* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Midcycle OSCE
Survey
Document related concepts
Transcript
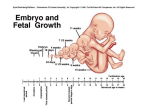
425 OSCE slide show By: 425 people =D Hi everyone =D Welcome everyone =) This is a 425 OB/GYN slide show exam, most of the pictures here were the exact pictures showed in exam, some were almost the same. I’m ganna put (*) next to pictures that were the exact ones. The answers here were my answers in exam, so there is a chance to be wrong, so please tell others whenever there is a mistake and feel free to edit the slides. And for the next groups in 425, feel super free to add your slide show exam to this slides right after our exam with your beautiful names for years after us =) thanks a LOT guys. And BIG FAT good luck to you all. 425 Female midcycle Slide Show Exam Slide 1 Qs: 1. 2. 3. What is this procedure? Name 4 indications for this procedure. Name 2 other antenatal diagnostic tests. 1. 2. Amniocentesis. Chromosomal abnormality (cells) Infections Bilirubin (in case of haemolysis) Check lung maturity. 3. Name other 2 antenatal diagnostic tests. PUBS (percutanous umbilical cord blood sampling) CVS (Chorionic villia sampling) Slide 2 Qs: What is this condition? Name 4 causes. Which of them has highest dangerous complications. And why? Name 2 complications you would anticipate. 1. 2. Macrosomic baby Diabetic mother (GDM or pre-existing) Post date Family history of big babies Undiagnosed DM Obese mothers. Gaining a lot of weight during pregnency. 3.Diabetic mother, because it is associated with fetal poor health and delayed lung maturity and respiratory distress. 4.Complications: Polycythemia, hypoglycemia, hyperbilirubinemia, delayed lung maturity, shoulder dystotia, prolonged labour and risk of fetal distress. Slide 3 * Qs: Identify the defect in arrow 1. Identify the anatomic structure in: (1, 2, 3, 4 ). Name 3 risk factors for this condition. Cystocele. 2. 1= urinary bladder wall, anterior vaginal wall. 2=rectum 3=uterus 4=urinarry bladder 3. multiparty, old age, genetic connective tissue weakness, previous injury 1. Slide 4 * Qs: What is the defect in arrow 3? What is the position of this uterus? Identify instruments in arrow (1, 2). How can you prevent this condition. 1. 2. 3. 4. Perforated uterus. Sharply anteflexed uterus. (1=Sim’s uterine sound, 2=metallic vaginal speculum ). 1.US-guided procedure 2.Gentle and gradual insertion. Slide 5 * Qs: 1. 2. 3. 4. Name this organism. How would it present clinically? What is the treatment? Would you treat the partner? Why? 1. 2. 3. 4. Trichomonus vaginalis. It could present with itching and discharge. Treat with metronidazole. Yes treat the husband, because it is infectious sexually transmitted disease. Slide 6 Qs: Identify Name three indications. Name three complications 1. 2. Plastic ventous suction cup Indications: Prolonged labour maternal exhaustion Fetal distress Maternal medical illness. 3. Complications: Epidural , cephalic haematoma. Hyperbilirobinemia Birth canal injury due to tissue entrapment. Prolonged suction causes fetal distress. Slide 7 Qs: 1. 2. 3. Identify the abnormality. What is the normal range? Name 4 causes. 1. Fetal tachycardia. (>180 beats/mint) 2.120-160 beats/mint 3.CAUSES of fetal tachycardia Maternal: Fever, Anxiety, medications (ex: terbutaline) Fetal: Infection, excitation and movement, early hypoxia, infection, fetal heart arrhythmia and prematurity. Slide 8 * Qs: 1. Name the 4 hormones in menstrual cycle and from where are they secreted? 2. Name the two phases and their predominant hormone. 1. FSH……………..from anterior pituitary LH ………………from anterior pituitary Oestrogen………from granulosa cells Progesterone….. from corpus luteum 2. Proliferative phase (by estrogen) secretary phase-luteal- (by progesterone) Slide 9 Qs: 1. 2. 