* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Indigenous Unknowns Lab Report Introduction
History of virology wikipedia , lookup
Quorum sensing wikipedia , lookup
Infection control wikipedia , lookup
Microorganism wikipedia , lookup
Phospholipid-derived fatty acids wikipedia , lookup
Anaerobic infection wikipedia , lookup
Disinfectant wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Marine microorganism wikipedia , lookup
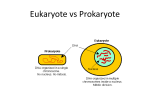
Bacterial cell structure wikipedia , lookup
Triclocarban wikipedia , lookup
Human microbiota wikipedia , lookup
Indigenous Unknowns Lab Report Introduction: Normal flora, which make up about 90% of the cells of a human body, are microbes that live and grow on the body without causing disease under normal conditions. Many of these bacteria simply live on the body without harming or helping it, but many of the bacteria that inhabit the body can also protect us against other bacteria that may grow and cause disease. The purpose of this experiment was to swab the skin, nose, and throat to see what bacteria are present in each of these bodily environments, and then to choose three colonies and identify these bacterial species using a dichotomous key and a series of biochemical tests. The identification of normal flora can be beneficial in the case of an opportunistic infection. If one of the body’s own normal flora is given the right conditions, such as increased growth or a weakened immune system, it can cause an infection. In this case if an infection results from one of the body’s own flora, it may be necessary to identify the organism in order to decide which antibiotic to use. Each individual person has their own unique combination of microbes living on them as normal flora, but there are certain genera that are commonplace in certain body locations. Of the places that were observed in this experiment, the skin and the nose generally have the same genera. These species include Corynebacterium, Micrococcus, Staphylococcus, and Proprionibacterium. The bacteria in the throat are generally different from those on the skin because they live in a different environment under different conditions. These bacteria include Fusobacterium, Haemophilus, Lactobacillus, Neisseria, Staphylococcus, Veillonella, and the most common inhabitants of the oropharynx are species of the Streptococcus genus. In this experiment, a dichotomous key and biochemical tests were used to identify one species from each of the environments that were swabbed (1). Methods: To begin this experiment, five swabs were used to take bacteria from the skin, nose, and throat. The swab was dipped in sterile water and the back of the hand was swabbed then heavily inoculated onto the primary area of a blood agar plate. This was then done for the inside of the nares. To swab the back of the throat, the swab was not dipped in sterile water as the environment is already moist, and the blood agar plate was inoculated in the primary area. Then an inoculating loop was used to finish streaking out each of the blood agar plates. After these plates were allowed to incubate, five colonies were chosen out of all the colonies from the three plates combines. Two colonies from the skin plate were used, one from the nose plate, and two from the throat. These five colonies were then narrowed down to the three bacteria to be identified: two from the skin and one from the throat. The blood agar plates were observed for hemolysis and gram stains were performed. A catalase test was done on each bacterial species by placing a colony onto a slide using a sterile stick, and then dropping hydrogen peroxide onto the colony. All three bacteria were also streaked onto MacConkey and CNA plates using an inoculating loop (2). Next, an anaerobic test was done by streaking skin bacteria #1 onto two plates, and one plate was put right into the incubator while the other plate was put into an anaerobic chamber that was placed in the incubator. Three CTA carbohydrate tubes were inoculated with the skin bacteria: sucrose, maltose, and mannitol, and this was done by using the loop to inoculate the bacteria into the carbohydrate tube. A modified oxidase test was performed by using a stick to pick up a single colony and place it onto a microdase disk. A nitrate test was performed by inoculating a nitrate reduction tube. Then after the tube had been incubated for 24 hours, 10 drops of reagents A and B were added to the broth. An esculin tube was also inoculated, as well as a coagulase tube, by using a loop to inoculate the bacteria into the broths. A urease slant was also done by streaking the slant with bacteria using a loop. An arginine dihydrolase test was done by inoculating a Moeller decarboxylase tube as well as an arginine tube with bacteria and putting a layer of mineral oil in each of the tubes. A mannitol salt agar plate was also used by streaking down the middle and then crossing over the first streak several times. Finally, a DNAse plate was done by streaking two parallel lines about an inch apart from each other (2, 3). For skin bacteria #2, only two additional tests were performed. A modified oxidase test and a glucose tube were inoculated using the same procedures that were used for the skin species. Finally, for the throat bacteria, mannitol and lactose tubes were inoculated using the previously mentioned procedure. An arginine tube was also inoculated as well as an esculin broth, a nitrate