* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download REVIEW - Ebsco
Survey
Document related concepts
Transcript
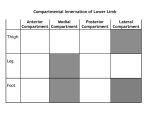
CLINICAL REVIEW Compartment Syndrome, Chronic Indexing Metadata/Description › Title/condition: Compartment Syndrome, Chronic › Synonyms: Chronic exertional compartment syndrome; exercise-induced compartment syndrome; recurrent compartment syndrome; subacute compartment syndrome; chronic exertional compartment syndrome; compartment syndrome, chronic exertional; compartment syndrome, exercise-induced; compartment syndrome, recurrent; chronic compartment syndrome › Anatomical location/body part affected: Most often affects the lower leg, especially the anterior and lateral compartments,(35) but can affect all compartments, including gluteus, foot, shoulder, hand(35), upper leg, and forearm(1) › Area(s) of specialty: Orthopedic rehabilitation, sports rehabilitation, cardiovascular rehabilitation › Description • Compartment syndrome – “A condition in which the circulation and function of tissues within a closed space are compromised by increased pressure within that space”(2) • There are two types of compartment syndrome, acute and chronic. Acute compartment syndrome is a surgical emergency;(2) please see Clinical Review…Compartment Syndrome, Acute; Item Number: T708485 for details • Chronic compartment syndrome– A reversible rise in tissue pressure to abnormal levels brought on by exertion and relieved by rest that occurs within an enclosed space and has the potential to threaten perfusion and tissue viability(2) • The prevalence of chronic compartment syndrome is not known since it is not uncommon for patients to administer self-directed treatment or activity modification and not seek medical attention(32) • 95% of all chronic compartment syndrome cases affect the leg(32) Authors Ellenore Palmer, BScPT, MSc Cinahl Information Systems, Glendale, CA Andrea Callanen, MPT Cinahl Information Systems, Glendale, CA Reviewers Andrea Callanen, MPT Cinahl Information Systems, Glendale, CA Abigail Grover Snook, PT, MS, MEd Cinahl Information Systems, Glendale, CA Rehabilitation Operations Council Glendale Adventist Medical Center, Glendale, CA Editor Sharon Richman, MSPT Cinahl Information Systems, Glendale, CA January 8, 2016 › ICD-9 codes • 729.7 nontraumatic compartment syndrome • 729.71 nontraumatic compartment syndrome of upper extremity: nontraumatic compartment syndrome of shoulder, arm, forearm, wrist, hand, and fingers • 729.72 nontraumatic compartment syndrome of lower extremity: nontraumatic compartment syndrome of hip, buttock, thigh, leg, foot, and toes • 958.90 compartment syndrome, unspecified • ICD codes are provided for the reader’s reference, not for billing purposes › ICD-10 codes • M62.2 ischemic infarction of muscle (non-traumatic compartment syndrome) • ICD codes are provided for the reader’s reference, not for billing purposes › G-Codes • Mobility G-code set –G8978, Mobility: walking & moving around functional limitation, current status, at therapy episode outset and at reporting intervals –G8979, Mobility: walking & moving around functional limitation; projected goal status, at therapy episode outset, at reporting intervals, and at discharge or to end reporting Published by Cinahl Information Systems, a division of EBSCO Information Services. Copyright©2016, Cinahl Information Systems. All rights reserved. No part of this may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the publisher. Cinahl Information Systems accepts no liability for advice or information given herein or errors/omissions in the text. It is merely intended as a general informational overview of the subject for the healthcare professional. Cinahl Information Systems, 1509 Wilson Terrace, Glendale, CA 91206 –G8980, Mobility: walking & moving around functional limitation, discharge status, at discharge from therapy or to end reporting • Changing & Maintaining Body Position G-code set –G8981, Changing & maintaining body position functional limitation, current status, at therapy episode outset and at reporting intervals –G8982, Changing & maintaining body position functional limitation, projected goal status, at therapy episode outset , at reporting intervals, and at discharge or to end reporting –G8983, Changing & maintaining body position functional limitation, discharge status, at discharge from therapy or to end reporting • Carrying, Moving & Handling Objects G-code set –G8984, Carrying, moving & handling objects functional limitation, current status, at therapy episode outset and at reporting intervals –G8985, Carrying, moving & handling objects functional limitation, projected goal status, at therapy episode outset, at reporting intervals, and at discharge or to end reporting –G8986, Carrying, moving & handling objects functional limitation, discharge status, at discharge from therapy or to end reporting • Self Care G-code set –G8987, Self care functional limitation, current status, at therapy episode outset and at reporting intervals –G8988, Self care functional limitation, projected goal status, at therapy episode outset, at reporting intervals, and at discharge or to end reporting –G8989, Self care functional limitation, discharge status, at discharge from therapy or to end reporting • Other PT/OT Primary G-code set –G8990, Other physical or occupational primary functional limitation, current status, at therapy episode outset and at reporting intervals –G8991, Other physical or occupational primary functional limitation, projected goal status, at therapy episode outset, at reporting intervals, and at discharge or to end reporting –G8992, Other physical or occupational primary functional limitation, discharge status, at discharge from therapy or to end reporting • Other PT/OT Subsequent G-code set –G8993, Other physical or occupational subsequent functional limitation, current status, at therapy episode outset and at reporting intervals –G8994, Other physical or occupational subsequent functional limitation, projected goal status, at therapy episode outset, at reporting intervals, and at discharge or to end reporting –G8995, Other physical or occupational subsequent functional limitation, discharge status, at discharge from therapy or to end reporting ›. G-code Modifier Impairment Limitation Restriction CH 0 percent impaired, limited or restricted CI At least 1 percent but less than 20 percent impaired, limited or restricted CJ At least 20 percent but less than 40 percent impaired, limited or restricted CK At least 40 percent but less