* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download ischr
Survey
Document related concepts
Transcript
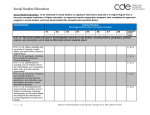
How To Develop & Implement a Practical Staff Competency Plan Pat Comoss RN, BS, MAACVPR Nursing Enrichment Consultants, Inc. Financial Disclosure I have no financial relationships to disclose Staff Competencies in Rehab Upon completion of this activity, participants will be able to: • Discuss why an annual staff competency plan is important for rehab personnel • Identify criteria that are useful when choosing competency topics • List acceptable methods for evaluating a staff member’s competency • Match selected competencies to AACVPR’s published Core Competencies for CR & PR Staff Competencies in Rehab Not New, Revisit WHAT WHY WHEN WHO HOW WHY Staff Competencies Intrinsic Philosophy: desire for continuous learning to be the best rehab practitioner you can be WHY Staff Competencies Intrinsic Philosophy = desire for continuous learning to be the best rehab practitioner you can be Extrinsic Expectation: • Hospital requirement • Joint Commission standard • AACVPR Program Certification criteria WHY Staff Competencies The Joint Commission “Competence assessment lets the hospital know whether its staff have the ability to use specific skills and to employ the knowledge necessary to perform their jobs.” Human Resources chapter: 2015 Hospital Accreditation Standards TJC: Standard HR 01.06.01 The hospital • Defines the competencies it requires of staff who provide patient care/ treatment/services TJC: Standard HR 01.06.01 • Uses assessment methods to determine competence in the skill being assessed Test taking Return demonstration Simulation/role play Observation of actual patient care TJC: Standard HR 01.06.01 An individual with the educational background, experience, or knowledge related to the skills being reviewed assesses competence: • Instructor • Preceptor • Coworker TJC: Standard HR 01.06.01 The hospital can utilize: • An outside individual Such as: guest speaker, consultant • Competency guidelines from an appropriate professional organization Such as: AACVPR Core Competencies TJC: Standard HR 01.06.01 Staff competence is assessed & documented • once every 3 years • or more often per hospital policy WHY Staff Competencies AACVPR Program Certification CR & PR: Requirement #1 = Staff Competencies • Individuals should possess a common core of professional & clinical competencies, regardless of academic discipline WHY Staff Competencies AACVPR Program Certification CR & PR: Requirement #1 = Staff Competencies • A program must provide evidence of annual assessment of clinical/professional staff competency AACVPR Program Certification PULMONARY REHAB Program Certification: Four assessed competencies MUST be specific to Clinical Competency Guidelines for Pulmonary Rehabilitation Professionals 2014 Collins EG, Bauldoff G, Carlin B, et al. JCRP 2014; 34: 291-302 AACVPR Program Certification CARDIAC REHAB Program Certification: Four assessed competencies MUST be specific to Core Competencies for Cardiac Rehabilitation/ Secondary Prevention Professionals: 2010 Update Hamm L, Sanderson B, Ades P, et al JCRP 2011; 31: 2-10 WHAT Staff Competencies Similar Categories for Staff Competencies CR & PR: • Patient Assessment • Exercise Training • Psychosocial Management • Tobacco Cessation • Emergency Planning WHAT Staff Competencies Cardiac Rehab • Blood pressure management • Lipid management • Diabetes management • Weight management Pulmonary Rehab • Dyspnea assessment & management • Oxygen assessment & management • Collaborative selfmanagement WHAT NOT Staff Competencies Discipline-specific hospital/department required competencies: • Cardiology RNs = conscious sedation • Respiratory RTs = precautions to prevent ventilator acquired pneumonia (VAP) WHAT NOT Staff Competencies Initial/Orientation checklist for new employees • often emphasize mechanical functions within dept vs. specific clinical patient care Hospital-wide required competencies • e.g. HIPAA rules, safety/security color-codes, etc. HOW Staff Competencies 1. Choose skills that need to be learned, reviewed, or updated because they are: • • • • NEW/CHANGED HIGH RISK LOW VOLUME PROBLEMATIC HOW Staff Competencies • • • • • • Categories Patient Assessment Exercise Training Psychosocial Management Tobacco Cessation Emergency Planning Etc. Criteria • NEW/CHANGED • HIGH RISK • LOW VOLUME • PROBLEMATIC HOW Staff Competencies 2. Sources of choices: INSIDE - OUT Use Core Competency documents for staff self-assessment = Identify strengths & weaknesses HOW: Inside - Out Examples • NEW = BODE Index calculation (PR), MET-minutes calculation (CR) • HIGH RISK = diabetic exercise management (blood sugar testing, high & low cut-offs) • LOW VOLUME = tobacco cessation HOW Staff Competencies Cross reference to Core = Smoking Cessation • Core Competencies for Cardiac Rehabilitation/Secondary Prevention Professionals: 2010 Update – pg 7 Tobacco cessation; Knowledge 1-7, Skills 1-3. • Pulmonary Clinical Competency Guidelines: 2014 Update - pg. 299, Tobacco cessation; Knowledge 1-7, Skills 1-2. HOW: Inside - Out Challenge: find resources to teach the topic/skill to rehab staff in rehab context • Within facility or external expert? • PROFESSIONAL DEVELOPMENT OPPORTUNITY = elect a staff member to study/research the topic & become the rehab expert Competency: Tobacco Cessation Counseling Name _______________________ Date ______ Dept. Cardiac Rehab Pulmonary Rehab Expectation: To provide effective counseling to help those patients who wish to quit smoking do so during the course of rehab. Essential Elements of Performance: 1 2 3 4 5 6 7 Proficient Needs Review/ Improvement Inadequate ** Explain the impact of continued smoking on cardiac/pulmonary disease & the benefits of quitting now. Recognize smoking status as a routine outcome measure & point-out questions in both admission & discharge interviews that collect that information Discuss recent alternatives to cigarette smoking, e.g. e-cigarettes, hookah, vaping At the beginning of rehab, assess each smoker for readiness to change their smoking behavior & reassess their stage every 30 days during rehab Use appropriate counseling strategies & resources for each stage of readiness List common medications used to assist smoking cessation, including nicotine replacement & psychotherapeutics, & provide related information about each to patients Identify outside resources Hospital Tobacco Counselor Community cessation programs Help line by phone or internet that can be tapped for additional help during rehab or follow-up after rehab Resources: For knowledge AACVPR PR Guidelines (new 4th edition) section on Smoking Cessation, pgs. 60-64 AACVPR CR Guidelines, 5th ed., chapter 8 Modifiable Risk Factors, pgs. 90-94 US Dept. of Health, Treating Tobacco Use & Dependence Krames patient workbooks For skills Workshop with hospital Tobacco Counselor to emphasize: a. assessing readiness to change b. teaching prescribed medication use HOW Staff Competencies 2. Source of choices: OUTSIDE - IN Use authoritative external information for competency ideas = Identify need to update/upgrade program HOW: Outside - In Challenge: make sure chosen topic/skill is within the scope of Core Competencies expectations • Where does the new interest match document? • PROFESSIONAL DEVELOPMENT OPPORTUNITY = elect a staff member to track connections between chosen topics & competency bullets Pulmonary Rehab Example NEW/CHANGED: Need to update PR policy & practice to incorporate latest evidence-based recommendations for this important outcome measure Pulmonary Rehab Example Changes to 6MWT Performance 2015: • For initial assessment, do 2 walks & take best result as baseline measure • Use patient's own oxygen equipment & usual O2 flow = DO NOT TITRATE O2 • Allow O2 sat to drop to low value cut-off of 80% saturation • For exit evaluation, look for change of at least 30 meters/100 feet to be clinically significant Pulmonary Rehab Example Exercise Testing p.298 Use of field testing (6MWT, shuttle walk) as outcome measure • Complete 6MWT using ATS criteria • Appropriately monitor responses • Develop ExRx on basis of results as appropriate Competency: Six Minute Walk Test (6MWT) as a Measure of Functional Capacity in Outpatient Pulmonary Rehab Patients Name _____________________________ Department: __Pulmonary Rehab____ Expectation: The pulmonary rehab therapist will demonstrate correct methods of preparing, instructing, performing, and documenting the walk test as a pulmonary rehab clinical outcome measurement. Critical Elements: Proficient 1 2 3 4 5 The PR therapist will be able to: PRE 6MWT Recognize the 6MWT as a submaximal exercise testing procedure Identify appropriate patients to participate, following policy for indications & contraindications Communicate advance instructions to