broth, and a urease slant. A DMS deep was also inoculated by taking a needle and stabbing the bacteria to the bottom of the tube (4). Results: First, all three bacteria were streaked onto blood agar, TSA, MacConkey, and CNA plates. On the TSA, skin bacteria #1 appeared as small, white, round colonies that were about 2mm in size, and there was no hemolysis on the blood agar plate because there was no clearing around the individual colonies. When streaked on MacConkey and CNA plates, the bacteria grew on CNA but did not grow on MacConkey. Next, a gram stain was performed on this bacteria, and the bacterial cells were small cocci that were purple and in clusters, making it a gram positive coccus. The catalase test was positive, which was indicated by the production of bubbles after hydrogen peroxide was added to the colony. An anaerobic test was also performed, and because the bacteria grew in the incubator as well as the anaerobic chamber, which means it is a facultative anaerobe or aerotolerant and can grow in both anaerobic and aerobic conditions. The carbohydrate broths that were inoculated with this bacteria all remained red and did not turn yellow, so skin bacteria #1 was negative for sucrose, maltose, and mannitol. After the bacteria colony was put onto the microdase disk for the modified oxidase test, it did not turn purple, indicating a negative result. For the nitrate test, the broth turned a deep red after the addition of both reagents, so this is a positive nitrate result. The esculin test also yielded a negative result because after incubation the broth did not turn black and remained its original color. The organism also does not have urease because the urease slant did not turn bright pink after incubation. The organism tested negative for coagulase because the liquid in the tube remained a liquid and did not solidify. The broth in the Moeller decarboxylase tube turned yellow, indicating that the organism grew in the tube and allowing the arginine test to be interpreted. The organism was positive for arginine because the broth in the tube was purple after incubation. On the mannitol salt plate, the organism grew on the plate but was also able to ferment mannitol salt, indicated by the yellow precipitate around the growth. There was no clearing between the streaks on the DNAse plate indicating that the organism was negative for the enzyme DNAse. These results in collaboration with the dichotomous key allowed the identification of this species to be made as Staphylococcus saccharolyticus (Table 1)(5). For skin bacteria #2, the appearance on the TSA plate was much different than skin #1. The colonies appeared large, round, and yellow, and were 4mm in diameter. On the blood agar plate there was clearing around the growth that did not have a green coloration making it a Beta hemolysin. The gram stain also showed gram positive cocci that were very small. The catalase test for this organism was also positive, and it grew on CNA but did not grow on MacConkey. Finally a glucose test was performed, but because the CTA tube did not turn yellow, the organism does not ferment glucose and its identity is Micrococcus luteus (5). Finally, the throat bacteria looked similar to skin bacteria #1 with the small, white colonies, but these colonies were only 0.5mm in diameter as opposed to 2mm. The blood agar plate had no clearing around the colonies and therefore had no hemolysis. The gram stain also showed gram positive cocci but they were in chains. This organism also grew on CNA but not on MacConkey, and when the catalase test was performed, there were no bubbles indicating that this organism does not produce catalase. The mannitol test produced a negative result because the broth did not turn yellow, but the lactose broth was yellow after incubation, indicating a positive result. The arginine dihydrolase test yielded a negative result because the broth was yellow after incubation (with a yellow control tube). The esculin broth was a dark black color which is a positive test result. The nitrate broth did not turn red after adding the reagents so this means the organism does not convert nitrate to nitrite. The urease tube remained the original color and did not turn bright pink, so the organism does not contain urease. Finally, there was no pigment in the DMS tube and the deep stayed the same color, which means the organism did not produce a pigment. The identity of the organism was determined to be Streptococcus salivarius (Table 3)(5). Table 1: Skin Bacteria #1 TSA Colony Morphology Small, White, Round, 2mm Blood Agar (Hemolysis) Gram Stain Catalase MacConkey CNA Anaerobic Test Sucrose Maltose Mannitol Modified Oxidase Nitrate Esculin Urease Coagulase Arginine Mannitol Salt Agar DNAse Identity of Bacteria Gamma Gram Positive Cocci, Clusters + No Growth Growth + – – – – + – – – + +/Yellow Precipitate – Staphylococcus saccharolyticus Table 2: Skin Bacteria #2 TSA Colony Morphology Large, Round, Yellow, Raised, 4mm Blood Agar (Hemolysis) Beta Catalase + Gram Stain Small, Gram positive Cocci, Clusters MacConkey No Growth CNA Growth Modified Oxidase + Glucose – Table 3: Throat Bacteria TSA Colony Morphology Very Small, Round, White, Smooth, 0.5mm Blood Agar (Hemolysis) Gamma Catalase Gram Stain MacConkey CNA Mannitol Lactose Arginine Esculin Urease Nitrate DMS – Gram Positive Cocci, Chains No Growth Growth – + – + – – – Skin 1: Staphylococcus saccharolyticus Skin #2: Micrococcus luteus Throat: