* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download APTC*s Price and Performances
Survey
Document related concepts
Transcript
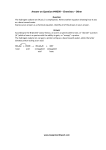
APTC’s Tender: Introduction, Requirements and Aims J. Verwey (editor), August 22, 2014 [CB:3880] Content 1 Introduction ....................................................................................................................... 2 2 Basic requirements and basic scope .................................................................................... 3 2.1 Basic requirements ........................................................................................................... 3 2.2 Basic scope of equipment................................................................................................. 4 3 Tenderer’s substantiation of cost ........................................................................................ 4 4 APTC’s tender aims and sought performances ..................................................................... 5 5 APTC’s Expectations (‘What We Think We Want’) ............................................................... 7 A.1. State-of-the-art and beyond in conventional radiotherapy.................................... 12 A.2. Summary of APTC’s research program CITE ............................................................ 14 1 Introduction APTC B.V. (Amsterdam Proton Therapy Center), founded by the Netherlands Cancer Institute (Antoni van Leeuwenhoek – AVL) and the academic medical centers VU University Medical Center (VUmc) and Academic Medical Center (AMC), invites vendors to tender for proton therapy equipment with the aim to jointly realize a beyond-state-of-the-art proton therapy center. This tender concerns the supply of key components for the treatment of patients with protons and for practice-changing research. The aim of APTC is to become one of the leading centers worldwide. In the Netherlands, the provision of proton therapy is regulated by a permit system. APTC received, as one of the four Dutch initiatives, the permit in February 2014. As of today, no reimbursement rates have been determined, and the Dutch healthcare insurance companies have not yet contracted with any of the initiatives. Zorgverzekeraars Nederland (ZN), an association of which all Dutch healthcare insurance companies are a member, has publicly stated that they do not intend to contract with all permit holders, and that they are considering a tender to decide with which initiative to contract. The required reimbursement rate, for the proton therapy center to ‘break even’, is expected to be an important criterium in this tender. The cost of the proton therapy equipment is thus expected to play a pivotal role in determining whether APTC will be contracted, and hence whether it can be realized. The permit system comes with conditions and requirements, making the challenges and the requirements for proton therapy centers in the Netherlands unique in the world. In the Dutch system, for most of the eligible patients, a proton treatment plan needs to be compared with a state of the art photon plan, and demonstrate an expected clinically relevant benefit by meeting certain criteria. Hence, the level of technology that APTC needs in order to be and remain viable as a center is co-determined by today’s state of the art technology in photon therapy, as well as expected developments therein. APTC assumes that the ability to provide a clinically relevant benefit with proton therapy over conventional radiotherapy, for a significant number of patients, both now and in the future, is not only the overarching aim of a proton therapy center, but also for a vendor of proton therapy equipment. APTC’s research program CITE, (see appendix A.2) is designed to provide the scientific requirements to ensure this aim can be achieved, providing the basis for APTC’s tender requirements. APTC believes it is uniquely positioned to – in close collaboration with the supplier – realize this shared aim. APTC is an initiative of three internationally renowned centers, including a comprehensive cancer center (AVL) and two academic medical centers (VUmc and AMC). The academic centers rank 15 and 44 in the field of medical sciences among 240 ranked European universities in the CWTS Leiden Ranking 2014. The radiotherapy departments of AVL and VUmc are major research and development partners of the main suppliers in conventional radiotherapy with demonstrated expertise in imaging, motion management, and the introduction of innovative treatment techniques. The combined expertise (research and clinical) of the radiotherapy departments of AMC, AVL, and VUmc is unique in the Netherlands, and possibly matched by only a few centers worldwide. The radiotherapy departments of AMC, AVL and VUmc are reference centers for all proton therapy indications and established referral patterns are in place. APTC’s aim stems from the available expertise and current level of technology in the radiotherapy departments of AMC, AVL and VUmc, and the expected developments in conventional radiotherapy in the coming years. These developments, to which the founders of APTC have contributed and are still contributing significantly – notably, but not exclusively in the field of image-guidance, motion management and adaptive strategies – are thus important to appreciate APTC’s vision, the research program CITE, and the tender aims, and have been described in appendix A.1. Aim of APTC: APTC’s clinical performance (proton therapy) must, over the operational lifetime of the proton therapy center, be able to consistently outperform the clinical performance (photon therapy) of