* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Nephron - Amazon S3
Survey
Document related concepts
Transcript
Nephron
The functional units of the kidneys are called nephrons. We will cover
the anatomy and physiology of the nephrons in the next section. To
understand how different regions of the nephron are able to have
unique, spatial functions, we will first discuss how the multicellular
epithelial structures found in these structures are organized for specific
functions.
Nephrons are made up of epithelial cells with an underlying non-cellular
layer or basement membrane that separates the filter in the lumen fluid
from the interstitial space. These epithelial cells differ in cellular
anatomy along the length of the nephrons according to the filtering and
processing functions of the epithelial cells.
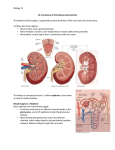
Functional Urinary Tissue – The Nephron
As the chief functional organ in the urinary system, the kidneys excrete
nitrogenous wastes and are involved in regulating the volume,
composition, and pH of the blood. The kidneys receive one fourth of
total cardiac output, a reflection of their function as blood processors.
Each kidney contains about one million nephrons, the structural and
functional units of the kidneys. Each nephron is made up of a highpressure capillary bed called a glomerulus and a renal tubule, segments
of which included a proximal convoluted tubule, nephron loop (loop of
Henle), and distal convoluted tubule. The distal convoluted tubules from
multiple nephrons join a common collecting duct. The nephrons are
involved in three functions: filtration, reabsorption, and secretion.
Overview of the Nephron Structure
The structure within each nephron that actually filters blood plasma is
the renal corpuscle containing the glomerulus and glomerular
capsule. Another nephron structure called the renal tubule receives
the filtered fluid, called glomerular filtrate. Very thin and a little
over an inch long, the renal tubule has three major consecutive
segments that the filtrate flows through: a proximal convoluted
tubule the nephron loop(loop of Henle), and a distal
convoluted tubule.
Nephron Functions
Nephron
Structure
Function
Description
Glomerulus
Filtration
The glomerulus is a capillary network found in close
proximity to the nephron that filters plasma into the
nephron.Proteins and blood cells are retained in the
glomerular capillary.
Tubules
and
nephron loop
(loop of Henle)
Reabsorption Epithelial cells actively transport some substances
from the tubular fluid back into blood. Other
substances, such as water, are passively reabsorbed in
some segments.
Capillaries
specifically
Peritubular
Secretion
Epithelial cells actively secrete certain substances from
the blood into the tubular lumen.
Collecting duct
Collection
Accumulates any material that is not returned to blood
in the preceding segments. Secretes or reabsorbs H+,
HCO3+, and K+ ions. Reabsorbs water under the
influence of anti-diuretic hormone. Anything left in the
distal end of the collecting duct will l be excreted as
urine
The Glomerulus
The renal corpuscle is made up of a tangled capillary network called
a glomerulus and a cup-shaped structure called the glomerular
capsule (Bowman's capsule) surrounding the glomerulus. The
glomerular capsule has an external parietal layer made of simple
squamous epithelium. Although this layer is not involved in the
production of filtrate, it helps to maintain the shape of the capsule. An
inner visceral layer adheres to the glomerular capillaries and is
composed of a special type of simple squamous epithelial cells
called podocytes. These podocytes have multiple projections called
pedicels or foot processes. The pedicels of one podocyte interlock with
the pedicels of adjacent podocytes. Filtrate from the glomerulus passes
through filtration slits, the openings between the foot pedicels, to enter
the capsular space(Bowman's space), the area between the
visceral and parietal layers of the glomerular capsule.
The Proximal Convoluted Tubule
The proximal convoluted tubule (convoluted refers to the coiled shape)
tubule connects the glomerular capsule to the nephron loop. The apical
surface of the simple cuboidal epithelial cells making up the proximal
convoluted tubule are covered in microvilli producing a brush border.
The brush border and the length of the proximal convoluted tubule
dramatically increase the luminal surface area available for reabsorbing
water and solutes and for secreting substances into the filtrate.
The Nephron Loop
The renal corpuscle, the proximal convoluted tubule, and the juncture
between the proximal convoluted tubule and the nephron loop are
located in the renal cortex. The first part of the nephron loop, the
descending limb of the nephron loop, drops into the renal medulla. In
the renal medulla, the loop makes a sharp, almost 180-degree turn back
toward the renal cortex as the ascending limb of the nephron loop.
