* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Atrial Fibrillation 2014. AF prevalence is around 1.6%, although in
Survey
Document related concepts
Transcript
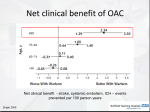
Atrial Fibrillation 2014. AF prevalence is around 1.6%, although in the over 75s it is greater than 10%. AF increases stroke risk 5 fold compared to people without AF. NICE CG 180 June 2014 advises several changes, including: - Aspirin is no longer recommended. Anticoagulation needs to be used to reduce stroke risk. - Rate control should be offered for the majority (1st line). - CHA2DS2Vasc score (rather than CHADS2) to assess stroke risk. - HASBLED to assess bleeding risk for all patients. - Stratify stroke risk for paroxysmal AF and Atrial flutter in the same way as for permanent AF. - Increased use of left atrial appendage ablation (see later) for those who don’t respond to conventional therapies. Classification of AF Paroxysmal = spontaneous resolution within 7 days. Persistent = > 7 days & indefinite unless cardioverted. Permanent = > 7 days and sinus rhythm unachievable. Screening - No evidence of benefit for population screening in asymptomatic individuals. - Opportunistic case finding for symptomatic individuals. Check pulse if breathless, palpitations, syncope/dizziness, chest discomfort, stroke/TIA. ADMISSION is indicated: - In the presence of compromise, severe or life threatening. - If new onset AF within 48 hours, to consider immediate cardioversion. OTHERWISE, manage as per FOLLOWING FLOW CHART: 1/. Suspected AF (irregular pulse found opportunistically) ECG. (order 24 hour ECG if paroxysmal AF suspected) AF or flutter confirmed Assess stroke risk: CHA2DS2Vasc (on mothership.) 2 or more: – offer anticoagulation. 1 (men): consider anticoagulation, 1 (women): no antithrombotics score 0 :no antithrombotics Assess bleeding risk: HASBLED (on mothership.) Score 3 or more, high risk.) Discuss anticoagulation with the patient : – No anticoagulation - Warfarin - NOAC (2nd Line if drugs CI/not tolerated = Left atrial appendage occlusion) Use patient decision aid from NICE CG180. http://www.nice.org.uk/guidance/cg180/resources/cg180-atrialfibrillation-update-patient-decision-aid2 Add rate control agent* 1st line (any beta blocker, not sotalol, or rate limiting calcium channed blocker – usually diltiazem). Aim for pulse 80-90. Bloods (morning): FBC, Cr&Es, Hba1c, non fasting lipid profile, TSH,LFT, clotting screen. Echo: NOT routine. Only if suspected structural or functional heart disease (eg. murmur or failure) or, cardioversion planned or, needed for better risk stratification for antithrombotic therapy ( eg. Those with high CHA2DS2Vasc and HASBLED scores Specialist referral: Routine referral not needed. Refer promptly (within 4 weeks) if treatment fails to control symptoms. Or if valvular cause eg. Mitral stenosis. *Rhythm control only if: reversible cause for AF eg pneumonia, AF is resulting in Heart Failure or new onset AF 2/. CHA2DS2Vasc Score Stratifies Stroke risk. www.chadsvasc.org Score 2 or more (men and women): offer anticoagulants Score 1 in men only: consider anticoagulants Score 1 in women only: no antithrombotics Score 0 (men and women): no antithrombotics Risk Factor CHA2DS2Vasc: maximum=9 Congestive cardiac failure Hypertension Age 1 1 1 (if 65-74) 2 (if 75 and over) 1 2 1 1 Diabetes Stroke/TIA (history of) Sex (female) Vascular disease (MI, PAD, aortic plaques) HASBLED score Stratifies bleeding risk. www.chadsvasc.org Score 3 and over identifies high risk of bleeding. HASBLED criteria (3 or more=high bleeding risk) Hypertension- uncontrolled (SBP>160) Abnormal renal function (on dialysis/transplant/cr>200) &/or Abnormal liver function (chronic hepatic disease eg cirrhosis, or abnormal LFTs eg. Brb >2x upper limit of normal, AST/ALT/ALP>3x upper limit normal) Stroke Bleeding (PMH of bleeding tendency/anaemia) Labile INRs (unstable INRs or INRs frequently not in therapeutic range) Elderley (age >65) Drugs (eg. On aspirin/NSAIDs) or alcohol abuse (1 point each) Points: maximum =9 1 1 point for any renal abnormalities 1 point for any liver abnormalities 1 1 1 Score 0 if never had warfarin 1 1 or 2 3/. Anticoagulation When aspirin is compared with anticoagulants, there is clear benefit from anticoagulation in terms of: All cause mortality Ischaemic stroke There is also a lack of evidence for other antiplatelets eg. Clopidogrel. Benefits of anticoagulation: Compared with placebo, NICE found anticoagulants (basically this means warfarin): Reduced