* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Sexually Transmitted Diseases
Human papillomavirus infection wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Diagnosis of HIV/AIDS wikipedia , lookup
Neonatal infection wikipedia , lookup
Hepatitis B wikipedia , lookup
Epidemiology of HIV/AIDS wikipedia , lookup
Herpes simplex wikipedia , lookup
Herpes simplex virus wikipedia , lookup
Hepatitis C wikipedia , lookup
Microbicides for sexually transmitted diseases wikipedia , lookup
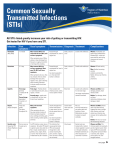
Sexually Transmitted Infections Presented by: Why do you need to know about STIs? The average age both male and female Canadians have sex for the first time is 16.5. 28% of teens aged 15-17 report having had sexual intercourse at least once. By age 20-24, this increases to 80%. In a 2005 report, 41% of males aged 15-17 and 39% of those aged 18-19 reported having more than one sexual partner in the previous year. For females in the study, 29% of 15-17 year olds and 31% of those aged 18-19 reported having more than one sexual partner in the previous year. Overview What is an STI? What causes STIs? Risk Factors How can STIs be transmitted? Common STIs What should you do if you suspect you may have an STI? Preventing the spread of STIs Quiz What is an STI? Sexually transmitted infections are infections usually transmitted through sexual intercourse. STIs often do not have any symptoms; it is possible to have an STI and not even be aware of it. General Warning Signs different vaginal discharge discharge from penis burning during urination or sex sores or growths on genitals or around anus itch or odour Any STI… can increase chances of getting another STI. can be passed from the mother to the baby during the birthing process. may lead to infertility in women. What causes STIs? bacteria viruses curable with antibiotics easily cured if caught early; however, there are often no symptoms http://matcmadison.edu/is/hhps/mlt/mljensen/image s/Bacterium.jpeg http://micro.magnet.fsu.edu/c ells/viruses/images/virus.jpg not curable other organisms can treat symptoms www.ento.okstate.edu/ddd/insects/pubiclice.htm Risk Factors Anyone who has had sexual intercourse is at risk for having an STI. factors that increase risk: - more than one sexual partner - sex with someone who has more than one partner - sex without a condom STIs are NOT transmitted via… toilets eating utensils holding hands towels STIs are NOT transmitted via… bedding swimming pools telephones insect bites How are STIs transmitted? sharing/using dirty needles sexual intercourse (anal, vaginal, oral) at birth Before we learn about STIs… What do normal genital areas look like? Female http://upload.wikimedia.org/wikipedia/commons/thumb/2/2d/Vagina-anatomy-labelled2.jpg/444px-Vagina-anatomy-labelled2.jpg Male http://upload.wikimedia.org/wikipedia/commons/8/84/Human_penis_both_flaccid_and_erect.jpg Common STIs bacterial: chlamydia gonorrhea syphilis viral: HIV human papillomavirus/genital warts hepatitis Chlamydia & Gonorrhea chlamydia: up to 90% of women and 70% of men with chlamydia have no symptoms gonorrhea (‘The Clap’): 80% of women & 40% of men with gonorrhea have no symptoms common symptoms: - discharge from penis/vagina - painful urination and bowel movements - painful intercourse - in women: bleeding between periods, bleeding after intercourse Symptoms usually appear a couple of days to a few weeks after infection. Prevalence of Chlamydia http://www.health.alberta.ca/documents/STI-ND-Annual-Report-2011.pdf Prevalence of Gonorrhea http://www.health.alberta.ca/documents/STI-ND-Annual-Report-2011.pdf Updated October 2013 Chlamydia can easily be treated with a single dose of antibiotics a significant cause of blindness passed through vaginal/anal sex, but not usually through oral sex Gonorrhea can be treated with antibiotics arthritis pelvic inflammatory disease Syphilis several stages of infection: primary 3 weeks to 3 months after infection chancres on genital area—painless and VERY contagious secondary 2-3 months spotty skin rash fever, fatigue, hair loss Syphilis chronic period of no symptoms may continue for years! may progress right on to tertiary tertiary serious organ damage occurs anytime after one year affects eyes, brain, muscles can be fatal Updated March 2008 Syphilis infection can be spread to fetus in pregnant women and cause stillbirth or lifelong disabilities fetal abnormalities prenatal care! treatment: infection <1 year long: a single shot of penicillin infection >1 year long: many doses of penicillin over three weeks Human Papillomavirus HPV can lead to genital warts in the genital or anal areas #1 cause of cancer of the cervix symptoms: - genital warts (cauliflower-like) - often recurrent and resistant - up to 90% of people have no symptoms (self-heal within 2 years) extremely common, with up to 80% sexually active people being infected newborn babies rarely get the virus during the birthing process Human Papillomavirus diagnosis of HPV done using the Pap smear once sexually active, females need yearly Pap smears symptoms (genital warts) can be treated, but there is no cure Human Papillomavirus protection: females are vaccinated between the ages of 9-26 (up to age 45 in women at high risk) Gardasil®: offers protection against cervical cancer and genital warts given as 3 injections over 6 months covers 4 out of 6 HPV viruses that can cause cancer (70% of cervical cancer and genital warts) Speak to a health care professional about whether you should receive it. Herpes symptoms can occur 2-10 days after exposure may show no symptoms can cause itching, blisters/sores, pain/discomfort of genital area, difficulty or pain in urinating estimated 1/7 Canadians aged 14-59 have herpes estimated only 1/10 of those know they have it Herpes symptoms can be treated, but herpes cannot be cured may be passed on to partners at any time viral shedding occurs even when blisters