than 60 percent impaired, limited or restricted CL At least 60 percent but less than 80 percent impaired, limited or restricted CM At least 80 percent but less than 100 percent impaired, limited or restricted CN 100 percent impaired, limited or restricted Source: http://www.cms.gov . › Reimbursement: No specific issues or information regarding reimbursement have been identified › Presentation/signs and symptoms • Presentation – there is a variety of different presentations(39) –Gradual onset of symptoms(3,4) –Patients typically present with a long duration of preexisting symptoms(32) –Symptoms frequently occur during repetitious movements (e.g., jogging, biking) and will cease once activity stops(3,5,25) –Over time, a low-intensity ache may persist even when activity has ceased(3) –Typically occurs bilaterally and at the same point (duration/intensity) during exercise(6) –Most often affects the lower leg compartments(1) - Anterior compartment – most often affected - 95% of cases occur in anterior compartment(40) - Lateral compartment - Superficial posterior compartment - Deep posterior compartment –Also reported in the thigh, forearm, and foot(27) - Thigh contains 3 compartments: anterior, posterior, and medial - Forearm contains 2 compartments: anterior and posterior - Foot contains the medial, lateral, superficial, and deep compartments –Signs/symptoms - Pain during exercise at a predictable point that resolves with cessation of activity(7) - Pain gradually intensifies to be severe enough to prevent the individual from continuing activity such as running or walking(26) - Mild weakness or tenderness of muscle group of impaired compartment(7) - Soft tissue within the affected compartment feels tense/tight(27) - Physical examination is asymptomatic at rest(7) - Burning, cramping, and aching over involved compartment during and immediately following exertion(4,6) - Paresthesia (e.g., numbness, tingling) corresponding to the nerve within the affected compartment during aggravating activity(3,4,27) - Paresthesia occurs over the dorsal aspect of the foot if the anterior compartment is affected(27) - Paresthesia occurs on the plantar aspect of the foot if the deep compartment is affected(27) Causes, Pathogenesis, & Risk Factors › Causes • Result of increased or prolonged exertion (exercise) that leads to elevated pressure in the involved compartment(2,4) • Other potential causative factors(2,4) –Sudden escalation in training –Alteration in type of surface practiced/trained on –New footwear –Faulty biomechanics › Pathogenesis • The pathophysiology is not fully understood. Hypotheses include the following: –Muscle volume normally increases during exercise; however, in chronic compartment syndrome, the osseofascial compartment is unable to accommodate to the increase in size associated with muscle contraction and swelling. The increased volume increases intracompartmental pressure and reduces perfusion of the tissues within the fascial compartment and ischemia results. The ischemia leads to pain, discomfort, paresthesia, and metabolite accumulation(1,27) –Muscle that has been injured through repetitious activity on an inflexible surface secretes protein-bound ions, thereby altering osmotic pressure. In turn, swelling increases, resulting in inadequate blood flow to the region(8) –Fluid extravasation (leakage into tissue) and increased intracompartmental pressures may contribute to neural compression(32) –Decreased capillary density or obstructed venous outflow have also been implicated in the development of chronic compartment syndrome(32) • Unresolved questions about the pathophysiology of chronic compartment syndrome include(39) –why the pain remits immediately after cessation of activity whereas in acute skeletal muscle compartment syndrome it persists, even though swelling and ischemia is the predominant pathology in both conditions –why unilateral presentations occur even though both lower extremities would be expected to have similar levels of exertion, and thus a similar amount of swelling and ischemia for most triggering activities › Risk factors • Prolonged or high-performance athletics/physical training(4,8) –Runners and endurance athletes have a higher risk than sedentary populations or those who engage in upper extremity dominant sports(27) –Chronic compartment syndrome in the forearm can occur in gymnasts and climbers,(27) and musicians(41) - In a study in Italy the highest incidence of chronic compartment syndrome in the forearm was found in professional motorcycle drivers(41) –Runners and aerobic trainers can getchronic compartment syndrome in the foot(27) • Military recruits are at increased risk for developing chronic compartment syndrome(8) –United States researchers conducted a cohort study on enlisted service members in the U.S. ground military forces to determine incidence rates of chronic compartment syndrome in this population because of exposure to at-risk dismounted activity (i.e., operations conducted on foot) on the battlefield and in training(31) - 4,100 individuals were diagnosed with chronic compartment syndrome between 2006 and 2011 within an at-risk population of 8,320,201. This correlates to an incidence rate of 0.49 cases per 1,000 per year - Increasing chronological age, female sex, white race, junior enlisted rank, and Army service were significantly correlated with an elevated risk for chronic compartment syndrome –Anabolic steroid and creatine supplement use(38) - Increases muscle volume Overall Contraindications/Precautions › Acute compartment syndrome may result if the patient does not receive proper intervention. Acute compartment syndrome is a medical emergency;(1) please see Clinical Review… Compartment Syndrome, Acute, referenced above, for details › See specific Contraindications/precautions to examination and Contraindications/precautions under Assessment/ Plan of Care Examination › Contraindications/precautions to examination • If during the course of evaluation a diagnosis other than chronic compartment syndrome is suspected (e.g., stress fracture), the patient should be referred back to his or her treating physician for consultation › History • History of present illness/injury –Mechanism of injury: When did the patient first develop symptoms? What activity was the patient performing when symptoms began? Does the activity consistently cause the symptoms every time? Is there more than one activity that brings pain on? How long does the patient perform the aggravating activity before onset of symptoms? How long does it take for the symptoms