The partnership should continue to invest more resources in prevention in line with guidance and local targets to halt the rise in child obesity. - Work across the partnership to get better information on the prevalence of obesity amongst children with learning disabilities and Looked After Children. - Ensure early identification and prevention of obesity through the Healthy Child Programme by setting clear commissioning outcomes. - Implement the breastfeeding strategy and commission services to implement the UNICEF Baby Friendly Initiative. - Develop a child nutrition strategy and ensure integrated nutrition interventions through Children’s Centres, schools, and other community settings. - Support implementation of the Physical Activity, PE and Sport Strategy for Children and Young People to ensure more opportunities for physical activity, particularly family based interventions and access to facilities in deprived areas. - Develop a mechanism for recording progress towards the ambition of offering all children at least five hours of PE and sport every week. - Joint planning in the areas of the built environment, the natural environment, access to healthy food and transport. - Expand provision of targeted weight management interventions for the 5 – 13 year age group. - Develop and implement a communication strategy to ensure effective implementation of the Care Pathway to increase uptake of interventions. - Conduct a Health Equity Audit of the Go4It weight management service to assess equitable uptake of the service by disadvantaged and minority groups. - Continue to build the capability of the wider children’s workforce to ensure those working at a local level are clear about promoting the benefits of a healthy weight and feel confident in sensitively raising the issue with those who are overweight or obese. - Rigorously evaluate current interventions by including evaluation criteria from the Standard Evaluation Framework for Weight Management Interventions, (National Obesity Observatory, 2009) in contracts, and through research to inform future impact modelling and commissioning. - Conduct an assessment of new research around child obesity and re-evaluate the effectiveness of interventions in light of new evidence base. Page 2 of 16 1) Who’s at risk and why? - Obesity prevalence is influenced by age, gender, ethnicity and deprivation. - Prevalence of obesity almost doubles between the age of 4-5 years and 10-11 years (from 10.4% to 20% in boys and 8.8% to 16.6% in girls). Figure 1: Prevalence of child obesity, overweight, healthy weight and underweight, 2007/08 School Year Sex: Obese Overweight Healthy Weight Underweight Reception Boys Girls 10.4% 8.8% 13.6% 12.3% 74.5% 77.9% 1.5% 1.0% Year 6 Boys 20.0% 14.4% 64.5% 1.2% Girls 16.6% 14.2% 67.6% 1.6% Source: Ridler et al, 2009 - Levels of overweight and obesity are higher in children in deprived populations (Figure 2). In Nottingham where 81% of children fall in the first 3 deprivation deciles, this is a significant contributing factor. Figure 2: Prevalence of obesity in Year 6 children 2006/07 and 2007/08 by 2007 Index of Multiple Deprivation decile Source: Ridler et al, 2009 - The National Child Measurement Programme 2007/08 found that children in the Bangladeshi, Black African, Black Caribbean and Pakistani (except Year 6 girls) groups were significantly more likely to be classified obese than individuals from the White British ethnic group (Ridler et al, 2009). The above average proportion of people from African Caribbean and Pakistani communities within Nottingham is also therefore likely to contribute to Nottingham's overall higher rates of child obesity. - However it is important to note that the reasons for some of these differences are complex. Deprivation is a confounding variable for ethnicity and that there are differential degrees of deprivation between different ethnic groups, influencing the odds of being classified as overweight & obese. Differences in stature between ethnic groups can also account for some Nottingham City Joint Strategic Needs Assessment April 2010 Page 3 of 16 apparent ethnic differences. Controlling for height and development suggests that earlier findings in which children from Black African and Black Caribbean ethnic groups had the highest odds of being obese, were most likely to be due to physical characteristics related to ethnicity, in particular height. (Ridler et al, 2009) - Only 3 percent of overweight or obese children have parents who are not overweight or obese (Cross-Government Obesity Unit, 2008). The family environment has a strong influence on a child’s development, their eating and activity habits, and predisposition to overweight (Finn et al, 2002). Nottingham also has high rates of adult obesity increasing the risk of child obesity. - Children’s eating behaviours are influenced by the family food environment, including parental food preferences and beliefs; children’s food exposure; role modelling; media exposure and child/parent interactions around foods (Campbell et al, 2001). Similarly, children’s activity levels are strongly influenced by, for example, parental decisions on car use and walking, family television viewing habits, leisure time activities. - Inadequate diet (high intake of energy-dense foods) and low levels of physical