patient by phone or mail: Wear walking shoes Bring usual walking aids Bring own oxygen equipment Take usual meds at usual times Prepare for possible emergencies during the test: Location of crash/cart/defibrillator Availability of supervising physician Access to emergency medications = albuterol, nitrogylycerin, oxygen Means of calling for help Set-up space & equipment in advance: Flat unimpeded walking path, ideally 100 linear feet Cones to mark ends of walking path Chairs for patient to stop if needed Stop-watch or other timer Borg 0-10 scale for rating both RPD & fatigue Clipboard with script of patient instructions & report form to record laps & responses B/P cuff & stethoscope Wearable oximeter Telemetry monitoring = optional Needs Review/ Improvement Inadequate ** 6 7 8 9 10 11 12 13 14 15 Plan for patient to use own devices during test performance = walking aids, oxygen equipment If using oxygen, maintain usual flow rate & keep constant during test = DO NOT TITRATE Identify one exception for applying oxygen during test if not used routinely = if patient desaturates to 85% or less on room air after 10 min rest Position patient in a chair near start of walking path to: Relax & breathe quietly 5-10 minutes Confirm that usual meds were taken & that oxygen is set at usual levels Attach oximeter to provide continuous O2 sat data during walk No warm-up is needed DURING 6MWT Discuss the importance of following a standardized procedure for test performance for test to help assure reproducibility Perform pre-test measurements: Heart rate, BP, & O2 saturation Dyspnea level & fatigue level (Borg 0-10) Explain that this is a self-paced walking test for the purpose of seeing HOW FAR a person can walk in 6 minutes time Read ATS scripted instructions to each patient for each test Demonstrate correct walking technique such as: Where to walk out & back How to go around cones without slowing down And so on Select a mid-point along the path to stand for best observation & coaching, including visualization of oximeter data as patient passes by Give rationale for NOT walking with patient, unless there is a safety issue or fall risk = if needed, walk behind patient to not influence their pace 16. 17 18 19 20 21 22 23 24 25 26 Provide scripted instructions every 1 minute during test = DO NOT use other words of encouragement Allow patient to stop & rest if needed = lean against wall or sit down, but clock keeps ticking When stops occur, use scripted instruction every 30 seconds to “please resume walking whenever you feel able” Note time stopped & when restarted Monitor O2 sat & HR each time patient passes therapist’s position Without interrupting walking pace, have patient hold up hand to see oximeter data when passing by React immediately to stop test if/when O2 sat drops to 80% or less = new cutoff value As 6 minute endpoint approaches, warn patient that “time is almost up, when I say STOP, please stop where you are & I will come to you”. At 6 minutes, go to patient’s side to: Obtain HR & O2 sat data Take blood pressure Ask RPD & fatigue ratings Ask why they could not walk any farther POST 6MWT Have patient sit in chair & relax for 510 minutes Complete test documentation including Total distance walked Number & length of stops Lowest O2 sat & highest RPD observed during test Signs/symptoms reported Reason could not go farther Translate total distance walked into mph & METs to help with starting exercise training on the treadmill At entry walk, continue with other admission assessments & repeat walk at end of visit (at least 30 minutes later) 27 Explain that rationale for 2nd walk test ton same day is to allow for patient’s learning curve & provide opportunity for improvement in performance Use best result (longest distance) of 2 initial tests as outcome data 28 Describe 2 types of exceptions to repeating the walk test a second time: Patient who does quite well the first time = unlikely to do better Patient who is quite sick & struggles to complete first walk = unable to walk again 29 At exit walk, compare results to entry walk data & explain extent of change to patient Explain that rationale for only 1 walk at exit is because patent is now familiar with the 6MWT procedure State that a clinically significant change from entry to exit test is 30 meters/100 feet = the minimal important difference (MID) to indicate functional improvement as a result of rehab 30 31 Resources: For knowledge ATS/ERS