to subside? What type of footwear does the patient wear during the activity? Any recent change in training or footwear? Any recent history of trauma? –Course of treatment - Medical management: Typically the patient will undergo conservative treatment first. Conservative treatment typically includes activity modification, cryotherapy, massage, and stretching. (5) If conservative treatment is unsuccessful or if job requirements demand continued activity, the physician will consider surgery (fasciotomy) - Fasciotomy is considered a safe and effective treatment for chronic compartment syndrome(33) - Various surgical techniques are used(3) - Generally a minor incision is made and the fascia surrounding the muscle is cut open to allow the muscle to expand with activity(3) - Medications for current illness/injury: Determine what medications clinician has prescribed; are they being taken? Are they effective? Nonsteroidal anti-inflammatory drugs (NSAIDs) may be recommended by physician - Diagnostic tests completed - Intramuscular pressure measurements (via a catheter/needle), pre and post exercise, are used to diagnosis chronic compartment syndrome(6,9) - Chronic compartment syndrome is indicated by pressures >15 mmHg at rest, >30 mmHg 1 minute after exertion, or >20 mmHg 5 minutes after exertion(25) - Exercise challenge testing should be personalized with an action that is analogous to the activity that causes the patient’s symptoms(39) - The majority of patients experience their leg symptoms during running activities, but in nonathletic older adults walking may be a stressor. Other common stressors include dancing, stair climbing, and prolonged standing - In a systematic review published in 2012, 38 studies were analyzed to assess the validity of the diagnostic criteria for chronic compartment syndrome. With the exception of resting pressure, the current criteria for diagnosing chronic compartment syndrome overlap the range found in normal healthy subjects. Several studies reported mean pressures that would prompt a diagnosis of chronic compartment syndrome, despite none of the subjects reporting any symptoms. The authors recommend clinicians use protocol-specific upper confidence limits to guide the diagnosis following failed conservative management(29) - Diagnostic utility of intramuscular pressure measurement is improved when measured continuously during exercise(34) - In a study conducted in the United Kingdom, a cutoff of 105 mm Hg during exercise provided better diagnostic accuracy than the criteria of 30 mm Hg and 20 mm Hg at 1 and 5 minutes, respectively, after exercise(34) - There are drawbacks to measurement of pressure during exercise, including that it is invasive and can be complicated by bleeding or infection, and that it is often difficult for patients to exercise with the catheter in place(3) - MRI has been used to assist in diagnosis;(9) MRI may also reveal signs of bone stress(4,10) - Near-infrared spectroscopy evaluates the hemoglobin saturation in tissue and also has been used to assist in diagnosis(4,9) - Electrodiagnostic testing (nerve conduction velocity, electromyography) to assist with differential diagnosis(30) - Neuropathy may develop in more severe cases of chronic compartment syndrome(30) - Home remedies/alternative therapies: Document any use of home remedies (e.g., ice or heating pack) or alternative therapies (e.g., acupuncture, herbal supplements, dry needling) and whether or not they help - Previous therapy: Document whether patient has had occupational or physical therapy for this or other conditions and what specific treatments were helpful or not helpful –Aggravating/easing factors (and length of time each item is performed before the symptoms come on or are eased) - Document frequency, duration, and intensity of training sessions(32) - Patients typically have no pain or symptoms while at rest(11) - During volitional contractions and passive stretching pain level will be increased(8) - Symptoms are frequently seen during repetitive movements (e.g., jogging, biking) and will cease once activity stops(3) - Over time, the period of rest required for resolution tends to increase,(11) and a low-intensityache may persist even when activity has ceased(3) - Typically occurs at the same point (duration/intensity) during exercise(6) and can usually be reliably predicted by the athlete(11) –Body chart: Use body chart to document location and nature of symptoms - Pain occurs in lower leg usually over involved compartment and typically occurs bilaterally(6) - Patients with upper extremity chronic compartment syndrome report symptoms most often in the forearm –Nature of symptoms: Document nature of symptoms (e.g., constant vs. intermittent, sharp, dull, aching, burning, numbness, tingling) - Pain is typically said to be “tight, cramp like or a squeezing ache” or burning in a certain region of the lower leg when chronic compartment syndrome is present(1) - Patients can report feelings of numbness and tingling through the lower leg and into the foot or through the forearm and into the wrist and hand(3) –Rating of symptoms: Use a visual analog scale (VAS) or 0-10 scale to assess symptoms at their best, at their worst, and at the moment (specifically address if pain is present now and how much) –Pattern of symptoms: Document changes in symptoms throughout the day and night, if any (A.M., mid-day, P.M., night); document changes in symptoms due to activity level, weather, or other external variables such as footwear or running surface (e.g., hard court, grass, track) –Sleep disturbance: Document number of wakings/night, if any - Chronic compartment syndrome should not disturb a patient’s sleep cycle –Other symptoms: Document other symptoms patient may be experiencing that could exacerbate the condition and/ or symptoms that could be indicative of a need to refer to physician (e.g., unexplained weight loss, saddle paresthesia, headaches, dizziness) –Barriers to learning - Are there any barriers to learning? Yes__ No__ - If Yes, describe _________________________ • Medical history –Past medical history - Previous history of same/similar diagnosis: Document history of compartment syndrome. Any other orthopedic injuries? - Comorbid diagnoses: Ask patient about other problems, including diabetes, cancer, heart disease, complications of pregnancy, psychiatric disorders, orthopedic disorders, etc. - Individuals with diabetes may be misdiagnosed with claudication pain instead of chronic compartment syndrome - Medications previously prescribed: Obtain a comprehensive list of medications prescribed and/or being taken (including over-the-counter drugs) - Other symptoms: Ask patient about other symptoms he or she may be experiencing • Social/occupational history –Patient’s goals: Document what the patient hopes to accomplish with therapy and in general –Vocation/avocation and associated repetitive behaviors, if any: Chronic compartment syndrome is recurrent and associated with repetitive physical activity, but it may also occur in sedentary individuals who get activity-related pain.