the combined achievements of the radiotherapy departments of AMC, AVL and VUmc for a significant number of patients, leading to the development and implementation of innovative, practice changing treatment strategies, while continuously reducing the cost differential with photon therapy for these patients. APTC recognizes that, in order to realize its aim, it relies heavily on the available expertise with the tenderer (as expressed by the performances of its equipment, the developments therein, and in the capacity to implement technical and clinical innovations), and has opted for the Best Value Procurement (BVP) approach in combination with the tendering procedure of competitive dialogue. This combination provides maximal room for APTC and the tenderers to bring in their own unique expertise working towards a shared aim. The BVP approach results in the optimal alignment of expertise and a clear assignment of project risks, which both are important elements in reducing price. In the dialogue phase the tenderers’ expertise and innovative solutions will aid APTC in more clearly defining its aims and how to achieve them, especially in the fields of future developments and implementation. Specific elements in the agreement will also be discussed in this phase. Given APTC’s aims and the dependence on the tenderer’s expertise, APTC invites all tenderer’s who meet the basic requirements to participate in this dialogue. The tendering guidelines, the required BVP documents and awarding criteria are described in the information provided through the Negometrix platform. This document contains APTC’s basic requirements, basic scope of the equipment, and tender aims (with per aim a description of sought performances) as required to draw up the BVP documents. Where applicable APTC has, for the sought performances, provided a description of ‘What we think we want’. 2 Basic requirements and basic scope 2.1 Basic requirements Table 1 Basic requirements. # 1 2 3 4 5 6 Requirement Cyclotron, delivering a continuous wave proton beam. Gantry able to rotate at least 360 degrees. Pencil Beam Scanning (PBS) delivering technique for each gantry. The degrader and the Energy Selection System (ESS) is placed outside of the treatment room. Able to meet the imaging requirements defined by APTC (see Table 4). The proton therapy equipment (including software and control) with which the tenderer will realise the in the tender documents stated performances (i.e. from the operational start of APTC), is to be certified following national rules and regulations in 2016. For improvements/enhancements on the stated performances no such requirement exists. 2.2 7 The Oncology Information System (OIS) Mosaiq and Aria must be supported. The control system of the proton therapy delivery machine must interface with the OIS and provide all relevant treatment parameters to the OIS for record and verify purposes. 8 Operational service level uptime requirements of fifty-two weeks a year: 16 hours a day (06:30 to 23:30) for five days a week, and 9 hours (08:00 to 17:00) on Saturday. 9 APTC is to use a European tender to decide upon the Treatment Planning System (TPS). In case the tenderer does not already support the TPS selected by APTC, the tenderer will provide the TPS-supplier all the information required to prepare the TPS for treatment planning with the supplier’s equipment. This information is to be provided within three months of APTC signing the contract with the TPS-supplier. 10 Tenderer is able to provide support and maintenance for at least 10 years following the start of clinical operation. 11 The ability to have at least one treatment room accepted and ready for clinical commissioning within 34 months after signing the contract Basic scope of equipment The offering is to include the following proton therapy equipment: Cyclotron Beam transfer lines from cyclotron to three separate gantry rooms Three gantries (procurement of the third gantry is conditional, see the Agreement, (APTC doc 06)) To be priced separately (as an option): extension of the beam transfer line to APTC’s horizontal beam room. 3 Tenderer’s substantiation of cost Cost is an important element of APTC’s awarding criteria. A substantiation of the cost (how the cost is build up) is a separate awarding criteria (see ‘Awarding criteria’ on Negometrix platform). The aim of this substantiation is to provide transparency: not the cost will be graded, but the overall transparency and clarity provided in the document. In Table 2 some elements that APTC seems relevant in underpinning the price components have been listed. This list is not exhaustive and the tenderer is absolutely free to provide other, additional and or better performances in support of realizing the stated aim as it sees fit. Table 2 Underpinning of price structure Aim [P] # P.1 P.2 P.3 P.4 P.5 P.6 P.7 P.8 It is the aim of APTC to, over the entire operational life time of the proton therapy center, to consistently outperform photon therapy, while continuously reducing the cost differential with photon therapy (for treatment of the same patients) Elements deemed relevant to substantiation of cost structure General: The combined goals of a high performing state-of-the-art proton therapy center and reducing the cost differential with photon therapy may have led to choices that affect the price of some or all of the components. Sought is a description of these choices, and their impact on the cost components. The relationship between scheduled maintenance and technological lifetime of key components. To what extent it is possible for APTC to, eventually, provide first level support, and to what financial effect. (In