* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download TEC -CONTROL
Survey
Document related concepts
Transcript
Laboratory 2: Kit Preparation and Chromatography
PART 1: KIT PREPARATION
Introduction
In nuclear medicine, radionuclides are rarely used in their simplest chemical form.
Instead they are incorporated into a variety of chemical compounds that take advantage
of important biochemical, physiologic, or metabolic properties. A chemical compound
tagged with a radionuclide and prepared in a form suitable for human use is known as a
radiopharmaceutical. The authority to regulate and approve for human use the
pharmaceutical component lies with the United States Food and Drug Administration
(FDA). The United States Nuclear Regulatory Commission regulates the radioactive
component. Most radiopharmaceuticals are used to obtain diagnostic information rather
than to produce therapeutic results, although their use in therapy is increasing. For
diagnostic uses, they are administered in tracer quantities in a single dose and produce no
pharmacologic effects.
Design Considerations for a Radiopharmaceutical
Because a radiopharmaceutical consists of a radionuclide and a biochemical, two
considerations apply in designing or developing a radiopharmaceutical, one relating to
the radionuclide and the other relating to the biochemical.
Selection of Radionuclide
The choice of a radionuclide for imaging purposes is chiefly dictated by the necessity of
minimizing the radiation dose to the patient and the detection characteristics of nuclear
medicine instrumentation. To minimize the radiation dose to the patient, a radionuclide
should have as short a half-life as is compatible with the biological phenomena under
study. For example, a radionuclide with a one hour half-life cannot be used in studies of
physiological or metabolic functions that span days.
A radionuclide should preferably emit a monochromatic (single energy) gamma ray with
energy between 100 and 300 keV. The lower limit of the desired energy range of gamma
rays is arrived at from the consideration of attenuation of gamma rays in the patient. To
be effective, and contrary to x-ray imaging, the photon must have a high probability of
escaping the patient without interaction in order to be a useful imaging photon. This
probability diminishes markedly below 100 keV. The upper limit of the desired energy of
the gamma ray is the consequence of the detection characteristics of the scintillation
camera (Module 2.2) routinely used to image diagnostic radiopharmaceuticals. The NaI
crystal must be thin (about 3/8 inches thick) to provide sufficient image sharpness and the
collimator must have many holes separated by septa thin enough to yield good spatial
resolution. If too energetic, the photons penetrate thin septa and ruin the image quality.
Photon energies above 300 keV do not render quality images. (Do not confuse this with
Lab#2 Kit Prep and Chromatography (Last Update: February 2014)
Page 1 of 9
positron emission tomography imaging where no physical collimator is used. Imaging
apparati for 511 keV annihilation radiation are very different from conventional gamma
camera imaging.) In addition, a radionuclide should be available easily, economically and
in an uncontaminated form. Technetium-99m with its 6 hour half-life and 140 keV
gamma emission along with its easy economical availability from a generator comes very
close to ideally fulfilling the above requirements. This accounts for its wide use in
nuclear medicine.
Selection of a Chemical
Besides being nontoxic in the desired amounts, the choice of the biochemical or
pharmaceutical substance in the radiopharmaceutical is dictated by the requirement that it
be distributed or localized in the desired organ or biological compartment and that the
uptake by that organ in a normal condition differs substantially from the uptake in a
pathological condition. This is generally expressed as the target-to-non-target ratio. The
higher the ratio, the higher the contrast in the image and easier it becomes to visualize a
disease.
To help in the selection of a suitable biochemical, a wealth of information has been
acquired in the field of pharmacology. A number of biochemical variants determine or
affect the distribution and localization of drugs in tissues. Three important determinants
in this regard are route of administration, blood flow to the organ or tissues and extraction
by the tissues.
Radiopharmaceuticals, with few exceptions, are administered intravenously, primarily
because this is the fastest way to introduce a drug into the circulatory system of the body.
Blood flow or perfusion essentially determines the fraction of the administered dose that
will be delivered to a particular organ or tissue during the first transit. Extraction of a
drug or chemical from the circulation and localization in tissue may occur in a number of
ways.