3. What is shown in the picture? Name 4 common sites for this lesions. What are the two main ways of treatment? mention an example for each. 1.Endometriosis (shown by laproscope) 2.Common sites: Ovaries Peritoneum Ovarian/uterine ligaments Pelvic wall cervical 3.treatment 1.Medical: Pseudopregnency: progesterone pills, OCPs. Pseudomenopause: danazole, GnRH agonists. 2.Surgical: Partial or radical either by :Laproscopy or laprotomy Slide 10 * Qs: 1. 2. 3. 4. What is the lie and presentation? Name two diagnostic signs. Name two complications. What is the management: Before delivery? During labour? 1.Transverse lie, shoulder presentation. 2.Signs: low fundal hight to date, feel the head on abdominal lateral sides, feel the back of the fetus running transverse lie, transverse lie by US. 3.Complications: cord prolapse (Most common), cord compression, shoulder dystocia, prolonged labour, fetal distress, maternal exhaustion, fetal injury, bone fracture, maternal injury and obstructed labour. 4. management 1.Before delivery: External cephalic version. 2.Intra labour: C/S Special thanx to: Addana alsaad Aljowhara alameer For squeezing their brains to remember Qs =D :hearts: 425 Female Final Slide Show Exam Slide 1 Qs 1. 2. 3. 4. What do you see? Give two DDx. What would you ask in Hx. (give 3) What would you order for investigation. (give 3) 1. 2. What do you see? Breast budding. Give 2 DDx. Complete precocious puberty. Incomplete precocious puberty 1. 2. 3. 4. What would you ask in Hx? Ask if she has any pubic or axillary hair? Ask if she had any vaginal bleeding or menses. Ask if she has been taking any medications Ask for any family Hx in this condition. 1. 2. 3. 4. What would you order for investigation? Check hormonal level of estrogen. Check her FSH, LH levels. Take radio-images of her brain to rule out any secretery tumors (sp: pituitary) Do an US for her ovaries to rule out any estrogen secreting tumors (ex: granulosal cells tumor) Slide 2 * Qs 1. 2. 3. 4. 5. What is this condition? Caused by which hormone? What could cause it elevation? What other posible symptoms could it present with? How would you treat it? What is it? Galactorrhea By which hormone? Prolactin What could cause its elevation? (give 4) Physiological (lactating breast-feeding mother) Pituitary adenoma Drug-induced. Other prolactin-secretory tumors. Idiopathic elevation. Possible other symptoms: give 2 Infertility Amenorrhea How would you treat? Medically: bromocreptine (for decreasing prolactin secretion and reducing adenomas size), clomid (to restore fertility) Surgical: remove the tumor Slide 3 Qs 1. 2. 3. 4. 5. What is it? Used for what? What are the indications for its job? Who uses it? Name to complication. What? An amniotic hook (or an amniohook) Used for what? For artificial rupture of membranes (or amniotomy) 1. 2. 3. What are the indication? Used in induction of labor (to fasten baby birth due to any reason) Used to see muconium-stained amniotic fluid to confirm fetal distress (in an external fetal monitor) Used to put on fetal scalp heart monitor to confirm fetal distress in an external monitor. Who uses it? An obstetrician and a midwife. Name 3 complications: Bleeding. Injury to the baby’s presenting part. Infection. Slide 4 Pt presents with 6 week of amenorrhea and lower abdominal pain (look at picture) Qs What is the Dx? What possible other symptoms? Give 4 risk factors. How would you treat? What is the Dx? Ectopic pregnancy. What possible other symptoms? PV bleeding, lower abdominal pain and amenorrhea Give 4 risk factors. Previous Ectopic pregnancy Tubal disease Chronic PID and adhesions. Adhesions from endometriosis IUCD Tubal ligation How would you manage? Medical: methotrexate if it fits the recommended criteria. Surgical: salpingostomy (if in ampulla and uncomplicated) salpingectomy if otherwise with checking the patency and health of the other tube. Slide 5 Qs 1. 