The ascending limb is continuous with the distal convoluted tubule. The
ascending and descending limbs of the nephron loop have two distinct
parts: a thin section of the limb and a thick section of the limb. In the
thin section of the limb, the diameter of the tubule is distinctly smaller
than the diameter of the rest of the nephron tubules. In the thin sections
of the limbs, the epithelium is thinner simple squamous epithelium that
is permeable to water. In the thick sections of the limbs, the epithelium
is simple cuboidal epithelium that is highly impermeable to water.
Regardless of being in the thin or the thick segments, the lumen is the
same size as the lumen in the rest of the renal tubule.
Distal Convoluted Tubule
The final segment of the nephron is the distal convoluted tubule. As the
ascending limb of the nephron loop reaches the renal cortex, it becomes
the distal convoluted tubule. The distal convoluted tubule extends to the
collecting tubule, the short connection with a collecting duct. The distal
convoluted tubule is composed of simple cuboidal epithelium with very
few microvilli and no brush border.
Capillaries of the Nephron
The glomerulus is not the only capillary bed associated with
nephrons. Peritubular capillaries are branches of the efferent
arterioles that drain the glomeruli and recover most of the filtrate
produced in the renal corpuscle. Glomerular capillaries differ from other
capillary beds in the body, because they are both supplied by and
drained by arterioles. The feeder afferent arterioles are branches of
the cortical radiate arteries. The draining efferent arterioles branch into
the peritubular capillary network around the proximal and distal
convoluted tubules or the vasa recta around the nephron loop. The
diameter of the draining efferent arterioles is smaller than that of the
afferent arterioles, giving the efferent arterioles higher resistance.
Because of this, the glomerulus has a high blood pressure that allows it
to filter high volumes of fluid and solutes out of the blood and into the
glomerular capsule. The nephrons segments reabsorb approximately 99
percent of this filtrate. The peritubular capillaries adhere to neighboring
convoluted tubules and drain into neighboring venules. These lowpressure and porous capillaries easily reabsorb the water and solutes
that the tubule recovers from the filtrate. In some nephrons, rather than
breaking up into peritubular capillaries, the efferent arterioles form
clusters of thin-walled vasa recta. Important for the formation of
concentrated urine, the vasa recta are long, straight capillaries that
reach deep into the medulla alongside the longest nephron loops where
they can collect reabsorbed substances from the loop segments.
Because blood in the renal circulation flows through two arterioles
(where a majority of the manipulation of vascular resistance is found),
renal blood pressure drops from about 95 mm Hg in the renal arteries to
less than 10 mm Hg in the renal veins. Resistance in the afferent
arterioles fluctuates in order to help maintain a relatively constant
glomerular capillary hydrostatic pressure even if there are substantial
changes in systemic blood pressure. The resistance of the efferent
arterioles also contributes to maintenance of glomerular capillary
hydrostatic pressure and also contributes to a low hydrostatic pressure
in the peritubular capillaries.
Specialized Cells Associated With the Nephron
In all nephrons, the last part of the ascending limb of the nephron loop
transitions into the distal convoluted tubule and comes in contact with
the afferent arteriole supplying the renal corpuscle. In this region the
columnar epithelial cells at the beginning of the distal convoluted tubule
are very crowded, leading to the name macula densa ("dense spot").
The macula densa is believed to monitor sodium chloride concentration
of the filtrate entering the distal convoluted tubule. The wall of the
afferent arteriole that is adjacent to the macula densa contains granular
cells (also known as juxtaglomerular cells ). The granular cells
produce and secrete the enzyme renin and are also capable of
contracting when stimulated. These cells and the macular densa make
up the juxtaglomerular apparatus. The action of the
juxtaglomerular apparatus helps control glomerular hydrostatic
pressure by sending signals to the afferent arteriole. There are also
special smooth muscle cells called intraglomerular mesangial cells in in
the spaces between the loops of the glomerulus. These cells help regulate
blood flow through the glomerulus.
Collecting Ducts
As the functional units of the kidneys, the primary role of the nephrons
is to filter plasma, reabsorb what the body would like to keep, and
excrete the rest. Any substances not reabsorbed in the tubules of the
nephrons flows into one of thousands of collecting ducts in the
kidney. A short collecting tubule forms the juncture between a distal
convoluted tubule and a collecting duct. Each collecting duct receives
fluid from several nephrons and then transports it to the renal pelvis.
The collecting tubules and ducts have two types of cells: intercalated
cells, cuboidal cells with plentiful microvilli, and the more
populous principal cells, cuboidal cells with limited, short microvilli.
Principal cells help maintain water and sodium and potassium ion
balance in the body. Intercalated cells help regulate the acid-base
balance of the blood.