activity increase the risk of obesity. The Health Survey for England, 2007 found that among girls aged 2 to 15 years, 21% of girls in the low physical activity group were classed as obese compared to 15% in the high activity group. - There are associations between certain geodemographic groups (groups defined by social, economic and lifestyle factors) and child obesity. However, owing to the lack of transparency in the way in which data is aggregated for these indicators it is uncertain how far these differences are explained by the factors already mentioned. Such data can be used however as a predictive tool to estimate postcode level risk. This is demonstrated by the ‘penetration map’ produced by Experian which shows the percentage of Super Output Area above the baseline level for Child Obesity. - Obesity is more common in people with learning disabilities than in the general population: It is estimated that 24% of children with learning disabilities are obese (Kerr et al, 2006). - There is very little information about the physical health of looked after children and young people despite evidence that they are at increased risk of ill health in adulthood. However according to the Caroline Walker Trust, looked after children may have poor access to adequate healthcare and health promotion information and highlight that their diets are a particular cause for concern. 2) The level of need in the population Published results from the National Child Measurement Programme undertaken during the 2008/9 academic year suggest that: - In Reception (aged 4-5 years), 26% of boys and 23% of girls were overweight or obese; - In Year 6 (aged 10-11 years) 38% of boys and 34% of girls were overweight or obese. Nottingham’s children have similar levels of obesity than the England average in Reception, although levels are higher than the England rate in Year 6 where 22.6% of those measured were obese. Data relating to 2008-09 is also available via he Information Centre website www.ic.nhs.uk Latest data presented in Figure 3 shows that rates appear to be rising in Year 6 boys and falling in reception year children. However, there are too few points to establish a trend and overlapping confidence intervals indicate that the differences are too small to be confident that differences are Nottingham City Joint Strategic Needs Assessment April 2010 Page 4 of 16 more than background random year on year change. 2006/7 and 2007/8 cohorts are not comparable groups of schools. That said, relatively higher rates of child obesity in the 10-11 years age group and falling rate in 4-5 years age group suggest that work in primary school age children should be one of the areas on which to focus attention locally. Figure 3: Proportion of children who are obese in Nottingham City schools reception year (aged 45 years) and year 6 pupils (aged 10-11 years) Source: National Child Measurement Programme The variability in rates at a smaller level is illustrated in Figure 4. Each point represents a school and there are widely varying rates between schools. However, almost all schools fall within the tramlines indicating a large proportion of the variation could be accounted for by small numbers and differences due to chance year on year variation. Figure 4: Funnel plot of percentage of Children Year 6 who are obese by school (2008/9 data) Source: Local Child Measurement Programme Data Nottingham City Joint Strategic Needs Assessment April 2010 Page 5 of 16 Benchmarking Nottingham against similar PCTs (ONS centres with industry B) shows Nottingham to be worse than average position, but similar to its peer group. The estimated expected percentage of children aged 10-11 years who are obese for Nottingham based on deprivation national rates is 21.45%. Table 1: Percentage of Obese Children Aged 10-11 Years: ONS Centres with Industry –B; 2008/9 Source: National Obesity Observatory e-Atlas AREA Sandwell Barking and Dagenham Wolverhampton Manchester Nottingham Birmingham East & North South Birmingham Leicester % Obese 24.59 24.22 23.52 22.64 22.56 20.75 19.79 17.78 Mosaic group F (people living in social housing with uncertain employment in deprived areas) has been identified as having the highest index score for child obesity in the City. The top ten wards with households in this group can be seen below: Top Ten Wards St Ann's Bridge Radford & Park Arboretum Bestwood Mapperley Dales Berridge Wollaton East & Lenton Abbey Bulwell % of Group F Households 60 51 30 24 18 18 16 14 13 12 Source: Nottingham City Council Children’s Services There are approximately 42,000 children aged 2 - 15 years registered with a Nottingham City GP. It is estimated (using the UK BMI 1990 BMI chart’s 91st and 98th centile cut offs and child measurement programme data 07/08) that approximately 6000 children/families would potentially benefit from targeted weight management services. Assuming that a minimum of 10% of these is motivated and committed to change if offered the opportunity, sufficient capacity for at least 600 specialist programme places per annum needs to be provided via an obesity pathway. Issues of Inequality Mapping illustrates the extent to which obese children are concentrated in the more deprived City areas. The wards with the highest proportion of obese children are: Aspley, Bilborough, Bulwell