2. 3. What are 1, 2 ,3 ? Which one is the most important obstetrically and what’s its length? What are 4 and 5? What are 1, 2 and 3? 1= True (anatomic) diameter. 2=obstetric diameter. 3=diagonal diameter. Which is obs. Imp and what’s its length? Obstetric diameter and its about 11.5 cm 1. What are 4 and 5? 4=pubic bone (symphesis pubis) 5=sacral promontory. Slide 6 Qs 1. 2. 3. 4. What is your Dx? What symptoms would present (give 2) What hormones would be elevated? How would you treat? What is the Dx? Polycystic ovarian syndrome (PCOs) Symptoms: Acne Hiristisum Infertility Irregular menses 1. 2. 3. What hormones would be elevated? (Give2) LH Androgens Insulin How would you treat? Give combined OCPs (for hiristisum and prevention of endometrial cancer due to elevated unopposed estrogen Or give progestrone to prevent endometrial cancer Give metformin for insulin resistance. Remove ovary surgically if associated with neoplasm or unreasoning to medications. Slide 7 * Qs 1. 2. 3. 4. What is this condition? How to detect it antenatally? Name 3 complications. How would you prevent it? What? Anencephaly How would you prevent it? By folic acid supplementation in diet. Name 3 complications: 1.malpresenation 2.post date 3.polyhydrominous. 4.postpartum haemorrhage (uterine atony) 5.baby loss (depression) How to detect? 1.US: absent brain and skull bones. 2 triple marker test : elevated alphafetoprotein. 3.by physical exam: cant palpate the fetal head. Slide 8 * Qs 1. 2. 3. What is this condition? What could cause this condition? Name 3 complications of forceps delivery. What? Facial palsy. What could cause it? Operative delivery by forceps. Name 3 other obstetric and 3 fetal complications of forceps: Fetal: Fetal skull bone fractures. Intracranial hematomas. Intracranial haemorrhage. Low apgar score Fetal distress. Maternal: Birth canal injury. Post partum haemorrhage. Fistulae formation. Bladder, urethral and perineal body injury Urine incontinence. Slide 9 Qs What are 1 and 2? Name 4 indications for C/S. Name 4 complications for C/S. What are 1 and 2? 1= vertical (longtudinal) section (classic) 2= low transverse section. Name 4 indications. 1. Placenta prevea. 2. Preveious myomectomy 3. Previous C/S 4. Previous uterine rupture 5. Conditions need to deliver baby as fast as possible with the cervix is unfavourable like: A-Severe pre-eclampsia B-Eclampsia. C-Severe fetal distress. Name 4 complications: Heavy bleeding. risk of uterine rupture in a subsequent pregnancy. Higher risk for infections and puerperal sepses. Urine overflow incontinence (from anaesthetics) Risk of fetal injury (from cutting the uterus) Injury of other pelvic organ tissues. Slide 10 Missing picture =D In last Q (Q10), we had a case and a picture: The case was: postpartum patient, in day 4 with tender well contracted uterus. BUT unfortunately we don’t have the picture of it :$, It was a nurse chart :S It was so easy , so no need to freak out =D It clearly showed a temp of 38.5, HR: 120 and the word Heavy in the lochia column of the chart, and the Qs were as follows : Qs 1. 2. 3. 4. What do you see in the patient’s chart? What is the possible Dx? What investigations would you do? What general management would you do? What do you see in chart? Chart shows: fever, tachycardia and persisting heavy lochia (bleeding) What is the possible Dx? Secondary postpartum hemorrahge from retaind tissue and puerperal fever. What is most probably caused fever? Endometritis. What investigations would you do? (give3) US: to rule out retained placental tissue. CBC: for dropping Hb and leukocytosis. Culture of endometrial tissue and lochia to identify the causing organism. (not routinely done). General management? (give3) IV fluids (dehydration from fever). Antipyretics. Broad spectrum Abx. Analgesics. D&C to clear from retained tissue. The End Good luck Allergy =D