(11) Does the patient participate in recreational or competitive sports? What are the demands of training (frequency, duration, location of training)? Athletes and military personnel are at increased risk –Functional limitations/assistance with ADLs/adaptive equipment: Note any limitations –Living environment: Stairs, number floors in home, with whom patient lives, caregivers, etc. › Relevant tests and measures: (While tests and measures are listed in alphabetical order, sequencing should be appropriate to patient medical condition, functional status, and setting) • Anthropometric characteristics –Circumferential measurements may be used to assess for edema; compare bilaterally. Mild edema may be noted in individuals with chronic compartment syndrome(2) –Assess for leg length discrepancy - Small asymmetries can have a large additive effect on overuse with a highly repetitive activity such as running(39) - The longer extremity is likely to work harder, resulting in overuse and muscle hypertrophy –Measure height, weight, and body mass index (BMI) –In a study conducted in the United Kingdom, subjects with chronic compartment syndrome were found to be significantly shorter in height than asymptomatic controls, although there was no difference in height:leg length ratio(34) - This raises the possibility that pathogenesis may be related to anthropometric characteristics(34) • Balance: Evaluate static and dynamic standing balance reactions such as Single-Limb-Stance (eyes open and closed), Romberg/Sharpened Romberg • Cardiorespiratory function and endurance: Document vital signs at rest and with activity. Note any abnormal heart rate or respiratory rate • Circulation: Evaluate distal pedal or wrist pulse bilaterally; at rest pulse would typically be normal but can be diminished at the onset of symptoms and following exercise. If arterial compression is suspected, further diagnostic testing is recommended (e.g., MRI)(4,6) • Ergonomics/body mechanics: Assess body mechanics and note any deviations with lifting and carrying objects • Gait/locomotion: Complete formal gait assessment and note deviations or asymmetry –Have patient perform the activity that elicits symptoms, noting time elapsed prior to patient’s complaints of symptoms –Assess running biomechanics if symptoms occur with running/jogging or biomechanics with upper extremity activity (e.g., swinging a racket, golf club) if symptoms occur with repetitive motion –Chronic compartment syndrome occurs more commonly in patients who pronate during running(3) • Joint integrity and mobility: Assess joint mobility of involved joints, noting any hypo- or hypermobility –Pain in a joint or worsened with joint movement is unlikely to be chronic compartment syndrome(39) • Muscle strength –Perform isolated manual muscle testing (MMT) for bilateral upper or lower extremity musculature, paying particular attention to the muscles within the suspected involved compartments. In severe forms of chronic compartment syndrome, diminished strength may be present(6) - Ankle dorsiflexion is weak when the anterior compartment is affected(27) - Ankle eversion is weak when the lateral compartment is affected(27) - Toe flexion is weak with posterior compartment(27) • Observation/inspection/palpation (including skin assessment) –Inspection is usually unremarkable; however, fascial defects may be observed(3) –Findings of muscle atrophy are not consistent with chronic compartment syndrome(39) –Palpate soft tissue structures for tenderness, pain, and increased tissue tension. Patient may complain of tenderness as clinician palpates over involved compartment(6) –Muscle herniation in the compartment may be palpated in approximately 40% of cases, especially in the lateral and anterior compartments, where the superficial peroneal nerve pierces the fascia(3) –Tenderness elicited on the anterior crest of the tibia may signal a stress fracture, periostitis, or tendonitis(8) • Posture: Assess patient’s standing posture and note any postural deviations that may be contributing to chronic compartment syndrome (e.g., calcaneal valgus, genu valgus, pes planus, meta)(1) –Pronation is a common finding(3) • Range of motion: Assess passive and active ROM and muscle flexibility throughout the lower extremity; passive stretch of involved muscles often elicits pain if done post exercise(8) • Reflex testing: Assess deep tendon reflexes (L4, L5, S1) bilaterally and note any hypo- or hyperreflexia • Sensory testing –Assess lower or upper extremity dermatomes, paying particular attention to the involved compartments. Decreased two-pointdiscrimination and light touch deficits are more reliable than decreased pinprick sensation(12) –Nerves within lower leg compartment(1,4) - Anterior compartment – deep peroneal nerve (paresthesia may occur in 1st web space or over dorsal aspect of foot) - Lateral compartment– superficial peroneal nerve (paresthesia may occur in the anterolateral region of the lower leg) - Superficial posterior compartment– sural nerve (paresthesia may occur on the dorsolateral foot) - Deep posterior compartment – posterior tibial nerve (paresthesia may occur in plantar region of foot) –Nerves within forearm compartment most likely affected are the ulnar, radial, and median nerves • Special tests specific to diagnosis –Single leg stance provocative stress test(39) - Used to accentuate the muscle masses of the anterior and posterior compartments - Patient is asked to stand on single leg first in as much ankle plantarflexion as possible, followed by in as much ankle dorsiflexion as possible - Rock hard bulging muscles are consistent with a diagnosis of chronic compartment syndrome of the respective compartments –Lower Extremity Functional Scale (LEFS) –Disabilities of the Arm, Shoulder and Hand (DASH) Outcome Measure –Quality of life: SF-36 or SF-8 Assessment/Plan of Care › Contraindications/precautions • Clinician should continually monitor for any exacerbation in symptoms and refer to physician as indicated • Clinician should not use procedures that might increase intracompartmental