* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download H.Delshad MD
Survey
Document related concepts
Transcript
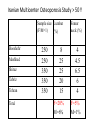
H.Delshad M.D Endocrinologist Research Institute for Endocrine Sciences The burden of osteoporosis ►The most common metabolic bone disease ►The most common cause of Fx. in older adults ►2 million fracture each year : • 300,000 hip Fx. • 547,000 Vert. Fx. • 135,000 Pelvic Fx. • 20% end up in nursing homes • 20% mortality within 1 year of fracture • 2/3 never return to pre-fracture functional level Annual incidence of common diseases Comparative annual incidence of osteoporotic fractures and other disease end-point in women 2,500,000 2,000,000 - 1,500,000 - 1,000,000 - 2,050,000 425,000 500,000 0 - 370,000 192,000 Osteoporotic fractures Stroke Heart attack Breast cancer A huge care gap exists after a fracture The vast majority of men and women presenting at Canadian hospitals with fragility fractures are neither screened nor treated for their underlying osteoporosis to prevent future fractures. Iranian Multicenter Osteoporosis Study > 50 Y Sample size Lumbar (F/M=1) (%) Booshehr Mashhad Shiraz Tabriz Tehran Total 250 250 350 350 350 Femur neck (%) 8 25 25 20 15 4 4.5 6.5 6 4 F=20% M=6% F=5% M=1% Osteoporosis: Definition Osteoporosis is the result of dysregulation of bone remodeling Osteoporosis: Definition • Low bone mass • Microarchitectural deterioration • Susceptibility to fracture Osteoporosis : who is at risk? Osteoporosis : Risk factors Osteoporosis : Risk factors Osteoporosis : Diagnosis • Osteoporosis is a ‘silent’ condition with few clinical symptoms and a fracture is often the first sign. • Like hypertension and atherosclerosis, osteoporosis can be defined by an intermediate outcome , in this case, low bone mineral density ( BMD ). Osteoporosis : Clinical signs • • Fracture ● • pain Loss of height Kyphosis Respiratory difficulty Gastrointestinal symptoms ( abdominal pain, hernia, reflux) Long-term disability Depression Indicators of secondary causes of osteoporosis (e.g. glucocorticoid treatment; GI tract disease such as Crohn’s disease or Celiac disease; hematological malignancies e.g. myeloma) • • • • • • • Osteoporosis : Diagnosis • Plain film • SPA • DPA • DEXA : The most common method for measurement of BMD • QCT • US • MRI BMD - Who Needs It ? •All women > 65 years •Men > 70 years •Post-menopausal woman with major risk factors •All individuals > 50 years with history of osteoporotic fracture •All individuals on long term steroids •Men with hypogonadal conditions •Patients with diseases a/w bone loss and fracture DEXA Apparatus DEXA Technology Detector (detects 2 tissue types - bone and soft tissue) Patient Collimator Photons (pinhole for pencil beam, slit for fan beam) X-ray Source (produces 2 photon energies with different attenuation profiles) ( g/cm2 ) Which Skeletal Sites Should Be Measured? Every Patien • Spine – L1-L4 • Hip – Total Proximal Femur – Femoral Neck – Trochanter Some Patients • Forearm (33% Radius) – If hip or spine cannot be measured – Hyperparathyroidism – Very obese Use lowest T-score of these sites Why measure both spine & hip ? • Spine-hip discordance a) Find lower BMD site • Fracture prediction a) Spine BMD for spine Fx b) Hip BMD for hip Fx • Flexibility in monitoring Contraindications for spinal BMD measurement • Pregnancy • Recent oral contrast media (2-6 days) • Recent nuclear medicine test (depends on isotope used) • Inability to remain supine on the imaging table for 5 min without movement • Spinal deformity or disease , orthopedic hardware in the lumbar spine Diagnosis Caveats • T-score -2.5 or less does not always mean osteoporosis: – Example: osteomalacia • Clinical diagnosis of osteoporosis may be made with T-score greater than -2.5 – Example: a traumatic vertebral fracture with T-score equals -1.9 • Low T-score does not identify the cause and medical evaluation should be considered: – Example: celiac disease with malabsorption Osteoporosis: Laboratory Osteoporosis: who should be treated Osteoporosis : FRAX FRAX : Clinical risk factors FRAX was developed to calculate the 10-year probability of a hip and a major Osteoporotic Fx. www.nof.org or www.shf.ac.uk/FRAX Ten-year probability of osteoporotic fractures (%) according to BMD T-score at the femoral neck in women aged 65 years from the UK Ten-year probability of osteoporotic fractures (%) according to body mass index (BMI) in women aged 65 years from the UK. • Adequate