Forest, St Ann’s, Arboretum, Mapperley, Lenton Abbey and Clifton (Figure 5). In terms of service planning it is useful to examine which wards have the highest number of obese children. This shows a similar, yet slightly different picture with the highest numbers in: Aspley, Bilborough, Bulwell, Bulwell Forest, Bestwood, Berridge, Basford, St Ann’s, Dales and Clifton (Figure 6). These are areas where estimates of adult obesity are also relatively high. 26.7% of children in Nottingham belong to ethnic groups other than White British. Given the rates Nottingham City Joint Strategic Needs Assessment April 2010 Page 6 of 16 outlined above for different ethnic groups and the local ethnic mix about 1.75% of the overall rate in Year 6 children (21.95%) is attributable to ethnic mix. Further local analysis is being undertaken to understand how far the national picture is reflected locally. When socio-economic circumstances and parental education is taken into account, ethnic differences may not be great. However, cultural issues are important for management and prevention. Figure 5: Number of obese children: 2006-2009 Figure 6: Proportion of obese children: 2006-2009 Source: Local Child Measurement Programme Data, NHS Nottingham City Notable changes in need since JSNA April 09 Between the academic year 07-08 and 08-09 there has been little overall difference in the percentage of overweight and obese children in both the Reception and Year 6 age groups. In Reception the percentage has decreased from 26% to 25% and in Year 6 the percentage has remained at 36%. The percentage of obese children in Reception has decreased from 13% to 10% and only a small increase (less than 1%) occurred in Year 6. Whilst year-on-year variation makes it difficult to assess the significance of the apparent slowing of the rise in child obesity, Nottingham still seems likely to meet its aspiration to halt the rise in child obesity by 2010 (albeit at a slightly higher proportion than the agreed targets). NCMP data from 2006-2009 has been combined which gives a more robust analysis of areas of the City with the highest rates and number of obese children. Since the JSNA 2009, some Nottingham City Joint Strategic Needs Assessment April 2010 Page 7 of 16 additional areas (Clifton, St Ann’s and Dales) have been identified as areas that would benefit from additional services. 3) Current services in relation to need A Strategic Obesity Group is in place to drive the strategy and action plan to support both the prevention and management of obesity in line with Healthy Weight, Healthy Lives and NICE guidance. Key elements of the strategy are: A jointly developed plan and strategy for child obesity for the city of Nottingham with clear indicators of success to support management of programme implementation by a strategic partnership group. A clear understanding of the size of the problem through a well conducted child measurement program and analysis informing the Joint Strategic Needs Assessment. A child nutrition programme to promote breast-feeding, uptake of Healthy Start and healthy diet delivered through children's centres and schools through the School Food Action Group, Healthy Schools and Healthy Children’s Centres work. Promotion of physical activity as part of the schools' core offer to deliver the national curriculum, Healthy Schools, extended schools, the Nottingham City Council Sport and Physical Activity Strategy, the Nottingham Play Strategy, the Physical Activity, PE and Sport Strategy for Children and Young people and implementation of school travel plans and initiatives such as Active Schools and Active Families. Environmental approaches to improve accessibility and safety of recreational areas through the Breathing Space Strategy, Sport and Physical Activity Strategy, Nottingham Transport Plan, the Play Strategy and improving access to healthy fruit and vegetables through the city and county Food Initiatives Group. A care pathway to route children with weight problems to targeted and family-based initiatives developed in partnership. Increased capacity and capability of the workforce with increased investment, the development of support worker roles and provision of staff training. Use of Change 4 Life social marketing research to promote effectiveness of interventions and improve reach to target groups Evaluation of key interventions to refine delivery and improve commissioning The strategic group co-ordinates action required to meet the childhood obesity Local Area Agreement (LAA) target. The Local Strategic Partnership is working to meet both the NI 56 (child obesity) and NI57 (participation in PE and sport) LAA targets. Nottingham City Joint Strategic Needs Assessment April 2010 Page 8 of 16 Preventing overweight and obesity: Universal Approaches Much of the activity that will help to reduce child obesity at a population level is inherent within current general provision and therefore not readily identifiable. However listed below are some key interventions which contribute to the prevention of overweight and obesity: The overarching aim of the Breastfeeding Strategy is to improve the health Breastfeeding and survival of infants and young children by promoting the initiation and Strategy continuation of breastfeeding. The early identification and