pressure; examples include deep massage, isometric contractions, and NMES • The pain typically disappears quickly with rest, causing no permanent damage to the tissue in the compartment, however if an athlete continues to compete through pain, chronic compartment syndrome can convert to acute irreversible compartment syndrome(11) • Cryotherapy contraindications(13) –Raynaud’s syndrome –Cryoglobulinemia –Cold urticaria –Paroxysmal cold hemoglobinuria –Impaired circulation • Cryotherapy precautions(13) –Hypertension – cold can lead to an increase in blood pressure –Hypersensitivity to cold –Avoid aggressive treatment with cold modalities over an acute wound –Avoid placement over superficial nerves for extended periods (> 1 hour) –Cold may be counterproductive if being used to facilitate muscle relaxation and reduce pain in patients who do not tolerate the modality • Thermotherapy contraindications(13) –Decreased circulation –Decreased sensation –Acute/subacute traumatic and inflammatory conditions –Skin infections –Impaired cognition or language barrier –Malignant tumors –Tendency for hemorrhage or edema –Heat rubs • Therapeutic ultrasound contraindications(13) –Over the region of a cardiac pacemaker –Over the pelvis, abdominal and lumbar regions during pregnancy –Over the eyes and testes –In an area with infection or bleeding –If a tumor is present in the area –In the area of deep vein thrombosis (DVT) or thrombophlebitis –Over the heart, stellate or cervical ganglia –Over epiphyseal plates • Therapeutic ultrasound precautions(13) –Sensory deficits –Individuals who cannot communicate effectively (e.g., impaired cognition, language barrier) –Circulatory impairments –Plastic or metal implants –Note: Always decrease ultrasound intensity if the patient complains of discomfort › Diagnosis/need for treatment • Physical therapy may be implemented as the first line of treatment for chronic compartment syndrome. Pain, limited ROM, weakness, abnormal gait biomechanics, and limited endurance all necessitate intervention. Physical therapy may be recommended following fasciotomy in order to regain strength, ROM, cardiorespiratory endurance, dynamic balance, and sport-specific activities. Physical therapists (PTs) should also address any biomechanical concerns associated with the patient’s activity • However, many physicians and clinicians believe that only surgery will offer patients a chance at complete resolution of symptoms and a full return to desired activity(2) › Rule out • Medial tibial stress syndrome (shin splints)(3,27) • Periostitis(4) • Tibial stress fracture(3,4) • Fibular stress fracture(1,3) • Peripheral neuropathy (e.g., common peroneal nerve compression)(4) • Popliteal artery entrapment syndrome(3,4) • Claudication due to peripheral arterial disease(3,39) • Muscle strain(27) • Venous insufficiency • Diabetes(27) • Muscle hyperdevelopment causing compression of the popliteal artery(3) • Cystic adventitial disease(3) • Delayed onset muscle soreness(39) › Prognosis • The natural course of chronic exertional compartment syndrome in the lower leg appears to be persistent symptoms over time(42) –Based on a case series conducted in Norway involving 12 military men who did not undergo fasciotomy and participated in a repeat pressure measurement after a mean time of 50 months –At the second visit all 12 patients still had typical complaints and elevated pressures • The majority of patients eventually require surgery to completely relieve symptoms(8) • If patient who is an athlete goes undiagnosed and untreated, the patient may give up his or her sport completely(27) • Chronic compartment syndrome sometimes converts to acute compartment syndrome if individuals continue competing despite the pain and other symptoms(27) • The rate of postsurgical recurrence of chronic compartment syndrome has been variably reported in the literature at between 3% and 17%(24) • United States researchers conducted a long-term follow-up study on high school and college patients with chronic compartment syndrome who underwent either nonoperative management (n=27) or fasciotomy (n=73)(28) –The mean follow-up period was ~5.4 years –The operative group reported a higher success rate (81%) compared to the nonoperative group (41%) –The surgical group reported higher patient satisfaction rate (81%) compared to 56% of the nonoperative group –Patients who underwent anterior and lateral releases compared to anterior release only reported a lower success rate –Surgical patients who were post college had a lower satisfaction rate (66%) compared with high school (89%) and college (94%) patients • Poor long-term prognosis following fasciotomy is related to improper diagnosis or failure for the surgeon to address multiple compartments in the leg simultaneously(26) › Return to duty rates after surgical treatment are poor(32,35,36) • Only 55% of patients in the military with chronic compartment syndrome experience complete resolution of symptoms(32) and only 41% return to full military duty(35) • Compared to the civilian literature, clinical outcomes after surgery are less optimal in the military population • These poorer outcomes may reflect the persistent physical demands and minimal allowance for activity modification in the military(35) › In a retrospective chart review involving 13 patients in the United States, rate of return to full elite level sport participation following fasciotomy was reported to be 100%(37) • 11 patients (84.6%) who had anterior and lateral compartment releases were able to return to full activity at a mean of 10.6 weeks. Patients who had four-compartment release took a mean of 3.5 weeks longer to return to full sporting activities › Complications of elective fasciotomy for chronic compartment syndrome have been reported with rates up to 11%(24) • Complications can include bleeding, infection, DVT, wound infection, lymphocele, and nerve injury(3) • A recurrence rate of 3-20% has been reported(3) –The most common reasons for recurrence are inadequate fascial release and excessive scar tissue formation causing the compartment to become tight again(3) • A potential long-term complication of fasciotomy is increased risk for chronic venous insufficiency due to loss of calf musculovenous pump(3) › Referral to other disciplines • Orthopedic surgeon –Should conservative methods fail, a fasciotomy is most likely indicated(3) –Failure of conservative treatment is generally thought to be when symptoms last more than 3 months(6) –Intramuscular pressure measurements can be obtained, if not already, to