* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Vertigo Care Pathway
Survey
Document related concepts
Transcript
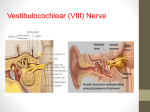
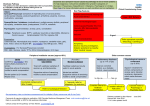
Vertigo Care Pathway Tower Hamlets Adult Care Pathway: For use in Primary Care January 2012 Vertigo Care Pathway for Tower Hamlets Background: Vertigo is a form of dizziness with an illusion or hallucination of movement. The broader term dizziness includes unsteadiness, lightheadedness, motion intolerance, imbalance, floating, or a tilting sensation. Balance is maintained by information from the vestibular apparatus (15%), vision (70%) and proprioception (15%) being processed by the brain. Vertigo is caused by peripheral causes in 80% of cases. Central causes are more common in elderly. A full-time GP may expect to encounter 10-20 cases of vertigo each year. 1 History: • Is there a rotatory element? Constant or episodic? • Duration of episode : seconds, minutes, hours and days • Otological symptoms ( e.g. hearing impairment, tinnitus, otorrhoea) • Associated symptoms (e.g., nausea or vomiting) • Neurological symptoms (including diplopia, dysarthria, dysphagia, focal weakness, autonomic symptoms, headache) • Triggers for vertigo (change of head position, menstrual cycle) • Past medical history, Drug history , Social history Examination: Otological examination: for signs of infection or inflammation Hallpike test should be performed if vertigo is positional (see below for details) Tuning fork test for hearing to ascertain whether hearing loss is conductive or sensorineural (SNHL) Neurological examination: neck movements, eye movements and nystagmus, stance and gait (Romberg’s test, heel to toe walking), cerebellar signs, cranial nerves and PNS as required Systemic examination: Vital signs including supine and standing blood pressure if syncope is suspected, cardiovascular and respiratory system assessment 2 Red Flags: headache, neurological symptoms and signs, irregular pulse (consider cardiac arrhythmia), history of cervical spine or head trauma. Refer to neurology if central cause is suspected: e.g. CVA, Tumour, Multiple sclerosis (MS). Such cases will almost invariable have more symptoms than just vertigo and will usually have neurological signs. Elderly (>75) – Patients often have multiple pathologies. Visual and proprioceptive abnormalities can lead to de-compensation from previous vestibular failure. The elderly are often taking several medications. Chronic vertigo should not be treated with vestibular sedative such as prochlorperazine as this impairs compensation. This group may need assessment in the Falls Clinic if they fit the criteria (see local guidelines for referral criteria) Is there any associated Deafness with the Vertigo? Yes No Meniere’s: Acute Labyrinthitis: Vestibular neuronitis: Benign Paroxysmal Unexplained episodic Lasting hours with tinnitus Acute onset of vertigo lasting days Acute onset lasting days or Positional Vertigo vertigo AND deafness. or weeks WITH deafness. weeks WITHOUT hearing loss. (BPPV): Typically first symptoms Due to inflammation of the Vertigo in certain head occur between ages 20-40 labyrinth which includes the Thought to be caused by viral positions, lasting seconds years. cochlea and the semicircular infection of the vestibular nerve only. 15% may have history canals. of relatively minor head trauma. Clinical features include Acute episode from bacterial or Abrupt onset of severe Observing nystagmus Migraine with or vertigo (<24hours), viral infections associated with debilitating vertigo with during a provoked without aura is the hearing loss (reversible hearing loss, nausea and vomiting. unsteadiness and nausea and manoeuvre confirms most common cause sensorineural), Can be associated with bacterial vomiting. BPPV in typical history. of otherwise Tinnitus (fluctuating). processes such as otitis media or unexplained episodic Aura of fullness or meningitis. Should NOT have hearing loss, Hallpike’s Positional Test vertigo lasting hours: pressure in the ear or side multi-directional non-fatiguing – provoke vertigo with - it may or may not be of the head Useful to establish if conductive or nystagmus (suggesting central geotropic (towards the associated with sensory nerve hearing loss. If cause), high fever, or mastoid ground) torsional headache Abnormal homeostasis of tuning fork test is not conclusive tenderness nystagmus which - look for a family inner ear fluid. Also known then needs an audiogram. habituates on repeated history and as primary endolymphatic Common in 4th and 5th decades. tests (see below). phonophobia or hydrops. Affects men and women equally. photophobia. Over diagnosed in General Preceded often by an URTI. Other causes: Practice. Labyrinthine fistula, cervical vertigo (cervical spine OA related), Autoimmune inner ear disease. 