the cost calculation template available on the Negometrix platform an indication of this effect is to be provided). The potential impact of energy consumption saving technology that is part of expected updates and or (priced in) upgrades. A description/explanation of payment scheme for equipment costs. (In the cost calculation template available on the Negometrix platform the tenderer is to provide the annual payments). A description/explanation of payment scheme for maintenance and operational costs. (In the cost calculation template available on the Negometrix platform the tenderer is to provide the annual payments). A description/explanation of how total equipment costs and annual maintenance and operational costs are related. A description/explanation of indicated reductions of cost in case a third gantry is not purchased, and in case APTC would be able to provide level-1 support. (In the cost calculation template available on the Negometrix platform an indication of this effect is to be provided). 4 APTC’s tender aims and sought performances To achieve APTC’s overall aim as mentioned in the introduction, the aims [A] to [D] have been defined (see Table 3). For each aim APTC has provided a couple of performances that APTC thinks relevant to the aim and hence could be used by the tenderer in the BVP documents. This list is not exhaustive and the tenderer is absolutely free to provide other, additional and or better performances in support of realizing the aim as it sees fit. Table 3 APTC's required performances. Aim [A] # A.1 APTC is to select a supplier able to provide, install and maintain a compact proton therapy system to safely achieve maximum tumor control with minimal side effects, with a first patient treatment taking place within three years of signing the contract. Sought performances The PBS technique installed at each gantry allows for IMPT and enables implementation of highly conformal state-of-the-art treatment strategies for both adult and pediatric tumors, either mobile or immobile, both superficial or positioned at greater depth. Relevant criteria are: Minimal spot size at shallow depth A.2 Aim [B] B.1 B.2 B.3 Aim [C] C.1 C.2 C.3 C.4 C.5 Minimal beam delivery time Fast energy switching Minimal safe distance between snout-exit and patient’s surface The proton therapy system (the total of all equipment, the bunkers and necessary rooms for operation and maintenance of the equipment), is compact, allowing for maximum freedom in configuration of the patient building and leaving maximum room on the available plot for future additions to the center. APTC is to select a supplier who, wherever possible in collaboration with APTC, continues to contribute to the safety and further proliferation of proton therapy (through the ongoing development of its equipment and the clinical implementation of these developments on the provided system), with the aim to establish APTC as a leading proton therapy center Sought performances In part based on developments in conventional radiotherapy APTC sees the following topics as relevant (in stated order, non-exhaustive): 1. Continuous line and contour scanning 2. Option of (later addition of) (a) heavier particle(s) 3. MRI guidance 4. Range verification system 5. Active motion management 6. Multiple nozzles to combine large field sizes and small air-gap The supplier contributes to APTC’s research program CITE (see appendix A.2 for a summary), jointly working towards the implementation of innovative, practice changing treatment strategies. Implementation of new functionality (software and or hardware updates and upgrades) taking place after start of treatment of the first patient has minimal impact on clinical operation. APTC is to select a supplier who provides a proton therapy system with an optimal workflow (with a productivity comparable to that of photon therapy for similar complexity of a given indication), with a high operational availability Sought performances (Near) instantaneous beam availability in each treatment room. Based on the current workflow in conventional radiotherapy and foreseen developments therein, and assuming a facility with up to four treatment rooms, the following elements are deemed relevant: 1. Safe, remote and automated ‘scripted’ sequence of movements of elements with patient-specific settings. 2. Comprehensible and easy to use automated beam request and beam switching software. 3. Utmost flexibility in treating the patient in the next available treatment room without having to recalculate the plan. Beam down time in line with top performers in the industry. Immediate, straightforward access to all logged machine data relevant to the aim of fast QA procedures (including patient specific dose reconstruction), continuous improvement of the workflow, and for potential use in APTC’s research program. Maximum availability (number of hours) and maximum flexibility (distribution of hours) of beam time for clinical activities and research. Aim [D] D.1 D.2 The system is able to meet the imaging requirements as defined by APTC Sought performances Imaging requirements as described in Table 4. APTC explicitly invites tenderers to provide additional imaging tools, solutions and/or developments in the ‘Added Value’ document that contribute to APTC’s aims. Table 4. APTC’s Imaging requirements. General Optional (to be priced separately1) 2D, 3D and 4D imaging at iso-center in co-planar treatment position Minimal imaging to treatment iso-center deviations Large field of view including seamless acquisition of multiple couch positions Imaging system rotates independently of the proton gantry Minimal acquisition times High temporal resolution Fast