Extraction of Drug or Chemical
Localization Mechanism
Example
Active transport
Thyroid uptake and scanning with iodine
Compartmental
localization
Blood pool scanning with human serum
albumin
Simple exchange or
Bone scanning with labeled phosphates
Lab#2 Kit Prep and Chromatography (Last Update: February 2014)
Page 2 of 9
diffusion
Phagocytosis
Liver, spleen and bone marrow scanning with
colloids
Capillary blockage
Lung scanning with macroaggregates
Cell sequestration
Spleen scanning with damaged RBCs
Receptor binding
Tumor imaging with somatosin receptor
binding indium pentetreotide
Labeling Radiopharmaceuticals with Technetium-99m
Because the half life of Tc-99m is short (6 h), most labeling has to performed locally
(within hours of transport time). The labeling of most chemicals by Tc-99m is achieved
by first reducing pertechnetate to ionic technetium (Tc4+) and then complexing it with a
desired chemical. The common agent used for reducing purposes is stannous chloride (
SnCl2). To label a particular chemical, what typically is done is to introduce a known
activity of sterile and pyrogen-free NaTcO4- into a “kit” vial and, voila, the labeled
compound is ready to use within a few minutes. Colloquially, the street language is
“shoot and shake”; shoot the activity into the vial and shake it to mix the kit. These
commercial kits are sterile and pyrogen-free vials in which all the desired chemicals are
premixed and held together in a lyophilized state under an inert gas atmosphere.
Figure 2.4-01
Lab#2 Kit Prep and Chromatography (Last Update: February 2014)
Page 3 of 9
Technetium Misbehaving
Unbalanced equations of technetium reduction and tagging are shown. The first equation
shows the normal case, where pertechnetate (7+) is reduced (3+, 4+, 5+) by stannous
chloride to enable tagging a pharmaceutical.
The second equation shows the case of air contamination. This generates free
pertechnetate, which accumulates in the stomach and thyroid and salivary glands.
The third equation shows the case of water contamination, generating technetium dioxide
("hydrolyzed technetium") and stannous hydroxide, a colloid. Technetium dioxide will
accumulate in the liver.
Paper chromatography with acetone will show free pertechnetate advancing with the
solvent front. Paper chromatography with saline as the solvent will show technetium
dioxide at the origin and water soluble tracers advancing with the solvent front.
Radiopharmaceutical Quality Control
Labeling efficiency is defined as the percent of total radioactivity present in the kit that is
tagged to the appropriate molecule or compound. The remainder of radioactivity not
tagged is present as a radiochemical impurity. In kits that use SnCl2 as the reducing
agent, radiochemical impurities are, in general, of two forms: free pertechnetate (which is
not reduced) and reduced or hydrolyzed technetium (which was reduced but did not tag to
the compound of interest).
A common method for the detection of radiochemical impurities is thin-layer or paper
chromatography. In paper chromatography, microliter amounts of the prepared kit are
applied to a 3-cm rectangular paper strip at an origin spot. The end of the strip is dipped
in the solvent so that the origin spot is not immersed. The solvent ascends the strip by
capillary action, separating each radiochemical component into different sections on the
strip. Assaying the section of the strip with unbound 99m-Tc separately from assaying the
portion of the strip with the bound 99m-Tc allows for a rough assessment of the
percentage of bound 99m-Tc in the kit solution.
Lab#2 Kit Prep and Chromatography (Last Update: February 2014)
Page 4 of 9
Figure 2.4-02
PART 2: CHROMATOGRAPHY
INTRODUCTION
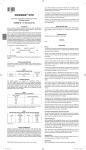
The Tec-Control kit consists of a complete miniaturized chromatography system for
Technetium-99m radiopharmaceuticals. Chromatographic procedures are used to
determine the labeling efficiencies of most Technetium-99m labeled kits. The
chromatography paper to perform rapid and concise separations of hydrolyzed
Technetium-99m (partially reduced) and free Technetium-99m Pertechnetate (unbound
oxidized).
GENERAL INFORMATION
Radiopharmaceutical Spotting
These tests require spotting approximately 10 microliters of the radiopharmaceutical
sample onto the chromatography strip. This is easily accomplished by using a 26 needle
and syringe. One drop equals a volume of 0.01 cc (l0 uL) (one microliter).
Development Aids
Each test strip is ruled on one side with indelible pencil lines indicating the spotting
location and the termination point in the strip development process. For user convenience
the back of each test strip is marked with a soluble dye that will migrate with the solvent
front. The user can easily see the solvent front via the movement of the dye. For reference
there is a color-coded tape at the top of each strip.
Data Analysis
The object of those tests is to determine the percentage of free pertechnetate, the
percentage of hydrolyzed reduced Tc-99m and the percentage of labeled
radiopharmaceutical.