Technical Standard: Field walking tests in chronic respiratory disease; European Respiratory Journal, 44:6; December 2014; 14281446. For skills Instruction/demonstration session by an RT experienced in 6’ walk studies Practice & return demonstration to each other Observation of an actual test on a PR patient Cross-reference to: AACVPR Clinical Competency Guidelines for Pulmonary Rehabilitation Professionals. JCRP 2014; pg 298, Exercise Testing: Knowledge bullets 1-5 & Skills bullets1 & 4. Evaluation: Signature _______________________________ Date ________________ ** any/all ratings of Inadequate require a corrective action plan tailored to the staff member involved Cardiac Rehab Example NEW/CHANGED: Need to update CR policy & practice to incorporate latest evidence-based recommendations for this important outcome measure Cardiac Rehab Example Changes to BP Management 2015: • New target value for secondary prevention of cardiac events = 140/90mmHg • Much lower is not necessarily better & may contribute to side effects or complications • Decreased coronary or cerebral perfusion • Orthostatic problems • DBP less than 65mmHg should be avoided in older patients Cardiac Rehab Example BP Management p.6 Normal range of BP at rest & with exercise; Current BP targets for secondary prevention • • • Accurate determinations Recognition of deviations from range Measurement of outcomes Competency: The Role of Cardiac Rehab in Managing Hypertension Name _______________________ Date ______ Dept. Cardiac Rehab Expectation: The cardiac rehab staff will monitor patients’ blood pressure at rest & during exercise and compare findings to current treatment recommendations & evidencebased goals for managing hypertension Essential Elements of Performance The cardiac rehab staff will be able to: 1 2 3 4 5 6 7 8 9 Define current blood pressure(B/P) values for: Normal B/P < 120/80 mmHg Pre-hypertension = 120-139/80/89 mmHg Hypertension > 140/90 mmHg Describe the underlying pathophysiology of hypertension as endothelial dysfunction inhibiting arterial ability to dilate & constrict Identify the new “reasonable” BP goal for secondary prevention of cardiovascular events as less than 140/90 mmHg for most patients Emphasize that the new goal also applies to cardiac patients with heart failure, kidney failure, & diabetes. Explain the rationale for the new goal number as based on evidence that less than 130/80 does not change morbidity or mortality outcomes in CAD patients Discuss the concerns that lower BP goals may have contributed to: Decreased coronary & cerebral perfusion Increased orthostatic side effects Recognize that some patients may benefit from a goal of 130/80 or less, such as those with: Stroke/TIA Abdominal aneurysm Selected MI patients Monitor patients for low DBP since less than 65 mmHg has been linked to an increase in orthostatic-related complications in older patients List treatment priorities recommended in the 2015 evidence-based document on hypertension management as: Lifestyle management Proficient Needs Review/ Improvement Inadequate ** 10 11 12 13 14 15 16 17 18 Outline the role of cardiac rehab in hypertension treatment as providing lifestyle management education & counseling for hypertensive cardiac patients, including: Diet management Sodium reduction Physical activity advice Recommend the DASH diet as the eating pattern of choice to help control hypertension & list its major components as: Non-fat dairy products Poultry, fish, legumes Monounsaturated oils & spreads Nuts (walnuts, almonds, hazelnuts) State the recommended sodium intake for patients with hypertension as 1500-2400 mg per day Identify the physical activity goal for all cardiovascular patients including those with hypertension as: Minimal = 150 minutes per week of moderate activity/exercise Optimal = 500-1000 MET-minutes per week Explain that the combination of healthy eating & regular exercise that has been shown to have the biggest impact on B/P lowering includes: Dash diet Low sodium Weight loss List the top 3 classes of drugs recommended for pharmacologic management of hypertension as: Diuretics Beta-blockers ACE inhibitors/ARB Reinforce the importance of medication compliance & provide patients with ideas & techniques, e.g. pill boxes, to help improve compliance Change the target goal number for B/P in your program’s outcome data documents to the new recommendation of less than 140/90 mmHg Monitor your outcome data to