prevention of obesity is a key priority in the HCP. Healthy Child All families are given information and advice around breastfeeding, healthy Programme (HCP) weaning, healthy eating and active play. Healthy Start is open to pregnant women and families with children under 4. Healthy Start Vouchers are provided to exchange for fresh fruit and vegetables as well as milk and infant formula milk. The group aims to promote and facilitate a whole school approach to healthy School Food Action eating, the prevention of childhood obesity and the promotion of good Group nutrition. City Smiles consists of oral health messages to improve oral hygiene and Oral Health healthy eating practices. Children’s Centres are supported to achieve best practice criteria within the 4 Healthy Children’s core themes of Personal, Social and Emotional Development, Healthy Centres Eating, Physical Activity and Play and Emotional Health & Wellbeing. This is an intervention which provides family physical activity sessions in city Active Families leisure centres and community settings offering a variety of activities suitable for the whole family School travel plans are a key aspect of the Sustainable School Travel School Travel Plans Strategy and aim to increase the number of pupils walking to school. An intervention delivered in primary schools to promote physical activity, Active Schools consisting of football and indoor rowing coaching, teacher mentoring and education in healthy lifestyles. Schools are supported to achieve best practice criteria within the 4 core Healthy Schools themes of PSHE, Healthy Eating, Physical Activity and Emotional Health and Wellbeing in order to achieve National Healthy School Status. A strategic framework to enable “All children in the City of Nottingham to Nottingham Play access a wide range of appropriate, freely chosen, self directed play Strategy opportunities”. The strategy seeks to inspire all children and young people to lead more Physical Activity, PE active, healthier and successful lives, through lifelong participation and & Sport Strategy for achievement in physical activity, physical education and sport. Children and Young People A local stakeholder group has been formed which coordinates local activity to Change4Life increase the impact and relevance of the Change4Life campaign to front line staff and families. The Strategy sets out proposals for the strengthening of local community Breathing Spaces engagement in the management and improvement of open and green space Strategy to achieve better quality, sustainable open and green spaces that are accessible and inviting to use. This piece of work is exploring the possibility of restricting the siting of new Planning fast food / hot takeaways premises near schools and other places where children and young people congregate. Nottingham City Joint Strategic Needs Assessment April 2010 Page 9 of 16 Interventions/services for children and young people who are overweight and obese (using 91st & 98th centile cut offs) Age Estimat Estimated Services in relation to need group ed number 2-4 years 1680 (1200 overweight & 480 obese) number eligible for intervention 1 120 eligible for Level 1 intervention (see care pathway) *100 eligible for Level 2 intervention *This includes obese children plus a proportion of overweight children who have had unsuccessful Level 1 intervention 5 - 13 years 5900 (4100 overweight & 1800 obese) 410 eligible for Level 1 intervention *380 eligible for Level 2 intervention *This includes obese children plus a proportion of overweight children who have had unsuccessful Level 1 intervention) Healthy Child Programme (Level 1) Families of overweight children receive brief intervention and intensive support including signposting to local healthy living opportunities by health visitors, Family Nurse Practitioners, GPs and practice nurses. There is capacity for all eligible families. Active Families (Level 2) An intervention which provides family physical activity sessions in city leisure centres and community settings. Families with an overweight or obese child aged 2-4yrs can be referred by a health professional and receive 10 free Active Families sessions. Brief intervention around healthy eating is given in addition to the referral. There is capacity for all eligible families. Brief Intervention (Level 1) Overweight children/families receive brief intervention and intensive support including signposting to local health living opportunities by school nurses, GPs and practice nurses. There is capacity for all eligible families through the School Nursing Service (Healthy Child Programme, 5-19 years). Go4It! (Level 2) Go4It is an evidence based targeted weight management service which encourages children and families to establish and maintain healthy lifestyles by promoting and educating them in skills and knowledge around nutrition, physical activity and behaviour change. Service consists of 24 sessions over a 12 week period. Running at 3 sites (in areas with high child obesity rates). There is capacity for 135 children/families per year. Academic Year 2005-2006 2006-2007 2007-2008 2008-2009 Total No. attending 46 82 40 74 Of the 74 who attended Go4It in 2008/09, 16% children attending had a disability, 42% were from BME communities and Nottingham City Joint Strategic Needs