and transparent interfaces for APTC reconstruction and registration software in clinical operation (raw imaging data should be available for external processing) Imaging during PBS possible Large dynamic range in imaging dose to facilitate guidance protocols ranging from pediatric bony alignment to adult soft-tissue alignment High image quality Diagnostic image quality (preferable at treatment iso center) in at least one treatment room Surface imaging tool Diagnostic CT quality imaging in more than one room Stereoscopic imaging 5 APTC’s Expectations (‘What We Think We Want’) The tenderer is not to provide a detailed scope in its BVP documents. It is however important for the tenderer to be aware of APTC’s expectations. The awarded tenderer may, however, be able to demonstrate that the requested performance can be met with parameters that lie outside of the expected range of APTC. Hence APTC expectations are not minimum requirements per se. The identifier in the first column refers to the identical identifier in Table 3. 1 On the Negometrix platform APTC provides an excel template to be filled out by the tenderer to determine total cost. See separate tab ‘PRICING OF OPTIONS’ on this template. Table 5 Expected performances sought by APTC. # A.1 A.2 B.3 C.1 C.2 C.3 C.4 C.5 D.2 ‘What we think we want’ For expectations with respect to the treatment equipment see Table 6. Area for proton therapy equipment and required spaces for operation and maintenance of equipment preferably within an area of 55x32 m2. There is no fixed restriction with respect to depth of pit, but given the plot conditions extra costs will arise at greater depth. A depth of up to 6-8 meter is considered acceptable. Updates and or upgrades (hardware and or software) are scheduled such that they have minimal impact on clinical operation (to avoid the situation whereby projected loss of revenue prohibits essential updates and or upgrades). Each treatment room with its own separate energy degrader/Energy Selection System (ESS) combination placed outside of the treatment room (to be operational when approaching full capacity). Beam can be switched between rooms after each field (not only at completion of fraction), and beam switching time (time from completion of dose delivery of field to start of dose delivery of field in another room) is in the order of seconds. 1) Safety precautions to allow for automated movements are required. Goal is that no operator shall be required to enter the treatment room in order to continue a treatment. 2) Beam is to be made available to a treatment room without the required use of an operator in the main control room. 3) a) There shall be no requirement that a patient’s plan can only be delivered by a single treatment room. b) The gantries are mechanically identical (same monitors in beam path etc.) c) Variation in the lateral dose fall-off 80-20% for higher energies expected to be no greater than 1 mm. Expected range for downtime: [2-4%]. (Availability rate in SLA proposed to be 95%, but better performance is the aim). Immediate straightforward access to relevant data in log files at any time include: Timing data of: o Imaging activities o Activities that are part of the patient positioning procedure o Position correction activities o Treatment activities All parameters required to accurately reconstruct delivered dose (with the aim of efficient phantom-less patient-specific dosimetry) Maintenance data of pivotal components: o Performance parameters o Failure and cause of failure o Repair/replacement time Interlock data Maximum operational availability is minimally affected by scheduled maintenance (minimal number of scheduled non-treatment days, and a minimized number of consecutive non-treatment days). Such as e.g. MRI on rails to be used both inside and outside the treatment room. Table 6. Expected values of important system parameters Item Expected Values (not minimal requirements) Cyclotron ESS/Degrader Snout Combination of beam current and extraction efficiency sufficiently high to allow for simultaneous treatment in 2 treatment rooms. Minimal activation to allow for short enough maintenance times in line with expected clinical availability of overall system. Beam intensity changes from full intensity to zero fast and accurate enough to allow for current modulation as required for continuous line scanning Maximum energy at least 230 MeV. The energy switching time is less than 0.5 seconds for a typical range-change in a treatment field. Minimum clinically available energy (without use of range shifters) of at most 70 MeV. The maximum distance of the snout exit to the iso-center is large enough to allow collision-free 360 degree rotation of the gantry without moving the patient The snout is optimized to maximally reduce the distance between snout exit and surface of the patient with the tumor aligned at isocenter Range shifter material in the nozzle to shift the range to shallower depths is placed as close to the patient as possible. The pencil beam can be scanned over a field with a maximum field size that is between 25x25 to 30x30cm2, centered at the isocenter. Snout position for each patient is known (and script allows for automated set up of snout position prior to treatment) For scanning proton therapy the maximum range in water at the iso-center position of the gantry is at least 30 g/cm2 The minimum range without further degrading after the ESS is at most 4 g/cm2 The distal Falloff (80% - 20%) in water is <= 0.1 g/cm above range straggling of mono-energetic beam. The maximum absolute deviation of the spot from the prescribed position is less than 1 mm. For 95% of the voxel distribution (size 2x2x2 