* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cranial Nerve X
Survey
Document related concepts
Transcript
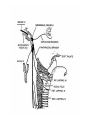
Cranial Nerve X - Vagus • "Vagus" is from the Latin meaning wandering. This is a fitting name as the nerve wanders from the brainstem to the splenic flexure of the colon. The vagus nerve consists of five components with distinct functions Somatic motor • Supplies the voluntary muscles of the pharynx and most of the larynx Visceral motor • Parasympathetic innervation of the smooth muscle and glands of the pharynx, larynx, and viscera of the thorax and abdomen. Visceral sensory • Provides visceral sensory information from the larynx, esophagus, trachea, and abdominal and thoracic viscera, as well as the stretch receptors of the aortic arch and chemoreceptors of the aortic bodies General sensory (general somatic afferent) • Provides general sensory information from the skin of the back of the ear and external auditory meatus, parts of the external surface of the tympanic membrane, and the pharynx. Special sensory (special afferent) • A very minor component of CN X. Provides taste sensation from the epiglottic region. This component will not be discussed further. Overview of SomaticMotor Component • The somatic motor component of CN X provides voluntary control of the following: – Striated muscle of the pharynx. – Striated muscle of the larynx, except for the stylopharyngeus muscle (CN IX) and the tensor veli palatini muscle (CN V). – Palatoglossus muscle of the tongue (the rest of the muscles of the tongue are innervated by CN XII). Origin and Central Course • The somatic motor component originates from the nucleus ambiguus in the reticular formation of the medulla. • Fibers leaving the nucleus ambiguus travel anteriorly and laterally to exit the medulla posterior to the olive as a series of 8 - 10 rootlets. Intracranial Course • Upon emerging from the lateral aspect of the medulla the somatic motor component travels with the fibers of the accessory nerve (CN XI) into the jugular foramen of the skull. The remaining components of the vagus nerve also enter the jugular foramen and give rise to two ganglia (the superior and inferior vagal ganglia) within the jugular foramen. The somatic motor fibers join with the rest of the vagus nerve just below the inferior vagal ganglion. Extra-Cranial Course and Final Innervation • Upon exiting the skull the vagus nerve travels between the internal jugular vein and internal carotid artery within the carotid sheath. The somatic motor fibers leave the vagus nerve as three major branches: • Pharyngeal branch • Superior laryngeal nerve • Recurrent laryngeal nerve Pharyngeal Nerve • The pharyngeal nerve is the principle motor nerve of the pharynx. It branches from the vagus nerve just below the inferior ganglion and travels inferiorly and medially to pass between the internal and external carotid arteries. • The nerve enters the middle constrictor muscle of the pharynx where it spreads out to form the pharyngeal plexus to innervate all muscles of the pharynx and soft palate (except the stylopharyngeus and tensor veli palatini muscles which are innervated by CNs IX and V, respectively). The muscles innervate by the pharyngeal nerve include: • Superior, middle, and inferior constrictor muscles • Levator palatini muscle • Salpingopharyngeus muscle • Palatopharyngeus muscle • Palatoglossus muscle of the tongue Superior Laryngeal Nerve • The superior laryngeal nerve branches from the vagus nerve just below the pharyngeal nerve. The nerve descends in the neck adjacent to the pharynx and splits to form the internal and external laryngeal nerves. • The external laryngeal nerve supplies the inferior constrictor muscle before piercing it to supply the cricothyroid muscle which is involved in the controlling the movements of the vocal folds. • The internal laryngeal nerve pierces the thyrohyoid membrane and is a sensory nerve of the larynx. Recurrent Laryngeal Nerve • The path of the recurrent laryngeal nerve differs on the right and left sides of the body. The left recurrent laryngeal nerve separates from the vagus nerve at the level of the aortic arch. The nerve loops posteriorly around the aortic arch and ascends through the superior mediastinum to enter the groove between the esophagus and trachea. Recurrent Laryngeal Nerve • The right recurrent laryngeal nerve splits from the vagus before entering the superior mediastinum at the level of the right subclavian artery. The nerve hooks posteriorly around the subclavian artery and also ascends in the groove between the esophagus and trachea. • Both recurrent laryngeal nerves pass deep to the lower margin of the inferior constrictor muscle to innervate the intrinsic muscles of the larynx responsible for controlling the movements of the vocal fold Motor Neuron (MN) Lesion • Unilateral damage to the vagus nerve is indicated by: • Hoarseness (due to paralysis of the intrinsic muscles of the larynx on the affected side). • Difficulty in swallowing due to the inability to elevate the soft palate on the affected side (due to paralysis of the levator palatini muscle). • On examination the soft palate droops on the affected side and the uvula deviates opposite the affected side due to the unopposed action of the intact levator palatini muscle. • Unilateral damage to the recurrent laryngeal nerve can occur during surgical procedures