all cause mortality:22 fewer per 1000 treated Reduced ischaemic stroke: 37 fewer/1000 treated (NICE give no time frames, probably 1y) 1. Warfarin Target for treatment: INR 2.5 (2-3) Warfarin in older people: NICE suggests that : For most, the benefit of anticoagulation outweighs the risks. We should NOT withhold warfarin solely because the person is at risk of having a fall. Warfarin: assessing time in therapeutic range: Aim for a time in therapeutic range (TTR) of more than 65% (TTR should be calculated over at least 6 months, excluding the initial 6 weeks) Poor control is shown by (in last 6months): TTR of 65% or less 1 INR higher than 8 2 INRs higher than 5 2 INRs less than 1.5 Remember to ask regarding alcohol intake, as well as cognitive function, compliance, other medication. Note: INR >8 – admit to consider Vit K administration. Raised INR ( 3 to <8) – patient is likely to be advised by anticoag clinic re dose omission and plan. INR (any) + significant bleeding = admit. Warfarin MAY be used with antiplatelets if the patient has also had an MI, for 2o prevention of cardiovascular disease . These are secondary care decisions and may be for a limited period of time eg. 1 year post MI. Note that newer antiplatelets eg. Prasugrel, ticagrelor and NOACs should not be used in combination due to lack of evidence. Remember, if the plan is not clear in the notes, use Advice and Guidance Choose and Book referral to cardiology to confirm the plan. 4/. Initiation of warfarin: Instructions (as below) are on the referral form. Link to form with guidance are on Atrial Fibrillation Template on Mothership. Ensure bloods are checked as per flow chart, prescribe warfarin 2mg od for 7days. Patient to attend blood testing on D7 or 8 at CRH (or RHI), where INR will be checked and counselling re warfarin will be offered in pharmacy. For housebound patients, fax a referral to the anticoagulation clinic and they will make arrange to visit the patient at home. 2. NOACs NICE advises offer NOACs or warfarin as thromboprophylaxis, provided use is within the NICE guideline for each NOAC (see later). Basically, this means a NOAC can be offered in place of warfarin, in non valvular AF if any of the following risk factors are present: Stroke/TIA Diabetes Heart failure Hypertension Over 75 years of age HOWEVER, SIGN remind us (SIGN 129,2012) The relative lack of experience of use of NOACs. Lack of an antidote Higher rates of GI bleeding (but fewer intracranial bleeds), especially with higher doses and in the elderly (total bleeding risk the same). No head to head trials between NOACs, but all 3 NOACs seem to be broadly similar with regard to bleeding risk and stroke prevention. Note: poor compliers on warfarin may also be poor compliers on NOACs. NOACs also have a short half life, so anticoagulation may be erratic in result – but you won’t know, because it isn’t being measured. Beware renal impairment and abnormal liver function when considering NOACs. See prescribing guidance. Care ++ therefore, if suspected alcohol abuse . Dabigatran Inhibits thrombin Ref: NICE 2012 TA249 Dose 150mg bd or, 110mg bd if > 80 years old (or if 75-80 with high bleeding risk/low thromboembolic risk) Beware renal impairment. Use lower dose of 110mg bd if eGFR 30-50. Check eGFR before start and annually if >75, weight <50kg or eGFR 30-50 Rivaroxaban Direct factor Xa inhibitor (also licensed for treatment and prevention of recurrence of VTE) Ref: NICE 2012 TA256 5/. Dose 20mg od with evening meal. Note dose adjustment with renal impairment eGFR <50, see BNF. Apixaban Direct factor Xa inhibitor Ref: NICE 2013 TA275 Dose 5mg bd. Reduced dose eGFR<30 or if at least 2 of: >80y, <60kg or Creat >133 (2.5mg bd) Beware hepatic impairment – do not use if transaminases >2x upper limit of normal. Common Side Effects of all 3: Nausea, GI upset, bleeding and anaemia. Monitoring Ensure that renal function and LFTs are checked pre treatment (as per flowchart) and annually, thereafter. Switching from Warfarin to a NOAC GP-Update suggests as below – taken from SPC Jan 2013 – as well as considering advice from a local expert. Dabigatran Stop warfarin. Start dabigatran as soon as INR is <2.0. Rivaroxaban Stop warfarin. Start rivaroxaban when INR is <3.0. Note: when on rivaroxaban the INR values will be falsely elevated. Apixaban Stop warfarin. Start apixaban when INR is <2.0. Note: all NOACs are licensed for prevention of VTE after elective hip/knee replacement. 