mm3) of a homogeneous dose inside a volume of 10x10x10 cm3 centered around the iso-center with a depth in the range of 5-20 cm water the deviation of the dose from the central dose is less than ±2%. The gantry can scan a volume of 10x10x10cm3 centered around the iso-center with the iso center at any depth in the range of 1025 g/cm2 water, depositing a dose of 0.7 Gy with a homogeneous dose distribution as specified in the above within 10 seconds. Beam Beam is optimized for the treatment of shallow tumors through: o Small spot size at low energies o A low minimal energy without range shifter (<=70 MeV) o Remote control of automatic placement of range shifter plate (ideally: able to change position during the treatment of the field itself) Beam switching time (as defined from completion of treatment field to beginning of treatment of field in another room) at most a couple of seconds The system is suitable for/capable of applying continuous linescanning with a speed up to 10 cm/ms. The ability to interrupt the beam for gated/breath-hold based motion management with a public interface between imaging system and TCS that has a sufficiently fast response time for clinical applications. Spot size PPS Safety Imaging Beam Energy (MeV) Range (g/cm2) Spot size in air (1 SD, mm) 70 4.1 6 100 7.7 5 150 16 4 The accuracy and precision of translations is better than 1 mm for the treated volume. The accuracy and precision of rotations is better than 0.25 deg. The motions of the PPS are driven using a smooth velocity profile. Remote control. Allows for unperturbed ‘docking’ of a table with a (pre-positioned) patient on it. Ability to treat through table (homogeneous density; special care taken to treat through table in head/shoulder area). Distance nozzle-exit and patient can be made as small as possible. The response time to any failure (including mismatches between machine control system, TPS steering file and TVS) is fast enough to limit the dose deposited to 3% of the prescribed fraction dose in the treatment volume (with a maximum of 4cGy) when using the maximum possible dose rate. After beam interruption it is possible to resume treatment starting from the control point at which an unexpected beam interruption occurred. Resume should be possible both within the same session as well as in a next session. A collision prevention and detection system is available. Imaging coordinate system to treatment isocenter deviations < 1mm. X-ray source and panel frame rate >= 15 fps with a delay < 100 ms. Volumetric imaging acquisition time <= 15 s. Fluence and energy range allowing for volumetric iso-centric imaging dose <0.1cGy (pediatrics) and >5cGy (adults). Planar FOV @ iso-center of at least 25 cm x 25 cm. Volumetric FOV large enough to capture complete skin line in transverse view, longitudinal at least 25 cm at iso-center. Dual energy fluoroscopy and volumetric capabilities. Mechanical reproducibility facilitating a spatial resolution of at least 10 lp/cm. Image quality at least competitive with IGRT systems available in photon therapy. Appendix A A.1. State-of-the-art and beyond in conventional radiotherapy In the last decade there have been several important technological improvements in photon based radiotherapy (RT) that have changed the clinical practice in radiotherapy drastically. Emerging technologies continuously establish further enhancements in photon based radiotherapy. In the following an overview of these developments is given for different aspects of the radiotherapeutic treatment delivery. Better conformation Using IMRT, a breakthrough has been achieved in achieving superior conformance of the high dose to the planning target volume in 3D and thus better sparing of critical organs. A further development was the introduction of helical and volumetric intensity modulated arc-therapy (VMAT), which gives equal or even better dose distributions. With VMAT, treatment delivery times were substantially reduced compared to conventional IMRT. Enhancements in treatment planning drive towards automated Pareto optimised treatment plans that incorporate all degrees of freedom available with modern linear accelerators. Using these techniques sharp dose gradients that approach the penumbra width of a 6MV beam (10%/mm) can be achieved for optimal sparing of organs at risk adjacent to the planning target volume. More precise To deliver the highly conformal dose distributions with high precision, improvements have been implemented in treatment machine technology. Examples are high-definition MLC with leaf width of a few millimeters, sub-millimeter isocentric precision of the beam and the introduction of very precise robotic 6 degrees of freedom patient support systems. More importantly, 2D (using MV and kV imaging) and 3D cone beam CT (CBCT) pre-treatment imaging of the patient in treatment position at the isocentre is already routine practice in photon RT for several years. CBCT enables soft-tissue imaging, and the developments are to increase the HU accuracy and image quality towards the standards known in diagnostic CT systems. The precision of the IGRT systems, depending on the hardware configuration, is typically at millimeter or even at the sub-millimeter level. Modern systems are equipped with advanced software packages for (automatic) analysis of positioning errors, in combination with automatic couch corrections. In practice a CBCT-based IGRT procedure including couch correction can be performed withing 5 minutes. At present imaging of the patient during treatment is being introduced, facilitating monitoring of the patient positioning during beam delivery. An important development is the introduction of integrated