determine the need for surgery › Other considerations • Results of a large-scale study of the long-term outcomes and rates of disability after elective fasciotomy for chronic compartment syndrome of the leg indicate that chronic compartment syndrome is a substantial contributor to lower extremity disability in the United States military population(24) –611 patients who underwent 754 surgical procedures for lower extremity chronic compartment syndrome (anterior, lateral, and/or posterior compartment fasciotomies) were identified –Symptom recurrence was reported by 44.7% of the patients –27.7% were unable to return to full activity, and 17.3% were referred for medical discharge because of chronic compartment syndrome • Investigators in Norway reported an 81.1% long-term patient satisfaction rate following lower leg fasciotomy(26) –Patients were initially evaluated using a standardized clinical examination that included skin sensitivity, pre-andpost-ICP measurements after a symptom provoking step test, self-reported leg pain levels, and SF-8 quality of life scale –37 patients completed the 2-year follow-up period –Leg pain decreased from an average of 8 to 2.3 on a 0-10VAS –There was no significant correlation between VAS pain score and ICP levels prior to surgical intervention • Forearm fasciotomies have been reported to be successful in patients with chronic compartment syndrome in the forearm(14) –12 patients with chronic compartment syndrome underwent bilateral (in most cases) forearm fasciotomies –All participants were professional motorcycle racers –11 patients stated they had full resolution of pain or a significant decrease in pain –2 patients stated they lost strength in their forearm but not function postsurgery • Researchersin the Netherlands concluded that the success rate following deep posterior lower leg fasciotomy was relatively low(15) –46 patients with symptoms of deep posterior chronic compartment syndrome in the lower leg participated in the study - 27 patients met the identified surgical criteria for this study – pressure in the compartment was> 20 mmHg at rest, > 25 mmHg up to 1 minute after exercise, and > 20 mmHg 5 minutes after exercise –Results of follow-up (~3 years later) indicate that only 52% of the patients who had surgery felt their outcomes were successful –The researchers noted that the established cut-off points for the compartment pressure to deselect patients for surgery were justified based on the long-term success rate (84%) of conservative treatment in patients with lower pressures • In contrast, researchers in Canada found no appreciable differences in outcomes (LEFS score or satisfaction measures), length of time that patients were symptomatic before surgery, or time at which patients experienced their best outcome after surgery between a group of patients who had deep posterior compartment involvement and a group with anterior compartment involvement(40) –The researchers concluded that patients with deep posterior compartment syndrome fare better than is reported in the literature –Surgeon expertise with the fasciotomy technique is proposed as an explanation for the discrepancy • 4/5 patients in the United Kingdom who underwent a fasciotomy for the treatment of medial chronic compartment syndrome in the foot reported a significant reduction in symptoms at an average of 21 months postsurgery(16) –5 patients participated in the study; 7 feet were analyzed –3/5 patients in the study also underwent fasciotomy for chronic compartment syndrome in other regions of their lower extremities • A United States case study reported the onset of chronic compartment syndrome post direct, minor trauma to the lower extremity in a female military officer –The officer sustained a contusion in a softball game and avoided activity for 2 weeks –Upon resumption of her running program, symptoms of chronic compartment syndrome arose within the anterior compartment –The officer eventually underwent a fasciotomy in an effort to manage her discomfort and resume her normal activity level(17) › Treatment summary • Treatment typically revolves around suspension of the trigger activity(41) • Alteration in running technique has been reported to decrease pain and disability associated with chronic compartment syndrome, based on a study conducted in the United States(18) –In a case series, 10 consecutive patients who were runners with chronic compartment syndrome indicated for surgical release participated in a 6-week running intervention –Patients were trained to adopt a forefoot strike running technique rather than a hindfoot strike –Outcome measures included resting and post running compartment pressure, kinetic and kinematic measurements, and self-report questionnaires. Run distance and reported pain levels were recorded and a global rating of change scale was used to measure perceived change after the intervention –After 6 weeks of training mean post run compartment pressures had significantly decreased, running distance significantly increased and reported pain significantly decreased. Ground reaction forces were reduced, and self-report questionnaire scores were increased –One year after the intervention self-report scores were even higher than after the 6-week follow-up, and 2-mile run times were significantly faster than pre-intervention values –Surgical intervention was avoided for all patients • Patients may opt for conservative treatment despite the recommendation for surgical intervention(10) . Problem Goal Intervention Expected Progression Home Program Pain Alleviate pain Therapeutic strategies _ Rest is recommended in beginning stages of (4,6) treatment _ _ Elevation of affected extremity(4) _ _ Educate the patient on any noted training errors(2) _ _ Alteration of running technique(18) _ _ Alterations to the patient’s shoes, adding orthoses, and structure of training (including type of terrain and intensity) may further reduce the patient’s pain(6) _ _ Addressing any trigger points and adding massage to the treatment regimen may offer favorable results in the shortterm (long-term, these interventions have not been shown to be beneficial)(2) _ _ Physical agents and mechanical modalities _ Ice, heat, or ultrasound may be implemented in an attempt to alleviate symptoms(2) Gradual resumption of previous levels of training as symptoms allow(6) Implement a home exercise program as indicated for each unique patient Impaired ROM Improve ROM Stretching exercises _ Stretching and light massage to tight musculature; restore Progress as indicated Implement a home exercise program