Assessment April 2010 Page 10 of 16 14 15 years 1800 (1200 overweight & 600 obese) 120 eligible for Level 1 intervention *120 eligible for Level 2 intervention *This includes obese children plus a proportion of overweight children who have had unsuccessful Level 1 intervention) Brief Intervention (Level 1) Overweight young people receive brief intervention and intensive support including signposting to local health living opportunities by school nurses, GPs and practice nurses. There is capacity for all eligible families through the School Nursing Service (Healthy Child Programme, 5 – 19 years). Slimming World (Level 2) Slimming World has been commissioned to provide weight management services for adults in Nottingham City and this extends to young people aged 14-15 who will be offered the children’s package. Children must be accompanied by their parent / guardian. A voucher is given to the child/parent who attends the group in the same manner as a paying customer. This consists of a 12- week local Slimming World group. 59 of the city’s 62 GP practices have signed up to the scheme. Nine young people have been referred and accessed the service since implementation in May 2009 until December 2009, all aged between 17-19 years. There is capacity for all eligible young people. In summary, we estimate we need sufficient capacity for approximately 600 children/families to receive a targeted weight management service. Current capacity is for 355 families. PCT funding will increase in 2010 to provide Go4It at two additional sites which will increase capacity to 445. Work is in progress to ensure children from priority groups are engaged in the programme. Go 4 It! is currently operating at Harvey Hadden Sports Complex, Bilborough, The Vine Community Centre, Bobbersmill/Radford, and Southglade Leisure Centre, Bestwood. The service will be expanded into Clifton and Sneinton in 2010 to reflect the higher need of the population in these areas. Specialist Services Overweight children who have co-morbidities or complex needs are referred for Paediatrician assessment and management. Present services meet demand but further work may be required to ensure appropriate uptake and referral is taking place in the future. Notable changes since JSNA April 09 - Implementation of Active Schools intervention. - Obesity care pathway for children aged 2-16 years has been developed as well as supporting documentation/guidance and an adapted version of the pathway for the wider children’s workforce is in development. - A Directory of Healthy Living Opportunities for Children has been developed to support signposting of overweight children to local physical activity and healthy eating opportunities. - Development of a Physical Activity, PE and Sport Strategy for Children and Young People. - Development and implementation of Active Families intervention. - National Child Measurement Programme - proactive feedback of results was piloted in two schools, where parents of overweight and obese children were contacted by school nurses and offered a one- one consultation. A larger pilot will take place in 2010 including a robust evaluation of the impact of this approach. Nottingham City Joint Strategic Needs Assessment April 2010 Page 11 of 16 - In partnership with NHS Nottinghamshire County the recruitment of an infant feeding coordinator to work towards achieving UNICEF Baby Friendly accreditation across local maternity services is currently being processed. - Department of Health funding has been awarded to recruit a breastfeeding coordinator to implement Baby Friendly across community health services. 4) Projected service use and outcomes in 3-5 years and 5-10 years In 2007/08, 21.9% of Year 6 children in Nottingham were obese. As the levels of obesity are predicted to continue to increase in the near future, halting the year on year rise is a challenging, complex and long term issue. Too few data points (4 years) are known to reliably set trends. The projected local trend (Figure 1) is therefore based on the current national trend, which estimates child obesity at both Reception and Year 6 rising at a yearly rate of 0.5% points (Department of Health, 2008). Figure 1: Rates, trends and targets for child obesity in Nottingham % of children who are obese 30 25 20 15 10 5 0 Actual Prevalence (Yr 6) 2005/06 2006/07 2007/08 2008/09 20.2 20.1 21.9 22.6 21 Projected Trend (Yr 6) LAA/Local Operational Plan Target (Yr 6) England Rate (Yr 6 ) Actual Prevalence (Reception) 12.5 2010/11 2011/12 2012/13 21.5 22.0 22.5 23.0 23.5 20 20 20 15.5 16 17.5 18.3 18.3 12.5 12.8 10 13.5 14 14.5 15 12 12 12 Projected Trend (Reception) LAA/Local Operational Plan Target (Reception) England Rate (Reception) 2009/10 9.9 9.6 9.6 However, the National Heart Forum (Brown et al, 2009) found evidence that the rate of increase in childhood obesity may be starting to slow. Its figures suggest that by 2020 the proportion of boys aged 2-11 who will be overweight or obese will be 30% - not 42% as previously predicted. For girls of the same age the revised prediction is now 27% - down from 48%. The revised predictions also indicate a big drop in the number of overweight and obese young people aged 12-19. The National Heart Forum based its latest predictions on data collected for the Health Survey for England