Streptococcus salivarius Figure 1: Gram Stains Discussion: The purpose of this experiment was to swab the skin, nose, and throat for normal flora, and identify these bacteria using biochemical tests and dichotomous key. The results of the gram stain indicate that all three bacteria were gram positive cocci. Because the cells of skin bacteria #1 were arranged in clusters and not chains, this indicates that the genus of this organism may be Staphylococcus rather than Streptococcus. Because MacConkey supports the grown of gram negative bacteria, and CNA supports the growth of gram positive bacteria, this organism is gram positive, confirming the gram stain results, because it grew on CNA and not on MacConkey. The catalase test is crucial in separating the Micrococcaceae from the Streptococcaceae. The Micrococcaceae are all catalase positive and the Streptococcaceae are all catalase negative. This organism must be a Micrococcus or a Staphylococcus because of the positive catalase result. This organism is likely a Staphylococcus because it has small white colonies, and it also can grow anaerobically. The dichotomous key for anaerobic Staphylococci was used to identify this organism. First, the sucrose test was used to narrow down the large group of bacteria to Staphylococcus cohnii, Staphylococcus carnosus, Staphylococcus saccharolyticus, and Staphylococcus caprae. The negative maltose result rules out S. cohnii and S. caprae. Finally, to differentiate between the last two, the mannitol result was used. Because the organism did not ferment mannitol, its identity was determined to be Staphylococcus saccharolyticus. Because this organism is a staphylococcus, it is a common inhabitant of the skin and could likely also be found in the nose. It is normal flora, so it will likely not cause disease unless the immune system is suppressed but in the case of an opportunistic infection, it could cause diseases such as pneumonia or endocarditis (6, 7). Skin bacteria #2 had a similar gram stain to #1, with gram positive cocci arranged in clusters. The grown on CNA but not MacConkey confirmed that this organism was gram positive, and there was beta hemolysis on the blood agar plate. The positive catalase test indicates that this organism is a Micrococcaceae. The yellow colonies suggest that it is a Micrococcus and based on the dichotomous key this narrows it down to just Micrococcus varians and Micrococcus luteus. The glucose test was used to differentiate between these two and because the organism was negative for glucose fermentation, it was identified as Micrococcus luteus. This result is also confirmed by the positive modified oxidase test. M. luteus is an extremely common skin and organism that can also be found in dairy products as well as on dust particles in the air or on surfaces. This organism also generally does not cause disease, but in the case of an opportunistic infection it may cause an infection wherever it is able to grow in higher quantities in the case of an immunocompromised patient (8). Finally, the throat bacteria also appeared as gram positive cocci, but these cells appeared in chains rather than clusters which suggest that they may be Streptococci. Again, the growth on CNA but not on MacConkey confirmed a gram positive organism, and it was narrowed down to Streptococci because it was catalase negative. This narrows it down to the organisms on the Streptococci dichotomous key. The lack of hemolysis narrows the group of Streptococci down to Streptococcus rattus, Streptococcus mutans, Streptococcus ferus, Streptococcus cricetus, Streptococcus sobrinus, Streptococcus salivarius, and Streptococcus milleri. The lack of mannitol fermentation narrowed this group down to just two organisms: S. salivarius and S. milleri. Then, the positive lactose result indicated that the identity of this organism is Streptococcus salivarius. This species is a common oropharyngeal normal flora species that could cause dental plaque or gum disease if allowed to grow and multiply enough in the absence of proper hygiene. The identification process of bacteria is not without flaw and error. An error in inoculation could lead to a false negative if there were no organisms present in the test. A false positive could also result if too much inoculation occurred. Any errors in reading the tests or following the dichotomous key would also affect the results and change the ultimate identification of the organism. Works Cited 1. Eggers, Christian. Isolation of Indigenous Microorganisms. Hamden: Quinnipiac University, 2011. Print. 2. Eggers, Christian. Micrococcaceae. Hamden: Quinnipiac University, 2011. Print. 3. Eggers, Christian. Gram Positive Rods. Hamden: Quinnipiac University, 2011. Print. 4. Eggers, Christian. Streptococcaceae. Hamden: Quinnipiac University, 2011. Print. 5. Leboffe, M. J., and B. E. Pierce. A Photographic Atlas for the Microbiology Laboratory.Englewood, CO: Morton, 2005. Print. 6. Wu, Xiaomei, Chunyan Yu, and Xinyan Wang. "A Case of Staphylococcus Saccharolyticus Pneumonia." International Journal of Infectious Diseases 13.2 (2009): E43-46. Print. 7. Westblom, T. U., Geoffrey J. Gorse, Thomas W. Milligan, and Andrew H. Schindzielorz. "Anerobic Endocarditis Caused by Staphylococcus Saccharolyticus." Journal of Clinical Microbiology 28.12 (1990): 2818-819. Print. 8. "Micrococcus Luteus." Wrong Diagnosis. 29 Apr. 2011. Web. 05 May 2011.<http://www.wrongdiagnosis.com/medical/micrococcus_luteus.htm>.