* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download DOC - World bank documents
Survey
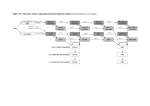
Document related concepts
Transcript
PROJECT INFORMATION DOCUMENT (PID) CONCEPT STAGE Project Name Region Sector Project ID Borrower(s) Implementing Agency Environment Category Date PID Prepared Estimated Date of Appraisal Authorization Estimated Date of Board Approval Report No.: 46673 Africa Regional Health and TB Support Project AFRICA Health (100%) P111556 REGIONAL PROJECT SEVERAL BORROWERS Ministries of Health in participating countries [ ] A [X ] B [] C [ ] FI [ ] TBD (to be determined) November 18, 2008 June 15, 2009 September 3, 2009 1. Key development issues and rationale for Bank involvement A major public health problem Sub-Saharan Africa has the highest rates of tuberculosis and the worst treatment outcomes, with the continent contributing significantly to the global rise in TB. While other regions have shown a steady decline in the TB burden, the numbers of new cases and mortality rates have been on the rise in Africa since 1990, fuelled by the HIV/AIDS epidemic. Of the 22 high burden countries worldwide nine are in Africa (DR Congo, Ethiopia, Kenya, Mozambique, Nigeria, South Africa, Tanzania, Uganda and Zimbabwe). About a dozen countries on the continent are afflicted with the highest incidence rates in the world, including Swaziland, Lesotho, Botswana, Zambia, and Malawi. Tuberculosis is a preventable and treatable infectious disease that hits hardest working age adults, and imposes heavy costs, particularly among the poor. A dual epidemic TB control in Africa is distinguished from other continents by the high prevalence of TB/HIV co-infection, with each disease accelerating the other’s progression. Tuberculosis is the most common opportunistic infection of people living with HIV/AIDS who have compromised immune systems and the leading killer of HIV infected patients. While the lifetime risk of developing active tuberculosis for a HIV negative person is 5-10 percent, an HIV positive patient has an annual risk of 5-10 percent to develop TB. For infected individuals there is a need for rapid diagnosis, as infectiousness and risk of TB transmission is most serious before people are placed on treatment. The HIV epidemic poses new challenges to the traditional approach of combating TB based on the DOTS strategy. While the DOTS strategy is essential it is not sufficient. The DOTS (Directly Observed Therapy Short-Course) strategy for TB control-- comprising of diagnosis by sputum-smear microscopy, short course chemotherapy with rifampicin and isoniazid, and systematic monitoring of each patient to evaluate outcomes-- has worked well historically in countries with low rates of HIV infection. Experience from Africa suggests that even well managed TB programs can not easily control the rise in tuberculosis in high HIV prevalence settings. Countries with high rates of HIV infection and drug resistance need to adopt a DOTS- plus approach, including greater attention to TB/HIV integrated care and greater focus on appropriate diagnostics for early identification and treatment of co-infected patients and those suffering from drug resistant strains. An emerging drug resistance problem Multi-drug resistant tuberculosis in Southern Africa is becoming an increasing threat to the health and development gains in the region. Multi-drug resistance stems from weak TB control systems, unstable supply of quality first-line drugs, and poor program management. Drugs for treatment of resistant forms of tuberculosis have higher levels of toxicity, case fatality, and treatment failure and are much more expensive. In high HIV settings the emergence of multi-drug resistant forms of TB is having devastating effects, threatening to compromise the gains made in HIV/AIDS investments. Recent experience has shown that people living with HIV/AIDS are not only more susceptible to TB but those on antiretroviral therapy (ART) are no more protected from death due to extensively drug resistant TB than those who are not on ART. The emergence of drug resistant strains underscores the importance of strengthening the quality of basic DOTS programs, as well as introducing appropriate technology for early and efficient diagnosis and treatment of those coinfected with TB and HIV and to strengthen surveillance efforts to respond more efficiently to future epidemics. Health systems challenges The effective response for disease detection and monitoring remains constrained by systemic health systems weaknesses. The barriers that limit laboratory capacity are largely those which limit health service provision in general, namely human resources, financing, procurement and supply chain management, regulatory environment, and information systems. Each of these systemic constraints needs to be strengthened, thereby reinforcing regional capacity for diagnosis and management of multiple diseases. Laboratories are among the weakest aspects of health systems, hindering patient management and disease surveillance. Allocation of resources for diagnostic laboratory testing has not been a priority for either governments or donors. The gross underfunding of laboratories has resulted in unreliable and inaccurate testing and misdiagnosis, which in turn leads to higher costs and compromised patient care. Building laboratory capacity to provide rapid, accurate, affordable, and reliable diagnostic tests will enable health care workers to deliver more effective treatment, enhance efficiency in use of resources, and improve quality of care. It is broadly recognized that lack of diagnostic capacity is a crucial barrier preventing an effective response to the challenge of HIV associated tuberculosis as well as multi-drug resistant forms. The accuracy of sputum smear microscopy, the standard method for diagnosing TB, is reduced by the presence of HIV infection. Most countries in the Africa region have limited or no capacity to diagnose HIV related tuberculosis which requires diagnostic