between 2000 and 2007. Previous estimates were based on data collected for the same survey between 1993 and 2004. Based on population projections, these revised predictions suggest that there will be approximately 5935 obese 2-19 year olds living in Nottingham by 2020. Nottingham City Joint Strategic Needs Assessment April 2010 Page 12 of 16 Nottingham 2020 Population Projection Obesity Rate based on National Health Forum Projections Projected Number Obese in 2020 2- 11 year population 32,560 13% 4233 12-19 year population 28,360 6% 1702 TOTAL 5935 These projections however, are based on national modelling so it can be assumed that this is an underrepresentation of the projected number of obese children in Nottingham due to high levels of deprivation in the city. They also do not take account of the effect of interventions to reduce child obesity. See page 1 of the Childhood Obesity factsheet for more information 5) Evidence of what works National Institute for Health and Clinical Excellence. Obesity: the prevention, identification, assessment and management of overweight and obesity in adults and children. 2006. Department of Health (2008) Healthy Weight, Healthy Lives - A Cross Government Strategy for England Department of Health (2008) Healthy Weight Healthy Lives – a Toolkit for developing local strategies. Foresight Report (2007) Tackling Obesities: Future Choices – Project Report It is very difficult to estimate cost effectiveness as effect of interventions are usually indirectly related to outcome and are difficult to measure over long-term scales. However, given the high costs of managing obesity and related health conditions and the high and rising prevalence it is likely that the return on investment is high. At present a small fraction of expenditure is on prevention when compared with dealing with consequences of obesity. 6) User Views Evaluation of Go 4 It! and Active Schools shows positive user feedback and further research of the outcomes of the programme are planned. The work carried out by the PCT as a part of Our NHS Our Future highlights childhood obesity as a priority issue as expressed via the public engagement event forums. Partners are working collaboratively to take account of local views and address concerns. Further work is planned to engage school governing bodies with the results of the Child Measurement Programme. 7) Equality Impact Assessments Issues raised by Equality Impact Assessment National and local data suggests a higher rate of obesity amongst children from Black and Minority Ethnic groups, particularly Black African, Black Caribbean and Asian groups. In 2008/09, 42% of families accessing the Go 4 It! programme were from Black and Minority Ethnic Groups. An Equality Impact Assessment of the Child Obesity Strategy will be conducted in 2010. Nottingham City Joint Strategic Needs Assessment April 2010 Page 13 of 16 8) Unmet needs and service gaps - There is a short-term need to continue to expand provision of universal and targeted interventions in order to reduce long-term need for health services to tackle the complications of child and adult obesity. - Services are located to provide access to disadvantaged communities but uptake on basis of need needs to be confirmed. - Some schools are reluctant to participate in the child measurement programme. This is being addressed by the development of a ‘school health forum’ in conjunction with head teachers, schools and the Local Authority in the 2009/10 school year - Go4 It! programme is established in 3 areas but at present uptake is low and the minimum estimated required capacity is not provided. - Opportunities for physical activity, particularly for families and young women who are prenatal could be increased. - There is a need to increase capacity and capability ensuring all staff working with children and families are trained to sensitively raise the issue of weight and offer appropriate support in line with the care pathway. - Evidence of effectiveness of interventions to tackle obesity is lacking and more research is required to understand underlying causes and what works. 9) Recommendations for consideration by commissioners - The partnership should continue to invest more resources in prevention in line with guidance and local targets to halt the rise in child obesity. - Work across the partnership to get better information on the prevalence of obesity amongst children with learning disabilities and Looked After Children. - Ensure early identification and prevention of obesity through the Healthy Child Programme by setting clear commissioning outcomes. - Implement the breastfeeding strategy and commission services to implement the UNICEF Baby Friendly Initiative. - Develop a child nutrition strategy and ensure integrated nutrition interventions through Children’s Centres, schools, and other community settings. - Support implementation of the Physical Activity, PE and Sport Strategy for Children and Young People to ensure more opportunities for physical activity, particularly family based interventions and access to facilities in deprived areas. - Develop a mechanism for recording progress towards the ambition of offering all children at least five hours of PE and sport every week. - Joint planning in the areas of the built environment, the natural