in the neck, resulting in hoarseness due to unilateral weakness or paralysis of the muscles controlling the vocal fold on the affected side. Enlargement of the paratrachial lymph nodes, as can be seen in metastatic lung cancer, can lead to compression of one of the recurrent laryngeal nerves with similar results. Overview of Visceral Motor Component • The parasympathetic (secretomotor) component of the vagus nerve consists of efferent fibers which innervate the smooth muscle and glands of the pharynx, larynx, and thoracic and abdominal viscera down to the splenic flexure. • In general, parasympathetic stimulation leads to increased secretion from glands and smooth muscle contraction. Specifically, CN X parasympathetic stimulation has the following effects (think "rest and digest") rest and digest • Cardiac - Slows heart rate • Lungs - Stimulates increased bronchiolar secretions and bronchoconstriction • GI tract- Stimulates increased secretions and motility Visceral Motor Component Origin and Central Course • The visceral motor component fibers originate from the dorsal motor nucleus of the vagus located in the floor of the fourth ventricle (vagal trigone) in the rostral medulla and in the central grey matter of the closed (caudal) medulla. Preganglionic fibers course through the spinal trigeminal tract and nucleus to exit the lateral medulla. Intracranial Course - Visceral Motor Component • Upon emerging from the lateral aspect of the medulla, the visceral motor fibers join the other components of CN X to exit the skull via the jugular foramen. Extra-Cranial Course and Final Innervations • Upon exiting the skull the vagus nerve travels between the internal jugular vein and internal carotid artery within the carotid sheath. Preganglionic fibers to the secretomotor glands of the pharyngeal and laryngeal mucosa travel with the pharyngeal and internal laryngeal nerves discussed above. • Within the thorax the left and right vagus nerves break up into many branches to form plexuses around the esophagus and major blood vessels to the heart and lungs. From the esophageal plexus, the left and right gastric nerves emerge and provide preganglionic parasympathetic innervation to the stomach. Innervation to the intestines and visceral organs generally follow the arterial blood supply to that organ. Overview of visceral sensory component • The visceral sensory component of CN X provides sensory information from the larynx, esophagus, trachea, and abdominal and thoracic viscera, as well as the stretch receptors of the aortic arch and chemoreceptors of the aortic bodies Peripheral Course • Sensory fibers from the plexuses surrounding the abdominal viscera converge and join the gastric nerves which ascend through the esophageal hiatus of the diaphragm and merge with the esophageal plexus. In the thorax, visceral sensory fibers from the heart and lungs also join the ascending fibers in the esophageal plexus which converge to form the left and right vagus nerves which ascend within the carotid sheath between the internal jugular vein and internal carotid artery. • Visceral sensory fibers from the larynx and pharynx join the ascending vagal fibers via the internal laryngeal and recurrent laryngeal nerves. The cell bodies of these afferent neurons reside in the inferior vagal ganglion in the jugular foramen Central Course - Visceral Sensory Component • The central processes of the visceral sensory neurons pass from the inferior vagal ganglion through the jugular foramen and enter the medulla. These fibers descend in the tractus solitarius to synapse in the caudal nucleus solitarius. From the nucleus solitarius, bilateral projections to several areas in the reticular formation and hypothalamus allow reflex control of cardiovascular, respiratory, and gastrointestinal functions. Connections between the reticular formation and the dorsal motor vagus nuclei (via the reticulobulbar pathway) allow most of these reflexes to be mediated by the visceral motor component of CN X Overview of general sensory component • This component of CN X carries general sensory information (pain, temperature, and touch) from the skin of the back of the ear and external auditory meatus, parts of the external surface of the tympanic membrane, and the from the larynx and pharynx. Peripheral Course • Sensory fibers from the external ear, external auditory canal, and external surface of the tympanic membrane are carried via the auricular branch of CN X. These fibers pass into the jugular foramen and enter the superior vagal ganglion where their cell bodies reside. General sensory information from the larynx and pharynx travels in the recurrent laryngeal and internal laryngeal nerves which join and ascend into the jugular foramen with the vagus nerve. The cell bodies of these neurons reside in the inferior vagal ganglion. Central course - general sensory component • The central processes of the general sensory neurons exit the vagal ganglia and pass through the jugular foramen to enter the brainstem at the level of the medulla. Upon entering the medulla these fibers descend in the spinal trigeminal tract and synapse in the spinal nucleus of the trigeminal Clinical Correlation • Stimulation of the fibers of the auricular nerve in the external auditory meatus can cause coughing and/or vomiting by reflex activation of the visceral motor component of the vagus nerve via the reticulobulbar pathway.