MRi-Linacs or MRi – Linac suites, in order to exploit the superior soft tissue contrast and advanced imaging possibilities of MRi (several systems are being developed, one of which is at the time of writing commercially available). Seeing what you treat, also during treatment delivery will further reduce the volumes to be treated and thus enable further normal tissue sparing or dose escalation for tumors that are difficult to treat at present. Motion management Treating targets that move with respiration has seen several developments. Using 4D-CBCT, though image quality is inevitably poorer than normal CBCT, it is possible to assess the respiratory motion of targets in 3D based on soft tissue contrast. Beam delivery can, if necessary, be performed with gated treatments using integrated systems that track respiratory breathing. These systems can also be used in combination with breathhold techniques. IGRT facilitates 2D imaging (fluoroscopy) to verify breathing motion before treatment. If fiducials are inserted in or close to the target, real time tracking of the fiducial (i.e. target) has become feasible, that can be used to dynamically track tumor motion using either MLC or the couch. In an integrated MRI-Linac unit it is possible to perform real-time tracking of the target (or OAR’s) using MRi without the need for implanted fiducials, also for targets in the upper abdomen. Speed of delivery To make treatment times shorter there are developments on hardware and software. Next to the introduction of VMAT, which enabled a faster delivery of IMRT also high-intensity treatment techniques were introduced making use of flattening-filter free beams. Furthermore advances in treatment console software facilitate automated delivery of multiple segments and beams with so-called ‘one-button’ operation. Remote operation of movements is possible, using automated dry-run sequences for safety checking in conjunction with collision detection techniques. As a result a hypo-fractionated treatment using high fraction dose, in which CBCT image guidance is used for positioning and intrafraction verification, can be delivered within 20 minutes (including patient positioning on the couch). Standard VMAT techniques with on-line image guidance can be done in less than 15 minutes. More secure Despite the fact that treatment techniques have become more complex in the last decade, the rate of errors in treatment delivery has declined. This is due to an increasing level of automation, integration of software systems and increasing level of interoperability of different software packages. Also automated verification steps in conjunction with an authorization system reduces the chance on errors. Furthermore, in photon therapy it is possible to perform an ultimate verification of delivered dose by performing in-vivo dosimetry where actual delivered dose to the patient is measured using the electronic portal imaging device and compared with the planned dose. Adaptive RT Using the results of the 3D CBCT (or MRi based) image-guidance, changes in patient anatomy can be detected. This information can be used to adapt the treatment plan to the new situation. State-of-the art is to create a new plan offline in case of systematic changes in patient anatomy. If changes in anatomy are more of a random nature it is possible to use a plan of the day chosen from a library of plans that are made for several anatomic conditions of the patient (like different levels of bladder filling). Ultimately, if there is no prior knowledge on anatomical variations, one has to perform daily on-line replanning to adapt the plan to the anatomy of the day. The latter requires a seamless integration of image-guidance system, treatment planning system and treatment delivery system. A.2. Summary of APTC’s research program CITE A.2.1 Introduction APTC’s research program (called CITE) stems from the combined expertise and strengths of the three oncology centers in general, and the radiotherapy departments in particular. For many years now the radiotherapy departments of AMC, AVL and VUmc collaborate in the fields of research and education, providing training programs for radio-oncologists and medical physicists. Doctoral students of all three departments participate in the OOA program (the joint graduate school of AMC, AVL and VUmc), the strength of which is based on the integration of the basic, translational and clinical oncology research in the three oncology centers. Three professors with appointments at two universities take full part in APTC’s research program (Prof C.R.N. Rasch – Adaptive radiotherapy at the University of Amsterdam, Prof M. van Herk – Image guided radiotherapy at the University of Amsterdam , Prof M. Verheij – translational radiotherapy at the VU Free University), each supervising a large group of researchers. Much of CITE’s program is a continuation of or built on existing research lines for photons. There is a long list of clinical and technical research projects where at least two of the three departments are involved. APTC has the ambition to become a ‘beyond state of the art’ proton therapy center. To realize this ambition a research program has been defined that aims to improve both the clinical performance of proton therapy as well as essential elements of the proton therapy workflow. Existing and future tools and strategies available to photon therapy and relevant for proton therapy to provide a significant clinical benefit, provide a focal point for the research aims of CITE’s various research lines. Near instantaneous, or instantaneous, beam availability of different energies in all treatment rooms, access to all treatment angles