intake of dietary calcium (1200 mg/d) 1 2 • Intakes in excess of 1,200 to 1,500 mg per day have limited potential for benefit and may increase the risk of developing kidney stones or cardiovascular disease • 800 to 1,000 IU of vitamin D / day for adults age 50 and older • This intake will bring the average adult’s serum 25(OH)D concentration to the 30 ng/ml • Regular weight-bearing exercise 3 4 5 • walking, jogging, Tai-Chi, stair climbing, dancing and tennis, weight training and other resistive exercises. •Fall Prevention • Avoidance of Tobacco use and excessive alcohol intake Pharmacotherapy ► Biphosphonates • Alendronate • Risedronate • Ibandronate • Zoledronic acid ► Calcitonins ►Denosumab ► Eestrogens ► rPTH ► SERMs ► Strontium ranelate Bisphosphonates • In bone, bisphosphonates accumulate in the hydroxyapatite mineral phase, its concentration is increased by a factor of 8 at sites of active bone resorption. • Bisphosphonates enter osteoclasts and reduce resorption and promotes early cell death. • Osteoclasts inhibition allows Osteoblasts to slightly increase BMD 1st line therapy for osteoporosis • Alendronate • Risedronate • Ibandronate • Zoledronic acid Bisphosphonates :Clinical Evidence Effect on Lumbar Spine and Femoral Neck BMD in Postmenopausal Women Alendronate : Residronate Ibandronate Drug Alendronate (Fosamax) Ibandronate (Bonivia) Residronate (Actonel ) Dose Vertebral Non-vertebral For prevention: Tab. 5mg/d or 35mg/week 5 , 10 , 75 mg For treatment : 10mg/d or 70mg/week 50% 50% Tab. 2.5 , 150 mg Amp. 3mg /3ml 50% - 41 – 49% 36% 70% 25 – 41 % For treatment : 2.5mg/d or 150mg/mon. 3mg/IV every 3- month For prevention & treat. 5mg/d ay Tab. 5 , 35 , 150 mg 35mg/week 150mg/month Zoledronic Acid (Reclast) Decrease Fx risk Over 3-year Amp. 4 mg For prevention & treat. 4mg/100 ml IV infusion Once yearly for treatment Once every 2-y for preven. Solution Zoledronic Acid ( Reclast , Zometa ) $ 1315.71 Powder for Solution Zoledronic acid has a high binding affinity for hydroxyapatide Single IV injection of human equivalent dose of zoledronic acid preserve bone micoartictecure in adult Rats 4 µ/kg 20 µ /kg 100 µ /kgµ Micro-CT image of adult s Rats proximal tibial metaphysis ( at 32 weeks) Bisphosphonates :Side Effects • An acute-phase reaction: Fever, Myalgia, Bone pain, Influenza-like symptoms , Headache, Arthralgia and Weakness occurs in 20% of patients after an initial intravenous infusion of Zoledronic Acid. ( Usually lasts 2 – 3 days ) • Atrial fibrillation : Zoledronic acid compared with placebo (1.3 percent vs 0.4 percent); the effect of other bisphosphonates on the incidence of atrial fibrillation is uncertain. • GI Problems : Erosive esophagitis, ulceration, and bleeding with daily oral Alendronate or Residronate , but occur rarely with current (nondaily) regimens. • Bone Problems: - Osteonecrosis of the jaw (particularly following IV bisphosphonate for cancer) - Atypical fractures of the femoral shaft Osteonecrosis of the jaw • Approximately 1 in 10,000 to 1 in 100,000 patient-years in patients taking oral bisphosphonates for osteoporosis Atypical fracture A number of recent case reports and series have identified a subgroup of atypical fractures of the femoral shaft associated with Bisphosphonate use. A population based study did not support this association. Such a relationship has not been examined in randomized trials. Secondary analyses of three large, randomized bisphosphonate trials: the Fracture Intervention Trial (FIT), the FIT Long-Term Extension (FLEX) trial, and the Health Outcomes and Reduced Incidence with Zoledronic Acid Once Yearly (HORIZON) Pivotal Fracture Trial (PFT). The occurrence of fracture of the subtrochanteric or diaphyseal femur was very rare, even among women who had been treated with bisphosphonates for as long as 10 years. In Sweden, 12,777 women 55 years of age or older sustained a fracture of the femur in 2008. 