techniques (e.g. liquid culture) that are more efficacious but also more costly, and more complex. The majority of countries in the region do not have capacity to do drug-sensitivity testing (DST) and to conduct drug resistance surveys. National laboratories are often in need of physical upgrading, as demand for their services has outstripped capacities, and as new technologies and diagnostics require physical modifications, such as improvements in bio-safety and infection control standards. In spite of the increasingly regional nature of TB in Africa, the region has virtually no diagnostic or surveillance capacity at the supranational level. Currently, there is only one supranational reference laboratory in South Africa which is stretched beyond capacity, supporting drug resistance tuberculosis surveillance activities and not able to expand routine diagnostic services, external laboratory quality assurance, and regional training. There is a huge need to establish additional supranational reference laboratories to boost diagnostic and quality assurance functions in the region. Human resources are another major weakness. Human resources capacity at national reference laboratories is a particularly serious issue, as numbers are far below critical mass, there is limited training, inadequate pay, lack of structured career paths, and non-recognition of the importance of diagnostic services. Given the highly infectious nature of TB, particular measures need to be introduced to protect health workers and laboratory technicians from being infected and priority treatment needs to be provided for staff that is infected. Rationale for Bank Involvement Tuberculosis prevention and control is a regional and global public good, with high positive externalities, as benefits accrue to non infected individuals within and across countries. The risks of transmitting drug resistant forms of TB, particularly in Southern Africa, are enormous and individual countries do not always have the resources and incentives to make the necessary investments which would have spillover effects for other countries. Investments in lab strengthening have potential spillover effects for other diseases, as upgraded labs will ultimately benefit other patients. The proposed project is consistent with the Bank’s institutional focus on global public goods and with the 2007 Bank Health Nutrition and Population Strategy which focuses on health systems strengthening. Tuberculosis Control in Sub-Saharan Africa Why TB? High burden of TB; highest levels of infection; disproportionate share of global burden Rise in drug resistant TB, which poses major public health risks regionally and globally Preventable and treatable disease associated with poverty which hits primarily working-age adults High expected rate of return, highly cost-effective, strong public good nature of TB control Why Labs? Gross underfunding has resulted in misdiagnosis, higher costs, and compromised patient care Accuracy of standard method for diagnosing TB is reduced by presence of HIV infection Virtually no capacity in the region to diagnose and treat drug-resistant forms of TB Introduction of modern diagnostics will result in reduced diagnostic delays and improved quality of care Why a Regional Approach? Potential to reap economies of scale, lowering costs, and achieving higher quality diagnostic services Dearth of capacity at regional level to deal with a regional public good Inherent market failures which imply that services may not otherwise be provided by individual countries Why Bank support? Investments in TB are in line with the institutional commitment to global public goods Comparative advantage to address systemic health systems issues hindering TB programs Funding gaps persist and key role for the Bank as donor of last resort Bank’s traditional comparative advantages (analytic capacity, convening power) can be brought to bear 2. Proposed objective(s) The project development objective is to improve access, quality, and efficiency of TB diagnostic services using an integrated approach to laboratory strengthening. The specific objectives would be to: (i) establish additional Supranational Reference Laboratories to provide quality assurance, training, and capacity building; (ii) introduce modern techniques for diagnosis of HIV related TB, and increase capacity for drug resistance diagnosis and surveillance in a group of national reference and public health laboratories in priority countries; and (iii) develop and test alternative service delivery models to promote private sector involvement. The project would also facilitate learning and knowledge sharing across the network of participating laboratories and countries. 3. Preliminary description Country Selection All countries will be eligible to participate. Selection and prioritization will be based on several criteria: (i) epidemiological situation (i.e. burden of TB, HIV, and drug resistant TB; (ii) existing laboratory capacity to address HIV related and drug resistance tuberculosis, (iii) presence of other partners and projected funding gaps; and (iv) country interest to participate in this regional operation and willingness to contribute one-third to the total cost from the respective IDA country allocations. Project Components The proposed US$140 Million Regional Health and TB Support Project includes three components. Project components are described below. Supranational Laboratory Capacity Enhancement (US$30 million) This component will finance the establishment of regional capacity to: (i) conduct external quality assessments of national reference laboratories, (ii) provide training and capacity building across the region to develop a new cadre of laboratory experts, and (iii) provide a regional forum for knowledge sharing and research on new diagnostics. This would be accomplished by financing the upgrading, rehabilitation, and equipping of regional laboratories with modern diagnostics, ensuring the availability of well trained personnel, assisting with operational and logistical