as indicated for each unique patient Therapeutic strategies Progress as indicated _ Therapeutic exercise should be implemented as indicated and appropriate; care should be taken to avoid exacerbating condition. Core strengthening may Implement a home exercise program as indicated for each unique patient Therapeutic strategies Progress as indicated _ Cardiovascular activities can begin once patient is pain free or only minimal symptoms are present Implement a home exercise program as indicated for each unique patient muscle length as able(3) Impaired strength Improve strength be indicated(2) Decreased endurance Improve endurance . Desired Outcomes/Outcome Measures › Decreased pain • VAS › Decreased edema • Circumferential measurements › Maximized ROM • Goniometry › Maximized strength • MMT › Improved cardiorespiratory endurance • 6MWT › Restored independence with functional mobility • LEFS • DASH Outcome Measure › Return to desired activity and activity level › Improved self-reported quality of life • SF-36 or SF-8 Maintenance or Prevention › Research results regarding prevention of chronic compartment syndrome are conflicting › Interventions for preventing lower limb soft tissue injuries in runners have limited support, based on a systematic review(19) • 12 trials with 8,806 subjects; most studies were limited to men in military training, so results may not be generalizable –There is some evidence for effectiveness of modification of training schedules; reducing the distance, frequency, and duration of running might be effective (based on 3 trials) –There is insufficient evidence to determine effectiveness of stretching exercises for major lower limb muscle groups (based on 5 trials) –There is insufficient evidence to determine effectiveness of insoles and footwear modification (based on 5 trials reviewed) › Evidence is inconclusive regarding the benefits of stretching and use of insoles in preventing overuse or training injuries in the lower extremity. These studies do not specifically pertain to chronic compartment syndrome • Stretching exercises 4 times daily (as compared to once daily) reduced risk of overuse leg injuries in study of U.S. military recruits during 13weeks basic training(20) –Overuse leg injuries included stress fractures, patellofemoral knee pain, muscle strain, tendonitis, plantar fasciitis, shin splints, and anterior compartment syndrome • Pre-exercise stretching did not significantly reduce training injuries in a randomized controlled trial(21) –1,538 Australian male army recruits (ages 17-35 years) randomized to stretch group (20-second stretches of lower extremity muscles during warm-up) vs. control group (warm-upactivities limited to non-stretching activities) for basic training that included 50 hours of physical training over 12 weeks –No significant differences were found in number of lower-limbinjuries when comparing stretch group vs. control –The most common injuries were tibial stress fractures, patellofemoral joint injuries, and ankle sprains • Researchers in Finland concluded that insoles might reduce lower limb injuries in military recruits based on a systematic review(22) –Included in the systematic review were 5 randomized or quasi-randomized trials evaluating different insoles in an effort to reduce lower extremity injuries compared to no insoles; 2,446 participants –All trials had methodologic limitations –4 trials reported statistically significant reductions in injuries • Shock-absorbing insoles do not appear to reduce lower limb injuries in military recruits(23) –1,205 military recruits in basic training in the United Kingdom were randomized to non-shock-absorbing insoles (Saran) vs. shock-absorbing insoles (Sorbothane) vs. shock-absorbing insoles (Poron) –Removal from training due to lower limb injury occurred in 18% of the Saran group, 17.3% of the Sorbothane group, and 19.8% of the Poron group –No statistically significant differences were reported Patient Education › Mayo Clinic Website, “Chronic Exertional Compartment Syndrome,”http://www.mayoclinic.com/health/chronic-exertional-compartment-syndrome/DS00789 › MedlinePlus. U.S. National Library of Medicine. National Institutes of Health. “Compartment Syndrome,”http:// www.nlm.nih.gov/medlineplus/ency/article/001224.htm Coding Matrix References are rated using the following codes, listed in order of strength: M Published meta-analysis SR Published systematic or integrative literature review RCT Published research (randomized controlled trial) R Published research (not randomized controlled trial) RV Published review of the literature RU Published research utilization report QI Published quality improvement report L Legislation C Case histories, case studies PGR Published government report G Published guidelines PFR Published funded report PP Policies, procedures, protocols X Practice exemplars, stories, opinions GI General or background information/texts/reports U Unpublished research, reviews, poster presentations or other such materials CP Conference proceedings, abstracts, presentation References 1. Wilder RP, Sethi S. Overuse injuries: tendinopathies, stress fractures, compartment syndrome, and shin splints. Clin Sports Med. 2004;23(1):55-81. (RV) 2. Padhiar N. Chronic compartment syndrome of the leg. Sportex Med. 2009;(40):16-22. (RV) 3. Herrera JE, Ibrahim MM. Compartment syndrome of the leg. In: Frontera WR, Silver JK, Rizzo TD Jr, eds. Essentials of Physical Medicine and Rehabilitation: Musculoskeletal Disorders, Pain, and Rehabilitation. 3rd ed. Philadelphia, PA: Saunders Elsevier; 2015:344-348. (GI) 4. Getzin A, Veigel J. Compartment syndrome, anterior. In: Bracker MD, ed. The 5-Minute Sports Medicine Consult. 2nd ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2011:88-89. (GI) 5. Brown GP, Skocypec J, Faust J. Rehabilitation of the foot and ankle complex. Compartment syndrome. In: Higgins M, ed. Therapeutic Exercise: From Theory to Practice. Philadelphia, PA: FA Davis Co; 2011:338. (GI) 6. Edwards PH, Wright ML, Hartman JF. A practical approach for the differential diagnosis of chronic leg pain in the athlete. Am J Sports Med. 2005;33(8):1241-1249. (RV) 7. Tzortziou V, Maffulli N, Padhiar N. Diagnosis and management of chronic exertional compartment syndrome (CECS) in the United Kingdom. Clin J Sport Med. 2006;16(3):209-213. (R) 8. Patel RV, Haddad FS. Compartment syndromes. Br J Hosp Med (Lond). 