1271 women had a subtrochanteric or shaft fracture and 59 patients with atypical fractures. The relative and absolute risk of atypical fractures associated with bisphosphonate use was estimated Although there was a high prevalence of current bisphosphonate use among patients with atypical fractures, the absolute risk was small. Conclusions These population-based nationwide analyses may be reassuring for patients who receive bisphosphonates. Calcitonin • Salmon’s calcitonin : ○ Prolonge action and greater potency compared to mammalian source. ○ Inhibits osteoclast activity and osteoclast lifespan ○ Analgesic effect ○ Not appropriate as 1st line treatment ○ Only use as 2nd or 3rd line treatment in patients who cannot tolerate bisphosphonates Calcitonin 200 IU , Intra-nasal spray : ○ 33% reduction in new vertebral fractures ○ 36% reduction in those with history of previous fractures (PROOF study) ○ No effect on non-vertebral fractures Nasal Calcitonin : Effect on lumbar spine BMD ( PROOF : 5 –Y analysis ) PROOF : Prevent Recurrence Of Osteoporotic Fractures Am J Med , 2000 ; 109: 267- 276 Roles of RANK and RANKL, in Osteoclast Differentiation and Function •Receptor activator of nuclear factor-kB (RANK) on the surface of osteoclast precursor is activated by the cytokine RANK ligand (RANKL), which is produced primarily by osteoblasts. • This activation, influences the differentiation of osteoclasts. • RANK signaling is also thought to exert anti-apoptotic effects. Denosumab Is a fully human monoclonal antibody to the receptor activator of nuclear factor-κB ligand (RANKL) that blocks its binding to RANK, inhibiting the development and activity of Osteoclasts, decreasing bone resorption, and increasing bone density. FREEDOM Trial : 9.2% 6.0% As compared with subjects in the placebo group, subjects in the denosumab group had a relative increase of 9.2% in bone mineral density at the lumbar spine and 6.0% at the total hip FREEDOM Trial : Changes in mean values for serum C-telopeptide of type I collagen (CTX) and serum pro-collagen type I N-terminal propeptide (PINP) are shown for 160 subjects who were included in a sub-study of bone-turnover markers Prolia : Adverse effects • • • • • • • • • Back pain, muscle pain, pain in the arms or legs Constipation Skin inflammation Severe allergic reactions Bladder infection Ear pain Severe stomach pain Hypocalcemia swelling or pain in jaw. ESTROGEN THERAPY OR HT Estrogens : ○ Bind to estrogen receptors on bone ○ Block production of cytokines and inhibit bone resorption and increase BMD ○ Reduced vertebral (33%) and non-vertebral (27%) fractures Women Health Initiative ( WHI) : Large investigation of prevention strategies for cancer ,CVD and osteoporotic fracture initiated in 1992. It was a very, very large study sponsored by the National Institutes of Health (NIH), in total enrolling more than 64,000 people in a clinical trial and 100,000 people in an observational study. It is a huge federally funded study. n=16,608 Postmenopausal women 50 -79 years n= 8506 Conjugated Estrogen= 0.625 mg/d MPA = 2.5 mg/d n=8102 Placebo HRT component of the WHI Summary of results at 5.2 years ( early termination) In post-menopausal women with an intact uterus, HRT was associated with : Cpolorectal cancer -37% Hip and clinical Vertebral fractures -34% HRT component of the WHI Summary of results at 5.2 years ( early termination) In postmenopausal women with an intact uterus, HRT was associated with : • 29 % increase in CHD events • 22% increase in total CVD • 26% increase in invasive breast cancer • 41% increase in stroke • 111% increase in venous thrombosis Current Indications for HT ○ 2nd line treatment due to risk for breast and endometrial cancers ○ Only for post-menopausal women who cannot tolerate non-estrogen medications ○ To be used with the lowest dose possible and for the shortest period of time to achieve treatment goals Women,s Health Initiative (WHI) Risk Benefit 29% increase CAD 41% increase Stroke 26% increase BC EARLY STOP Clear harm : VTE FRACTURE REDUCTION COLON CANCER SERMs Raloxifene : an alternative to HRT • Selective estrogen receptor modulators • Binds to estrogen receptors • Estrogen agonist activity on bone and circulating lipoproteins • Estrogen antagonist activity on breast and endometrial tissues • Increased risk for DVT • Does not block vasomotor symptoms of menopause • Increased spine BMD by 2.3% and hip BMD by 2.5% after 3 years 50% reduction in spine fractures • No effect on hip or other non-vertebral fractures • 60mg coated tablets taken once daily • Must be stopped 72 hours prior to and during prolonged immobilisation • Decreased absorption with Ampicillin. Effect of Raloxifene on vertebral fractures after 4 years of treatment The Multiple Outcomes of Raloxifene Evaluation (MORE) study (6800 subjects) Ral. 60 mg Ral. 120 mg % of women with incident vertebral fracture Pbo Pooled study population With ≥ 1 previous V. fracture J Clin Endocrino Metab. 