without having to move the patient, single breath-hold field deliveries, continuous line scanning, instant beam availability for gating and/or continuous tracking of mobile tumors are all considered pivotal bringing proton therapy forward, both in clinical terms and with respect to workflow. The latter aspects require versatile imaging tools, including imaging during treatment, and powerful and fast reconstruction and registration software. These CITE’s research lines build on the existing imaging and image processing strengths of AMC, AVL and VUmc. Ultimately it is the combination of APTC’s and the vendor’s clinical and technical expertise that will result in the development and implementation of innovative, practice changing treatment strategies. A.2.2 The CITE research lines Although APTC’s research program is organized in four research lines, many of the aims of the various lines are closely related and frequently go hand in hand. CITE comprises the following research lines: i. ii. iii. iv. Clinical research Image-guided and adaptive proton therapy (IGAPT) Treatment planning Efficiency en effectiveness ‘Clinical research’ focuses on (the improvement of) ‘outcome modeling’, prospective cohort studies, and clinical trials. ‘Image guidance and adaptive proton therapy’ (IGAPT) aims to minimize the deviations between the planned and actually delivered dose through image guided patient positioning, advanced correction strategies, and adaptive planning. In the line ‘Treatment planning’ the focus is on the development of optimization methods for robust treatment (re-)planning. ‘Efficiency and effectiveness’ includes improving the workflow and patient scheduling, as well as the efficient clinical implementation of the outcome of research from the IGAPT and Treatment Planning research lines. Research into (improving) cost efficiency of proton therapy is a final important element of this research line. A.2.3 CITE: Clinical research Prof. Dr. S. Senan1, Dr. R. Haas2, Dr. L. Stalpers3 1 Radiation-oncologist, Department of Radiotherapy, VUmc Radiation-oncologist, Department of Radiotherapy, AVL 3 Radiation-oncologist, Department of Radiotherapy, AMC 2 Background and expertise The Clinical research line will develop a methodology to select the appropriate patient cohorts for proton therapy through outcome modeling, prospective cohort studies and clinical trials. The development of realistic predictive models for tumor control and treatment related side effects has first priority. There is a wide range of expertise within the Amsterdam centers in the field of clinical research of tumors indicated for proton therapy. Examples are head and neck tumors at VUmc and AVL, lung tumors at the AVL and VUmc, pediatric oncology at the AMCand VUmc, and breast cancer at the AVL. Together AMC, AVL en VUmc dispose of a large database that enables both outcome modeling and data mining. Because of the large group of patients treated by AMC, AVL and VUmc (20% of all patients treated in the Netherlands) APTC is able to perform prospective cohort studies and clinical trials within a relatively short time, allowing for a quick translation of outcomes into the clinical practice. Clinical Research - Aims Improvement of predictive models of late effects, and reduction of toxicity Development of reliable methods for the early detection of (the location of) recurrences Analysis of Quality of Life following proton therapy (using Patient Reported Outcome) Demonstration of clinical benefit of proton therapy through clinical trials A.2.4 CITE: Image-guided and adaptive proton therapy (IGAPT) Dr. ir. J.-J, Sonke1, Dr. A. Bel2, Dr. M. Dahele3 1 Group leader adaptive radiotherapy, Department of radiotherapy, AVL Head physics, clinic and research, Department of radiotherapy, AMC 3 Radiation-oncologist, Department of radiotherapy, VUmc 2 Background and expertise During proton therapy treatment the patient’s anatomy changes on the time scale of seconds (respiration, swallowing), minutes (e.g. filling of bladder), days (positioning of patient, organ movements) and of weeks (tumor response to treatment, weight loss). The determined range of protons makes the treatment sensitive to such changes, affecting the quality of the delivered dose distributions, and ultimately reducing the effectiveness of the therapy and increasing its toxicity. Ways to minimize the influence of these anatomy changes include i) image guided proton therapy and ii) adaptive proton therapy. The aim of the IGAPT research line is an integrated strategy to minimize the effect on the delivered dose of anatomy and position changes, while simultaneously improving the workflow. APTC brings together the expertise of three active research groups in the areas of image guidance and adaptive radiotherapy. The AVL has an extensive track record in the development and valorization of new Cone Beam CT (CBCT) reconstruction techniques, advanced correction strategies, and adaptive therapies. VUmc has research lines in Digital Tomosynthesis (DTS), adaptive therapy, and extensive experience with the clinical validation of innovative techniques (e.g. dynamic arc therapy). AMC has research lines in deformable registration, plan selection, and embedding fast dosimetric verification in image guided radiotherapy. These complementary areas of expertise in imaging, registration, corrections and implementation will come together and synergize in the IGAPT research line. At APTC an integrated research group will develop and clinically implement image guided and adaptive proton therapy. IGAPT - Aims Optimizing the image quality of in-room imaging tools (including CBCT and DTS) Development and improvement of image