3. Left Atrial Appendage Occlusion. In those whom anticoagulation is not tolerated or contraindicated – offer left atrial appendage occlusion if: - Persistent AF - Paroxysmal AF The left atrial appendage is the embryological remnant of the left atrium and is a little blind ending passage/sac off the left atrium. There is a risk of stasis and thrombus formation and it is thought to be a major source of thrombus in AF. It can be done in the catheter lab. Rate Control For the vast majority. See Flow chart on page 2. Aim for pulse 80-90. 1. Beta Blocker (any except sotalol) or, 2. Rate Limiting Calcium Channel Blocker (usually diltiazem)..The latter are unlicensed, but recommended by NICE. 3. Only consider digoxin if sedentary patient with non-paroxysmal AF Do NOT use amiodarone. 6/. If monotherapy ineffective, try dual therapy with any two of 1., 2., or 3. If dual therapy ineffective, refer – rhythm control or ablation. Rhythm control For a minority. See Flow chart on page 2. 1. Electrical cardioversion is 1st choice (can add amiodarone from 4w previous to 12m post cardioversion to help maintain sinus rhythtm once restored) Can be done in standard way needing INRs for 4 weeks in therapeutic range or, with transoesophageal echo as guidance without prolonged anticoagulation (can check that there is no thrombus in the heart) 2. Drug treatment. This should be a cardiologist’s decision to maintain sinus rhythm after cardioversion. 1st line – standard beta blocker (not sotalol), then Dronedarone (a secondary care drug)– after successful cardioversion and 1st line treatment has failed and who have at least 1 of the following cardiovascular risk factors: Hypertension on rx with drugs of at least 2 different classes. Diabetes mellitus Previous TIA, stroke or systemic embolism Left atrial diameter of 50mm or greater or, Age 70 years or older and, - Who do not have left ventricular systolic dysfunction and, - Who do not have a history of, or current, heart failure. Consider amiodarone for those with LV impairment or heart failure. Do not offer class 1c antiarrhythmics – flecainide or propafenone - to those with ischaemic or structural heart disease 3. Pill in the Pocket For patients with paroxysmal AF with infrequent episodes and few symptoms or known trigger eg. caffeine or alcohol – can consider no treatment or ‘pill in the pocket’eg. flecainide in those who: Have no LV dysfunction,valvular or ischaemic heart disease Have infrequent, symptomatic episodes Have systolic BP>100mm hg and resting pulse >70 Are able to understand how and when to use the medication. Surgical techniques If drug treatment fails to control symptoms of AF or high ventricular rate consider: Left atrial catheter ablation (paroxysmal AF) Left atrial surgical (or catheter) ablation (persistent AF). Discuss risks and benefits with each person. Pace and AV node ablation (permanent AF and symptoms or high ventricular rate and LV dysfunction). 7/. Paroxysmal AF Stroke prevention – assess for anticoagulation as for all AF using CHA2DS2Vasc and HASBLED, then REFER to consider: Long term rhythm control or ‘pill in the pocket’ (as in 3. Above). Offer a Personalised Package of Care Go to AF personalised package of care auto-consult on S1, link on Atrial Fibrillation template. As per NICE: Ensure that the package of care is documented and delivered, and that it covers: stroke awareness and measures to prevent stroke rate control assessment of symptoms for rhythm control who to contact for advice if needed psychological support if needed up-to-date and comprehensive education and information on: - cause, effects and possible complications of AF management of rate and rhythm control anticoagulation - practical advice on anticoagulation in line with recommendation 1.3.1 in ‘Venous thromboembolic diseases (NICE CG 144) support networks (eeg. Cardiovascular charities) - Issue appropriate PILs from Atrial Fibrillation Template on mothership. QOF Rules - AF001: register - AF003: in those patients with AF in whom there is a CHADS2 score of 1, the percentage of patients who are currently treated with an antiplatelet agent or anticoagulation. - AF004: in those patients in whom there is a record of CHADS2 score >1, the percentage of patients who are currently treated with anticoagulation. 8/. References: NICE CG180 (update June 2014) www.gp-update.co.uk http://www.nhsemployers.org/~/media/Employers/Documents/Primary%20care%20contracts /QOF/2014-15/Summary%20of%20changes%20to%20QOF%202014-15%20%20England%20only.pdf Greater Huddersfield Commissioning Group (GHCCG) QOF QP Pathway. 9/.