2002, 87 : 3609-3617 Without previous V. fracture SERMs Adverse reactions • Headaches • Dizziness • Sweating • Nausea • Stuffy nose • Various pains • General weakness Recombinant PTH Continuous high-dose PTH increases Osteoclast-mediated bone resorption Mechanism of action of PTH on Osteoblasts Intermittent low-dose PTH increases bone formation Recombinant PTH rPTH is anabolic agent • Low dose , daily SC injection : enhance bone remodelling • Bone formation begins within the first month of treatment • Bone resorption begins after 6 months • During the first year of treatment bone remodelling is in a positive balance. 20mcg Teriparatide daily : • 83% reduction in moderate to severe vertebral fracture in men • 65% reduction in new vertebral fractures in women • 53% reduction in non-vertebral fracture risk Neer et al. Effect of PTH (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med 2001 ,344: 1434 Teriparatide : Effect on Lumbar Spine and Hip BMD in postmenopausal women P< 0.05 Neer et al. Effect of PTH (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis N Engl J Med 2001 ,344: 1434 Teriparatide : (Forteo ) Increases bone mass and improves architecture in ovarectomized monkeys Control Teriparatide Recombinant PTH The changes in BMD seen with PTH are early and of greater magnitude than those seen with other treatment and is therefore plays a role in the treatment of patients with sever established disease who are at particularly high risk of fragility fractures : ►T score ≤ -3.5 without fracture ►T score ≤ -2.5 with fragility fracture ►Any T score with fragility fracture Recombinant PTH • Is well tolerated • Leg cramps & dizziness • It caused an increase in the incidence of osteosarcoma in rats ►Contrindications: Paget,s , Prior bone radiation, Bone metastases, Hypercalcemia ► The safety and efficacy of Teriparatide has not been demonstrated beyond two years ►Teriparatide is used for a maximum of two years , follow with bisphosphonate Agent Doseing & Administration Monthly average cost Alendronate Oral Tab. 70 mg / week $ 87 Ibandronate Oral Tab. 150 mg / month $ 100 Ibandronate IV Injection 3mg /3 month $ 161 Residronate Oral Tab. 150 mg / month $ 100 Zoledronic acid ( Reclast , Zometa ) IV Infusion 5mg / year $ 1315 / year Calcitonin Nasal spray 200 IU/ day $ 126 Estrogen Oral Tab. 0.3 mg / day $ 35 Raloxifen ( Evista ) Oral Tab. 60 mg / day $ 108 Teriparatide ( Forteo) Injection 20 µg /day $ 675 Denosumab ( Prolia ) Injection SC 60 mg/ 6 month Combination therapy • Can provide additional small increase in BMD • The impact of combination therapy on fracture rates is unknown. • The added cost and potential side effects should be weighted against potential gains. Combination therapy Conclusions: •There was no evidence of synergy between parathyroid hormone and Alendronate • Concurrent use of Aendronate may reduce the anabolic effects of parathyroid hormone. • Taken together, these results do not support the concurrent initiation of Alendronate with parathyroid hormone treatment. Strontium Ranelate “Protos” • Act on osteoblasts to increase bone formation • Increases osteoprotegerin which reduces the number and activity of osteoclasts to decrease bone resorption • 41% reduction in vertebral fractures over 3 years • 43% reduction in hip fractures over 5 years • 41-59% fracture risk reduction in patients with osteopenia with or without a prevalent fracture. • Taken 1 satchet daily at bed-time Case discussion CASE DISCUSSION A 56-year-old woman, with an ankle fracture from a fall is seen in the emergency department. She drinks 1 cup of coffee once daily. She had a cardiology evaluation 4 years ago after experiencing rapid heartbeat; results were negative. She has a 2-year history of rheumatoid arthritis (RA). There is no family history of cancer or heart disease. Physical Examination and Laboratory Findings Height: 152 cm Weight: 53 kg BMI: 17.8 kg/m2 HEENT: normal for age BP: 168/100 mm Hg Lungs: normal breath sounds Heart: regular heart rate, no murmurs, rubs, or gallop No jugulovenous distention Abdomen: normal bowel sounds, no guarding, rebound, rigidity, or masses No peripheral edema Current Medications Prednisone 5 mg/d for RA Pravastatin 20 mg/d HRT Q1 • In addition to attending to her ankle fracture, what are the next steps needed for follow-up? A. BMD testing B. Complete blood count (CBC), comprehensive chemistry profile, and vitamin D levels C. Evaluation for possible hyperthyroidism D. Re-evaluation of lipid medication Q1 A. Recommended. BMD testing is recommended for women who experience a fracture after age 