are absent pregnant women should be tested herpes can be passed on to unborn child, causing disability or miscarriage Herpes recurrent episodes are usually shorter and less severe people have on average about four outbreaks per year stress and anxiety are common triggers for outbreaks HIV/AIDS True or False? Only MSMs, sex trade workers, and people in third world countries can get HIV. There is a cure for HIV. HIV/AIDS HIV = Human Immunodeficiency Virus; AIDS = Acquired Immune Deficiency Syndrome HIV is a virus that attacks the immune system; an HIV infection can progress to the AIDS syndrome HIV may have no symptoms, or mild symptoms; AIDS patients can have life-threatening infections or cancer HIV/AIDS an estimated 70 000 people have HIV in Canada; 2500 new cases each year HIV infection increases chances of getting another STI, and vice versa can be passed from a mother to baby through breast milk or at birth There is no cure for HIV! Hepatitis hepatitis = inflammation of the liver many types of hepatitis; most common are A, B, C diagnosed via simple blood tests vaccines available for Hepatitis A & B each one is transmitted a bit differently: A - fecal/oral B - blood and body fluids C - blood products Hepatitis A & B symptoms: flu-like symptoms, darker urine Hepatitis C symptoms: extreme fatigue may have no symptoms Other ways to get HIV and hepatitis IV drug use (20-40% of IV drug users are infected with hepatitis C within the first year, and up to 90% after 5 years; can also get HIV from IV drug use) tattoos Prevention! Don’t share needles, syringes, and other drug paraphernalia. What should I do if I suspect I have an STI? stop having sex get tested at a doctor’s office or clinic treat your partners as well Preventing STIs abstinence: the only 100% way of preventing the spread of STIs mutual monogamy: limiting sex to one uninfected partner who only has sex with you It’s a good idea to ask your partner if she/he has an STI and work out a risk reduction plan. Preventing STIs Do not use/share needles with anyone. Use a condom during intercourse; this can drastically decrease the chances of getting an STI. (N.B. Proper use is EXTREMELY IMPORTANT!) Other birth control methods: the pill, diaphragms, spermicide—do those prevent STIs? Test and treat for STIs as quickly as possible. Condom Disclaimer Condoms are not 100% effective against infections that can be transferred from skin to skin contact (i.e. herpes, HPV). Condom Dos and Don’ts Do store in a cool dry place. Do not leave condoms in the sunlight, a wallet or glove compartment. Do check the expiry date. Do use a water based lubricant (e.g. KY Jelly®). Do not use oil-based product (e.g. Vaseline®). Condom Dos and Don’ts Do open a package carefully. Do not open with teeth or scissors. Do not use spermicide with condoms; it may cause vaginal irritation or cause latex to break down. Do practice putting on and taking off the condom. Do read the instructions carefully. Resources school guidance counselor www.sexualityandu.ca family doctor, pharmacist, other health care professional walk-in clinics (Medicentres, SHINE Clinic) Capital Health STD centre and info line 1-800-772-2437 What your pharmacist can do for you advice referral to support services condoms and other methods of birth control Plan B® clean needles and syringes Quiz! – True or False 1. STIs are transferred through using public toilets. 1. False: STIs are commonly transferred by sexual intercourse and dirty needles. 2. STI’s are caused by a variety of organisms. 2. True: Bacteria, viruses, and other organisms may all cause STIs. 3. Chlamydia is curable. 3. True: Chlamydia can be treated with antibiotics. Quiz! – True or False 4. HIV is more easily transmitted when another STI is present. 4. True: The presence of an STI increases the likelihood of HIV transmission. 5. HPV can be cured. 5. False: HPV can be treated but not cured. 6. Gonorrhea may lead to infertility in women. 6. True: Even though gonorrhea often has no symptoms, it can cause infertility. Quiz! – True or False 7. Hepatitis is an inflammation of the liver. 7. True: The hepatitis virus affects the liver. 8. Herpes can be transmitted even when no symptoms are present. 8. True: Herpes can be transmitted before any visible signs occur. 9. Syphilis is not a fatal STI. 9. False: If untreated, syphilis can be fatal. 10. Condoms provide 100% protection against STIs. 10. False: Only abstinence provides 100% protection. Updated March 2008 Questions? References UptoDate. (September 2013). Patient Information: Chlamydia (Beyond the Basics). Retrieved October 12, 2013: http://www.uptodate.com/contents/chlamydia-beyond-thebasics Minnesota Department of Health. (March 2013). What you and your partner should know about gonorrhea and chlamydia. Retrieved October 12, 2013: http://www.health.state.mn.us/divs/idepc/dtopics/stds/importantinfo.html Cleveland Clinic. (2013). Understanding Cervical HPV. Retrieved October 12, 2013: http://my.clevelandclinic.org/disorders/genital_warts/hic_understanding_hpv.aspx CTV News. (April 2013). One in 7 Canadians has genital herpes: StatsCan study. Retrieved October 12, 2013: http://www.ctvnews.ca/health/health-headlines/one-in-7canadians-has-genital-herpes-statscan-study-1.1241792 Public Health Agency of Canada. (November 2012). At a Glance – HIV and AIDS in Canada: Surveillance Report to December 31st, 2011. Retrieved October 12, 2013: http://www.phac-aspc.gc.ca/aids-sida/publication/survreport/2011/dec/index-eng.php Infectious Diseases Society of America. (2013). A Systematic Review and MetaAnalysis of Interventions to Prevent Hepatitis C Virus Infection in People Who Inject Drugs. Retrieved October 12, 2013: http://jid.oxfordjournals.org/content/204/1/74.full
























































![itching and scratching guided notes [2/17/2017]](http://s1.studyres.com/store/data/005554232_1-fdcd1a11e73f76c0d26c4b298e3f53ab-150x150.png)