determine how many patients achieve the new goal in 2015 Resources: For Recommendations AHA/ACC/ASH Scientific Statement: Treatment of Hypertension in Patients with Coronary Artery Disease. Circulation, May 12, 2015. For Reinforcement Staff meeting with Medical Director to discuss the new guidelines & their application in the cardiac rehab setting Cross-reference to Cardiac Rehab Core Competencies: AACVPR Core Competencies for Cardiac Rehab, 2010: page 6 Blood Pressure Management; Knowledge bullets 3-4, 10-11; Skill bullets 3-4. Evaluation: Signature _______________________________ Date ________________ ** any/all ratings of Inadequate require a corrective action plan tailored to the staff member involved HOW Staff Competencies WHAT WHY WHEN HOW WHO WHEN Staff Competencies Schedule an in-service presentation and/or practice session • Annually • Quarterly GOOD PEOPLE HOSPITAL 2015 Staff Competency Plan Outpatient Cardiac Rehab Program Topic1 Rationale2 1st q Exercising LVAD Patients LOW VOLUME: A growing number of heart failure patients are being treated with Left ventricular Assist Devices (LVAD) Rehab staff need to understand the purpose & potential of LVAD devices Familiarity with device safety features, alarms, batteries, etc. & how to respond to each is essential to patient care in rehab Strength Training Calculating total exercise volume Assessing readiness to change risk factors Notes: Schedule3 2nd q 3rd q 4th q X Adjustment of assessment & exercise guidelines, e.g. no BP or pulse checks, is required for this special population HIGH RISK: Strength/resistance training is an increasingly common element of a rehab exercise program Proper patient selection maximizes patient safety Proper performance minimizes side effects/injuries Program policies need to reflect national guidelines and be consistently followed to avoid patient complications NEW: Evidence-based recommendations show that optimal exercise benefits accrue to patients who perform a total volume of 500-1000 MET-minutes of exercise per week That volume is comprised of both in rehab & outside exercise MET tables enable combining those exercises All staff should know how to compute that exercise volume data PROBLEMATIC: All patients are not ready to change all risk factors just because they are now in rehab Staff needs to know how to determine if, when, & what a patient is ready to change The trans-theoretical model (TTM) of readiness to change provides a practical means of determining readiness that can be integrated into initial & ongoing patient assessments Staff responsible for patient assessment need to implement the stages of change questions X 1. Each topic requires a cognitive component (new knowledge) and a performance (new skill) component. Learning packets that include an article, sample policy, etc. and a skills checklist are developed for each topic and completed by each staff member. 2. Topics selected by the staff are important aspects of care that are high risk, low frequency, problem-prone, or new. 3. Completion of each competency includes review/revision (or original development) of the corresponding program policy, treatment protocol, or chart form. X X Staff Competencies: SUMMARY • WHAT = documentation of staff knowledge, skill, & ability • WHY = improve quality of program; requirement for TJC & AACVPR • WHEN = 4 each year for cert/recert • HOW = learn, practice, demonstrate, document • WHO = staff member, outside expert Cardiac Rehab - SPECIAL NOTE Core Competency document is basis for new CCRP certification! Professional certification exam to be given at this AACVPR National Meeting: September 7, 2016 New Orleans, LA Pulmonary Rehab – PREVIEW PR Core Competency document will be basis for new CPRP certification! Now in development!! References Hamm LF et al. Core Competencies for Cardiac Rehabilitation Professionals: 2010 Update. JCRP 2011;31: 2-10. Collins EG et al. Clinical Competency Guidelines for Pulmonary Rehabilitation Professionals. JCRP 2014; 34: 291-302. References Holland AE et al. An official European Respiratory Society/ American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J 2014; 44: 1428-1446. Rosendorff C et al. Treatment of Hypertension in Patients with Coronary Artery Disease. Circulation 2015; 131: e1 – e36. Staff Competencies in Rehab Thank You! Good luck with planning & documenting your program’s staff competencies!! [email protected] Staff Competencies in Rehab Q&A ? ? ?