environment, access to healthy food and transport. - Expand provision of targeted weight management interventions for the 5 – 13 year age group. - Develop and implement a communication strategy to ensure effective implementation of the Care Pathway to increase uptake of interventions. - Conduct a Health Equity Audit of the Go4It weight management service to assess equitable uptake of the service by disadvantaged and minority groups. - Continue to build the capability of the wider children’s workforce to ensure those working at a local level are clear about promoting the benefits of a healthy weight and feel confident in sensitively raising the issue with those who are overweight or obese. - Rigorously evaluate current interventions by including evaluation criteria from the Standard Evaluation Framework for Weight Management Interventions, (National Obesity Observatory, 2009) in contracts, and through research to inform future impact modelling and commissioning. Nottingham City Joint Strategic Needs Assessment April 2010 Page 14 of 16 - Conduct an assessment of new research around child obesity and re-evaluate the effectiveness of interventions in light of new evidence base. Notable changes since JSNA April 09 The following recommendations have been removed because they have been, or are in the process of being implemented: - Further development of the child obesity strategy should make use of data in gaining engagement of independent agencies such as schools to implement interventions outlined in the Children and Young People’s Plan (CYPP). - Multiple approaches (as outlined in the CYPP) are required and therefore there should be a greater focus on local partnership action through a City-based child obesity working group that is a part of the local strategic partnership structure. - Family based interventions need to be developed alongside the adult obesity strategy to tackle the intergenerational aspect of obesity 10) Further needs assessment required - Bring together data on a range of obesity indicators and provide at a locality level where possible and share with all partners. - Carry out further data collation and analysis to understand the trends and patterns of child obesity and also to understand the uptake of services in relation to need with a particular focus on children with learning disabilities and Looked After Children. - Identify reasons for high drop out rates and non attendance to the Go4It programme. - Conduct an analysis of the child obesity data and the PE, school sports and club links survey (PESSCL) data by school, and provide to schools to inform commissioning decisions. Key contacts Dr. Peter Cansfield, Consultant in Public Health, NHS Nottingham City , [email protected] Sarah Diggle, Public Health Development Manager, NHS Nottingham City, [email protected] Susan Twemlow, Head of Service Commissioning Children and Families, Nottingham City Council, [email protected] References: APHO (2005). Indications of Public Health in the English Regions 3: Lifestyle and its impact on health. http://www.apho.org.uk/apho/publications/sepho_CMO3Lifestyle_220205.pdf Birch L, Davison K. (2001). Family environmental factors influencing the developing behavioural controls of food intake and childhood overweight. Paediatric Clinics of North America , 48:893–907 Brown M., Marsh T., McPherson K., Byatt T. (2009). Obesity: Recent Trends in Children Aged 2-11y and 12-19y. Analysis from the Health Survey for England 1993 – 2007. National Heart Forum Campbell K, Crawford D (2001). Family food environments as determinants of preschool aged children’s eating behaviours: implications for obesity prevention policy. A review. Australian Journal of Nutrition and Dietetic, 58:19–25. Caroline Walker Trust (2001). Eating well for looked after children: nutritional and practical guidelines. London: Caroline Walker Trust. Nottingham City Joint Strategic Needs Assessment April 2010 Page 15 of 16 Cross-Government Obesity Unit (2008) Healthy Weight, Healthy Lives: A Cross-Government Strategy for England. London: DH/DCSF (available at www.dh.gov.uk/en/ Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_082378). Department of Health (2008). How to set and Monitor Goals for Child Obesity: Guidance for PCTs and Local Authorities. Doak, et al. The prevention of overweight and obesity in children and adolescents. Obesity Reviews 2006; 7:111-136. Finn K, Johannsen N, Specker B (2002). Factors associated with physical activity in preschool children. Journal of Paediatrics, 140:81–5. Kerr MR, Felice D (2006). Paper based on data also included in an unpublished study for the Disability Rights Commission: Equal Treatment – closing the gap. London: Disability Rights Commission. McPherson K, Marsh T, Brown M (2007) Foresight Tackling Obesity:-Future Choices- Modelling Future Trends in Obesity and their impact on Health. Government Office for Science National Institute for Health and Clinical Excellence (2006), Obesity: the prevention, identification, assessment and management of overweight and obesity in adults and children. Ridler C, Townsend N, Dinsdale H, Mulhall C, Rutter H (2009); National Child Measurement Programme: Detailed Analysis of the 2007/08 National Dataset; HM Gov London Nottingham City Joint Strategic Needs Assessment April 2010 Page 16 of 16