costs, and providing funds for conducting research and organizing knowledge sharing workshops. Operational research activities will be financed to document and learn from this regional lab initiative. The project would fund operational research on suitability and cost effectiveness of new diagnostic technologies in resource constrained settings, and share emerging good practices. Laboratories targeted for becoming supranational facilities will be selected in consultation with countries and through the Global Lab Initiative with support of technical partners. The facilities would be accredited to function at the regional level, ensuring equity in geographical access and coverage. National Reference and Public Health Laboratory Network Strengthening (US$90 million) This component would support the modernization of national reference laboratories with an initial focus on tuberculosis control. The goal is to assist national reference and other public health laboratories to rapidly detect drug resistance, strengthen supervision and quality assurance, boost the volume, quality and efficiency of diagnostic services, and provide outreach and support services to district and rural clinical laboratories. This would be done by upgrading and expanding existing national laboratories; ensuring biosafety and appropriate infection control; introducing modern diagnostics; supporting drug susceptibility testing; providing logistical means to transport infectious samples promptly and safely; expanding training in laboratory methods, quality management, and biosafety; and providing technical support to build and sustain capacity. The project would also support the development of a Laboratory Quality Management System which would address systemic barriers that limit laboratory capacity. The Quality Management System will extend out of the National Reference Laboratory to build and monitor upstream (supranational) and downstream (regional and service level) linkages. The possibility of leveraging World Bank funds to mobilize financial support for drugs and diagnostics from UNITAID would be explored during project preparation. Public Private Partnerships in TB Control (US$20 million) This component aims to support the financing of partnerships with the private sector and the testing of alternative service delivery models to engage the private sector in achieving public health goals in TB control. While recognizing that some TB related services (e.g. control of disease vectors) are pure public goods because of the inherent market failures, other services (e.g. laboratory testing) may be provided by both the public and private sectors. Building on the significant private sector involvement in health in Sub-Saharan Africa the project would support different ways to harness the private sector in improving efficiency, promoting innovation, and ensuring sustainability. To this end, the project would finance a combination of the following activities, depending on individual country interests and circumstances: Knowledge Stocktaking, including the following activities: (i) a study of private sector involvement in laboratory services (with a particular focus on TB control) globally with applications for sub-Saharan Africa; (ii) consultations with policy makers and partners to discuss findings and their relevance to the regional initiative to bolster laboratory and diagnostic services and to reach agreement on the main elements of a public private partnership for strengthening laboratory services and TB control. Public-Private Partnerships: The project would fund contracts with private laboratories using a public/partnership model, with possible support from IFC. The partnerships may also be coupled with IFC loans to interested private sector groups who may wish to collaborate on a larger scale. The number and types of partnerships to be funded would depend on the findings of the study mentioned above, so maximum flexibility would need to be maintained. Operational Research: The project would support operational research to test alternative public private partnerships, such as management contracts, leases, structured leases or full concessions, for delivering these services in the most cost effective manner. Framework for Scale-up The preparation and design of the proposed operation will be done in close collaboration with key partners involved in strengthening diagnostics in sub-Saharan Africa. This will minimize the risk of duplication and ensure that participating countries take advantage on a priority basis of the grant financing available from the Global Fund, bilateral agencies, and foundations. This coordinated approach will ensure that the Bank’s comparative advantage in providing flexible financing will be coupled with the technical know-how of the Stop TB partnership, and top notch technical expertise, including from the network of laboratory specialists established under the Global Laboratory Initiative with its secretariat in the Stop TB Department of WHO, which is our key partner in this initiative. The Global Laboratory Initiative network aims to expand access to diagnostic services through associated laboratory infrastructure, financial, and human resources are mobilized. GLI provides a good framework for this operation with its mandate to work on: (i) global policy guidance on appropriate laboratory technology and best practices; (ii) laboratory advocacy and resource mobilization; (iii) laboratory capacity development and coordination; (iii) interface design with other laboratory networks to ensure appropriate integration; (iv) standardized laboratory quality assurance; (v) coordination of technical assistance; and (vi) effective knowledge sharing. 4. Safeguard policies that might apply The IDA-funded operation is expected to be classified as category B 5. Tentative financing Source: BORROWER/RECIPIENT International Development Association (IDA) Total 6. Contact point Contact: Miriam Schneidman Title: Sr Health Spec. Tel: (202) 473-9391 Fax: Email: [email protected] 140 140