3 Refer to ENT for diagnosis. Treatment for acute episodes consists of: Antihistamines e.g. cinnarizine Phenothiazines e.g. prochlorperazine (not for longer than 7 days). Betahistine hydrochloride can also be helpful (vasodilatation to inner ear) Reduction in dietary salt, caffeine, alcohol and tobacco is advised. Meniere’s is a diagnosis of exclusion, since other pathologies such as acoustic neuroma and otosyphilis may cause same symptoms. (secondary endolymphatic hydrops) If patient presents with sudden onset hearing loss (SNHL), refer to ENT as an emergency and start on high dose steroids such as Prednisolone 40mg. Steroids can be considered up to 2 weeks after sudden onset SNHL. Phenothiazines e.g. prochlorperazine – to manage acute symptoms of vertigo (not for longer than 7 days). Antibiotics may be required if suspected bacterial cause. If middle ear effusion may need tympanotomy. Bacterial infection is indicated by a painful discharging ear with signs of middle ear infection or chronic suppurative otitis media (CSOM). Antihistamines e.g. cinnarizine Phenothiazines e.g. prochlorperazine – should not be given for more than 7 days as patient loses capacity for central vestibular compensation affecting long-term recovery. Symptoms usually recover within 6 weeks. Consider referral to ENT If symptoms persist beyond 4-6 weeks. Vestibular rehabilitation therapy For chronic vertigo. Gaze stabilization exercise Balance and gait training (This will be through Audiology department – Direct Referral process is being explored) Canalith Repositioning manoeuvre – Epley’s Manoeuvre (see below): - used for BPPV - approximately 80% of patients can have symptom resolution with one or more sessions. Refer to ENT if uncertain of the diagnosis. Vestibular rehabilitation exercises: Home exercises include BrandtDaroff exercises (see below). Consider referral to ENT if symptoms persist beyond 4-6 weeks Vestibular rehabilitation therapy for chronic vertigo. (This will be through Audiology Department direct referral process is being explored). 4 Hallpike’s positional test Provokes dizziness and a typical geotropic upbeat torsional nystagmus is diagnostic of BPPV: With the patient sitting, the head is turned 45 degrees to one side. The patient is then placed supine rapidly; so that the head hangs over the edge of the bed (it is perfectly acceptable to lie the patient flat without extending their neck particularly if there are concerns about the neck). Keep in this position for at least 30 seconds. If no nystagmus occurs, they are then returned to the upright position and observed for another 30 seconds for nystagmus. The manoeuvre is repeated with the head turned to the other side. Nystagmus usually appears with a latency of a few seconds and lasts less than 30 seconds. It has a typical trajectory, beating torsionally, with the upper poles of the eyes beating towards the ground. After it stops and the patient sits up, the nystagmus will recur but in the opposite direction. 5 Further Reading/Resources 1.http://eng.mapofmedicine.com/evidence/map/dizziness2.html 2. Turner B, Eynon-Lewis N. Systematic approach needed to establish cause of vertigo. Practitioner 2010;254(1732): 19-23 3. www.vestibular.org – The vestibular disorder association provides support and advice for patients and healthcare professionals. 4. Epley’s manoeuvre: http://emedicine.medscape.com/article/791414-treatment , http://www.youtube.com/watch?v=NQr7MKJBAJY&feature=related 5. Brandt-Daroff exercises, patient leaflet: http://www.croftonandsharlston.co.uk/Leaflets/Brandt-Daroff.pdf 6. http://www.dizziness-and-balance.com/disorders/bppv/bppv.html 7. Patient information leaflets: http://www.patient.co.uk/health/Labyrinthitis-and-Vestibular-Neuritis.htm , also available on Mentor within EMIS and also: http://www.patient.co.uk/health/Benign-Paroxysmal-Positional-Vertigo.htm, again within Mentor on EMIS Local Referral pathway: 1. Department of ENT, Barts and The London NHS Trust - appointments booked via Choose & Book system. Urgent Cases discussed with on-call ENT. 2. Department of Neurology, Barts and The London NHS Trust – appointments booked via Choose & Book system. Urgent Cases discussed with on-call medical consultant. 3. Falls Management Team, Services for Older people and Rehabilitation, Bancroft Unit Mile End Hospital Fax: 0207 377 7844 6 This care pathway is not a full evidence based guideline and is aimed as a care pathway to guide referral decisions by Tower Hamlets GPs. Acknowledgements Written by: Dr Ali Ahmed-Shuaib ([email protected]) with advice from Dr Victoria Tzortiziou Brown ([email protected]), Dr Nicholas Eynon-Lewis ([email protected]) and Dr Kambiz Boomla ([email protected]) Clinical Effectiveness Group | Centre for Primary Care and Public Health | Blizard Institute Barts and The London School of Medicine and Dentistry | Yvonne Carter Building 58 Turner Street | London E1 2AB | Phone: 020 7882 2553 | Fax: 020 7882 2552 email: [email protected] | www.icms.qmul.ac.uk/chs/ceg/ 7