40 or 50 and any adult with a fragility fracture B. Recommended. Screening should comprise a complete medical evaluation, which should include gait, balance, and muscle strength testing; assessment of risk factors; BMD evaluation; and assessment of the patient’s ability to understand and comply with treatment intervention. As part of screening, CBC, serum chemistry, urinary calcium excretion, and serum vitamin D levels should be included. C. Recommended. If the practitioner believes there are secondary risk factors for osteoporosis, thyroid levels should be checked. D. Optional. There is no fracture-related reason to re-evaluate statin therapy; however, as part of her medical evaluation, lipid levels should be checked. osteo m 5 3 ultiple Follow-Up Orthopedic Visit On a follow-up visit for her ankle fracture, She says that she missed her BMD testing appointment and has not rescheduled. She has scheduled an appointment with her rheumatologist to discuss changing her arthritis therapy because she did research on the Internet and found that glucocorticoids may decrease her bone density. Q2 What evaluation(s) is appropriate at this time? A. Repeat order for DXA B. Evaluation of fasting lipid profile C. Evaluation for markers of bone formation and breakdown Q2 A. Recommended. She meets the criteria for BMD testing and should be evaluated by DEXA as soon as possible. B. Not recommended. There is no need to re-evaluate her lipids at this time. C. Not recommended. Markers of bone turnover may be predictive of fracture risk reduction after 3 to 6 months of osteoporosis treatment. However, the role of bone markers in osteoporosis and fracture risk management is unclear, as no correlation between changes in bone marker levels and fracture risk has been established. 1 Month Later She returns 1 month later to the orthopedist with results from her DXA. Her T-score is –3.0, indicating osteoporosis . She also reports after consulting with her rheumatologist, the corticosteroids were discontinued and she was started on disease-modifying antirheumatic drugs (DMARD) to treat her RA. Q3 What treatment options may be considered for her steroid-induced osteoporosis? A. FDA-approved bisphosphonate B. Discontinuation of HRT C. Calcium and vitamin D supplementation D. Regular swimming exercises osteo m 6 4 ultiple Q3 A. Recommended. The American College of Rheumatology (ACR) recommends bisphosphonate therapy for individuals with glucocorticoid-induced osteoporosis. B. Recommended. There is no evidence of added benefit in fracture reduction from combining HRT with other osteoporosis medications. Concomitant use is not recommended. C. Recommended. According to the ACR, supplementation with calcium and vitamin D should be recommended for patients treated with glucocorticoids and used in conjunction with bisphosphonates as part of treatment for patients who have had a fracture while receiving HRT.12 D. Not recommended. Although swimming will not hurt the patient, it has no effect on building bone, which requires weight-bearing exercises in which the feet and legs bear the weight, such as walking, jogging, or stair climbing. She walks 2 miles a day, but may benefit from increasing weight-bearing exercise. Follow-up She is prescribed generic alendronate and her other medications are unchanged. 1 year later.... She has suffered a fracture in her wrist and returns to the orthopedist for cast removal. She reports that she discontinued alendronate because it caused stomach upset and she stopped taking HRT on her own 6 months ago when her menopausal symptoms subsided. She remains very thin, with a BMI of 18 kg/m2. osteo 5 m 7 4 ultiple Q4 What are the next steps for her? A. Start an injectable, such as Teriparatide B. Urge her to discuss restarting HRT with her gynecologist C. Recommend hip protectors to prevent hip fracture Q4 A. Recommended. Teriparatide is approved for treatment of osteoporosis in postmenopausal women and has been shown to reduce fracture risk and increase lumbar spine bone mass in that population. It is well tolerated and not associated with stomach upset, which may be good for the patient. B. Not recommended. There is no evidence of added benefit in fracture reduction from combining HRT with other osteoporosis medications. C. Not recommended. Hip protectors have not been shown consistently to reduce the risk of hip fractures and were not effective in reducing fracture risk for adults like Rose, who do not live in nursing care facilities.