Lab#2 Kit Prep and Chromatography (Last Update: February 2014)
Page 5 of 9
GENERAL COUNTING PROCEDURES
Cut the developed test strip into two sections at the middle pencil line. Using a gamma
scintillation well counter peaked for Tc-99m, individually count each strip section in a
test tube for a specific period of time (i.e., 30 seconds). Count background and calculate
the net counts by subtracting the background counts from the number of counts
previously registered when counting the individual strip sections. Depending on count
rate, the dead time of the detector may give erroneous results.
Solvent Front
4
Tc-99m Chelate
TcO4-
2
TcO4-
1
Tc-99m Chelate
Tc-99m RH
Cut Mark
3
Tc-99m Reduced
Hydro
Origin
Saline 0.9%
Acetone
DETAILED TEST PROCEDURES
For determining free pertechnetate in Tc-99m labeled DTPA, Glucoheptonate,
Diphosphonate, Pyrophosphate, Polyphosphate and MDP.
1. Prepare one developing vial by adding 1 cc to the “red acetone” labeled solvent to the
red label vial.
2. Using a red chromatography strip, spot approximately 10 uL of the test sample onto
the bottom pencil mark line of the test strip.
3. Immediately place the test strip into the red vial containing acetone and develop until
the solvent front migrates to top pencil line.
5. Remove strip from the vial and allow to dry.
6. Cut strip at central pencil line, producing sections 1 and 2.
7. Count each section for activity (per unit time) using
a gamma counter (a dose calibrator can be substituted) and subtract backgrounds.
Lab#2 Kit Prep and Chromatography (Last Update: February 2014)
Page 6 of 9
% free pertechnetate =
=
net cts section 2
(net cts sec 1)+(net cts sec 2)
x 100
For determining hydrolyzed reduced Tc-99m in Tc-99m labeled DTPA,
Glucoheptonate, Diphosphonate, Pyrophosphate, Polyphosphate and MDP.
8. In a clean, black labeled vial place approximately 1cc of the black labeled (distilled
water) solvent
9. Select one strip of the black chromatography paper and spot approximately 10
microLiters of the test compound onto the bottom pencil line.
10. Immediately place the test strip into the black labeled vial containing distilled water
and develop until the solvent front migrates to top pencil line.
11. Remove the strip from the vial and allow to dry.
12. Cut strip at center pencil line into sections 3 and 4.
13. Count both sections for activity (per unit time) using gamma counter and subtract
backgrounds.
% hydrolyzed reduced Tc-99m =
=
net cts section 3
(net cts sec 3)+(net cts sec 4)
x 100
Lab#2 Kit Prep and Chromatography (Last Update: February 2014)
Page 7 of 9
For determining percent labeling in Tc-99m labeled DTPA, Glucoheptonate,
Diphosphonate, Pyrophosphate, Polyphosphate and MDP.
% labeling radiopharmaceutical =
100 % =
% free
pertechnetate
-
% hydrolyzed
reduced Tc-99m
Lab#2 Kit Prep and Chromatography (Last Update: February 2014)
Page 8 of 9
Resident Name (print): ________________________________
Date: ___/___/_____
Signature of individual supervising lab: _______________________________
Name of preparation kit used: _________________________
Under the Dosages and Administration section what is the average adult suggested dose
in millicuries? __________
From the Radiation Dosimetry section what is the organ with the highest radiation dose?
________________
Why is stannous fluoride (SnF2) in the vial? _______________________
Why is nitrogen put in vial? ______________________
In the Direction for Preparation what is the acceptable volume (mL) range for Sodium
Pertechnetate? ________________________
What common technique used to facilitate removing liquids from a vial will change the
chemical state of Sodium Pertechnetate? _______________________________________
What was the stated activity (mCi), volume and calibration time for the Sodium
Pertechnetate?
Calibration date and time _____________
Activity _______________
Volume _______________
Activity per mL _________
Using the Physical Decay Chart what is the current activity? ________________
Assay Sodium Pertechnetate in dosecalibrator: __________________ mCi
How much volume of the above Sodium Pertechnetate solution is required to reconstitute
the vial to make the kit for one adult dose? ___________ mL
How much volume of the above Sodium Pertechnetate solution is required to reconstitute
the vial to make the kit for one child who weighs 35 kg? ___________ mL
In the Direction for Preparation what is the maximum time the preparation is good?
_____ hr
Turn in a copy of this page only into the Physics and Education Offices for
credit.
Lab#2 Kit Prep and Chromatography (Last Update: February 2014)
Page 9 of 9