registration algorithms tailored to specific IGAPT applications (both in terms of accuracy and speed) Transfer (and improvement) of existing image guided correction strategies available for photon therapy at the three departments to proton therapy Development of strategies for selection of those patients who will benefit from adaptive planning Development of plan adaptation strategies Development of an effective treatment strategy which actively compensates for respiration to improve the quality of IMPT for moving targets A.2.5 CITE: Treatment planning Dr. A. Bel1, Prof. Dr. M. van Herk2, Dr. W. Verbakel3 1 Head physics, department of radiotherapy, AMC Head physics research, AVL; professor medical physics, University of Amsterdam 3 Medical physicist, department of radiotherapy, VUmc 2 Background and expertise For several years now an extensively researched area in the field of treatment planning for conventional radiotherapy has been automatic plan calculation. The aim is to automatically identify the plan that achieves optimal sparing of organs at risk without compromising the dose delivered to the planning target volume (PTV). For the involved normalorgans/tissues a good description of the Normal Tissue Complication Probability (NTCP) is essential, describing the relation between a specific dose parameter and the risk of developing a predefined type and grade of toxicity. VUmc has a research line for automatic planning for photon therapy. AVL has active research lines in Pareto-optimal planning and probabilistic planning. The AMC brings in experience in the field of new planning techniques for moving organs and fast dose computations, as well as quantification of organ mobility and deformation. These complementary research lines come together at APTC to develop new planning and optimization techniques for proton therapy that are sufficiently robust to result in sparing of healthy tissues not only in silico but also in clinical practice, taking into account positional uncertainties and anatomical variations. Treatment Planning - Aims Improve the accuracy of proton therapy planning by combining the information provided by CT, CBCT and MRI images Automated proton therapy planning Improving robust planning algorithms for a range of indications using the combined retrospective data sets available at the three radiotherapy departments To incorporate biological effects of radiation therapy for organs at risk into treatment planning, to allow for plan comparisons between various treatment modalities A.2.6 CITE: Efficiency and effectiveness Prof. Dr. Wim van Harten1, Drs. Delphine Constant2, Prof. Dr. Richard Boucherie3, Prof. Dr. Coen Rasch4, Prof.dr. B.J. Slotman5 1 AVL/Professor at School of Management and Governance, University of Twente Head department Quality and Process Innovation, AMC 3 Center for Healthcare Operations Improvement & Research, University of Twente 4 Head radiotherapy department, AMC 5 Head radiotherapy department, VUmc 2 Background and expertise Proton therapy requires substantial investments, making proton therapy a costlier treatment modality than conventional radiotherapy. The cost effectiveness of proton therapy is often uncertain, whereas there is clear potential for efficiency improvements in the proton therapy workflow. The aim of this research line is to investigate the cost effectiveness of proton therapy, and to improve this through increase of the efficiency of the proton therapy workflow. The capacity of a proton therapy center depends on many factors, including beam availability, variations in treatment duration, complexity of workflow, and time needed for maintenance. Optimization of referral procedures, external and internal workflows, patient logistics and treatment strategies will increase this capacity. To realize this increase this research line will start a program of data collection, analysis, redesign and adjustments in the logistic process based on mathematical algorithms. In parallel clinical data will be used to compare cost effectiveness between proton therapy and conventional radiotherapy with photons. The researchers at APTC will collaborate with the Department of Kwaliteit en Procesinnovatie (KPI; ‘Quality and Process Innovation) at AMC, the departments of Phsyso-Oncology and Epidemiology of the AVL, and the research center CHOIR (Center for Healthcare Operations Improvement and Research) of the University of Twente. They provide complementary expertise in the fields of efficiency and effectiveness analysis and improvements. KPI has supervised and implemented process optimizations in various clinical departments, including radiotherapy and radiology. CHOIR develops logistical solutions in health care and have developed and publish a range of solutions with respect to patient logistics. Efficiency and Effectiveness - Aims Optimizing the workflow from the multi-disciplinary consult meeting to imaging, planning, plan comparison, positioning and actual treatment Development of efficient and robust algorithms for patient scheduling Development of models to determine, a priori, the potential benefit of proton therapy over other radiotherapy treatment modalities Reduction of average treatment time through image guided patient position correction strategies and research into the potential of using increased beam intensity and continuous beam scanning Implementation of hypo fractionation treatment protocols for a wider range of indications Financial economic evaluation of a proton therapy center through a cost effectiveness analysis comparing the total incremental costs and health benefits for patients treated with protons with those for patients treated with photons