2005;66(10):583-586. (RV) 9. van den Brand JG, Nelson T, Verleisdonk EJ, van der Werken C. The diagnostic value of intracompartmental pressure measurement, magnetic resonance imaging, and near-infrared spectroscopy in chronic exertional compartment syndrome: a prospective study in 50 patients. Am J Sports Med. 2005;33(5):699-704. (R) 10. Seah R, Bell P. Chronic exertional compartment syndrome of the forearm musculature with ulnar bone stress in an elite tennis player. J Orthop Med. 2007;29(2):47-50. (C) 11. George CA, Hutchinson MR. Chronic exertional compartment syndrome. Clin Sports Med. 2012;31(2):307-319. (RV) 12. Fulkerson E, Razi A, Tejwani N. Review: acute compartment syndrome of the foot. Foot Ankle Int. 2003;24(2):180-187. (RV) 13. Michlovitz SL, Bellew JW, Nolan TP, Jr. Modalities for Therapeutic Intervention. 5th ed. Philadelphia, PA: F. A. Davis; 2012. (GI) 14. Leal S, Ziltener JL, Campos J, Menetrey J. Long-term outcome of fasciotomy for chronic exertional compartment syndrome of the forearm in competitive motor cyclists [abstract]. Isokinetics Exerc Sci. 2008;16(3):187. (R) 15. van Zoest WJ, Hoogeveen AR, Scheltinga MR, Sala HA, van Mourik JB, Brink PR. Chronic deep posterior compartment syndrome of the leg in athletes: postoperative results of fasciotomy. Int J Sports Med. 2008;29(5):419-423. (R) 16. Jowett A, Birks C, Blackney M. Chronic exertional compartment syndrome in the medial compartment of the foot. Foot Ankle Int. 2008;29(8):838-841. (R) 17. Tubb CC, Vermillion D. Chronic exertional compartment syndrome after minor injury to the lower extremity. Mil Med. 2001;166(4):366-368. (C) 18. Diebal AR, Gregory R, Alitz C, Gerber JP. Forefoot running improves pain and disability associated with chronic exertional compartment syndrome. Am J Sports Med. 2012;40(5):1060-1067. (R) 19. Yeung SS, Yeung EW, Gillespie LD. Interventions for preventing lower limb soft-tissue running injuries. Cochrane Database Syst Rev. 2011. Art No: CD001256. doi:10.1002/14651858.CD001256. (SR) 20. Hartig DE, Henderson JM. Increasing hamstring flexibility decreases lower extremity overuse injuries in military basic trainees. Am J Sports Med. 1999;27(2):173-176. (R) 21. Pope RP, Herbert RD, Kirwan JD, Graham BJ. A randomized trial of preexercise stretching for prevention of lower-limb injury. Med Sci Sports Exerc. 2000;32(2):271-277. (RCT) 22. Aaltonen S, Karjalainen H, Heinonen A, Parkkari J, Kujala UM. Prevention of sports injuries: systematic review of randomized controlled trials. Arch Intern Med. 2007;167(15):1585-1592. (SR) 23. Withnall R, Eastaugh J, Freemantle N. Do shock absorbing insoles in recruits undertaking high levels of physical activity reduce lower limb injury? A randomized controlled trial. J R Soc Med. 2006;99(1):32-37. (RCT) 24. Waterman BR, Laughl.in M, Kilcoyne K, Cameron KL, Owens BD. Surgical treatment of chronic exertional compartment syndrome of the leg: failure rates and postoperative disability in an active patient population. J Bone Joint Surg Am. 2013;95(7):592-596. doi:10.2106/JBJS.L.00481. (R) 25. Hansen PA, Willick SE. Musculoskeletal disorders of the lower limb. In: Braddom RL, ed. Physical Medicine and Rehabilitation. 4th ed. Philadelphia, PA: Elsevier Saunders; 2011:862-863. (GI) 26. Orlin JR, Oen J, Andersen JR. Changes in leg pain after bilateral fasciotomy to treat chronic compartment syndrome: a case series study. J Orthop Surg Res. 2013;8(1):6-12. doi:10.1186/1749-799x-8-6. (R) 27. Paik RS, Pepple DA, Hutchinson MR. Chronic exertional compartment syndrome. BMJ. 2013;346(7896):35-37. doi:10.1136/bmj.f33. (GI) 28. Packer JD, Day MS, Nguyen JT, et al. Functional outcomes and patient satisfaction after fasciotomy for chronic exertional compartment syndrome. J Sports Med. 2013;41(2):430-436. doi:10.1177/0363546512471330. (R) 29. Roberts A, Franklyn-Miller A. The validity of the diagnostic criteria used in chronic exertional compartment syndrome: a systematic review. Scand J Med Sci Sports. 2012;22(5):585-595. doi:10.1111/j.1600-0838.2011.01386.x. (SR) 30. Claflin ES, Robinson LR. wave abnormalities in a patient with possible chronic exertional compartment syndrome. Am J Phys Med Rehabil. 2013;92(8):734-735. doi:10.1097/ PHM<.0b013e3182555d48. (C) 31. Waterman BR, Liu J, Newcomb R, et al. Risk factors for chronic exertional compartment syndrome in a physically active military population. Am J Sports Med. 2013;41(11):2645-2649. doi:10.1177/0363546513497922. (R) 32. Dunn JC, Waterman BR. Chronic exertional compartment syndrome of the leg in the military. Clin Sports Med. 2014;33(4):693-705. doi:10.1016/j.csm.2014.06.010. (RV) 33. Pasic N, Bryant D, Willits K, Whitehead D. Assessing outcomes in individuals undergoing fasciotomy for chronic exertional compartment syndrome of the leg. Arthroscopy. 2015;31(4):707-713.e5. doi:10.1016/j.arthro.2014.10.018. (R) 34. Roscoe D, Roberts AJ, Hulse D. Intramuscular compartment pressure measurement in chronic exertional compartment syndrome: new and improved diagnostic criteria. Amer J Sports Med. 2015;43(2):392-398. doi:10.1177/036354651455970. (R) 35. McCallum JR, Cook JB, Hines AC, Shaha JS, Jex JW, Orchowski JR. Return to duty after elective fasciotomy for chronic exertional compartment syndrome. Foot Ankle Int. 2014;35(9):871-875. doi:10.1177/1071100714539661. (R) 36. Roberts AJ, Krishnasamy P, Quayle JM, Houghton JM. Outcomes of surgery for chronic exertional compartment syndrome in a military population. J Royal Army Med Corps. 2015;161(1):42-44. doi:10.1136/jramc-2013-000191. (R) 37. Irion V, Magnussen RA, Miller TL, Kaeding CC. Return to activity following fasciotomy for chronic exertional compartment syndrome. Eur J Orthop Surg Traum. 2014;24(7):1223-1230. doi:10.1007/s00590-014-1433-0. (R) 38. Brennan FH, Jr, Kane SF. Diagnosis, treatment options, and rehabilitation of chronic lower leg exertional compartment syndrome. Curr Sport Med Rep. 2003;2(5):247-250. (RV) 39. Strauss MB. Chronic exertional compartment syndrome: Myths, misconceptions, and fallacies. Consultant. 2015;55(6):450-456. (RV) 40. Pasic N, Bryant D, Willits K, Whitehead D. Assessing outcomes in individuals undergoing fasciotomy for chronic exertional compartment syndrome of the leg. Arthroscopy. 2015;31(4):707-713.e5. doi:10.1016/j.arthro.2014.10.018. (R) 41. Pozzi A, Pivato G, Kask K, Susini F, Pegoli L. Single portal endoscopic treatment for chronic exertional compartment syndrome of the forearm. Tech Hand Up Extrem Surg. 2014;18(3):153-156. doi:10.1097/BTH.0000000000000056. (R) 42. Van der Wal WA, Heesterbeek PJ, Van den Brand JG, Verleisdonk EJ. The natural course of chronic exertional compartment syndrome of the lower leg. Knee Surg Sports Traumatol Arthrosc. 2015;23(7):2136-2141. doi:10.1007/s00167-014-2847-2. (R)