* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Thymine-requiring Mutants of Proteus mirabilis
Survey
Document related concepts
Childhood immunizations in the United States wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Neonatal infection wikipedia , lookup
Schistosomiasis wikipedia , lookup
Infection control wikipedia , lookup
Transcript
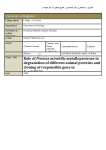
Journal of General Microbiology (1973),77,533-535 Printed in Great Britain 533 Thymine-requiring Mutants of Proteus mirabilis Selected by Co-Trimoxazole in vivo By 0. A. O K U B A D E J O A N D R O S A L I N D M. M A S K E L L The Public Health Laboratory, St Mary's General Hospital, Portsmouth (Received I 9 February I 973) Co-trimoxazole is widely used for the suppression of urinary tract infections (Cattell et al. 1971). The drug contains trimethoprim which can be used in vitro to select thymine-requiring mutants of bacteria (Andrew, I 973). This paper reports the isolation of thymine-requiring mutants of Proteus mirabilis from the urine of patients who were on long-term co-trimoxazole therapy for urinary tract infections. METHODS Routine urine cultures were made by plating a standard loopful on CLED medium (Mackey & Sandys, 1966), and sensitivity tests were performed by the flood-plate method on DST (Oxoid) agar enriched with 5 % lysed horse blood. Mastrings (Mast Laboratories Ltd, Liverpool) were used with antimicrobial agents as follows : nitrofurantoin, 200 pg ; sulphadimidine, 200 ,ug ; tetracycline, 100,ug ; ampicillin, 30 pg; nalidixic acid, 25 ,ug ; and co-trimoxazole, 25 ,ug. All plates were incubated for 18 to 24 h at 37 "C. The organisms were identified as Proteus mirabilis using standard methods (Cowan & Steel, 1966). The mutants were further tested for growth on routine media such as blood agar, MacConkey agar, nutrient broth, and, in addition, on plates of DST agar enriched with 5 "/b lysed horse blood with discs of p-aminobenzoic acid, sulphonamide, nitrofurantoin and co-trimoxazole. The nutritional requirements of the mutants were determined on minimal salts agar (Clowes & Hayes, 1968). Escherichia coli strains w311o (thymine-requiring, supplied by Dr N. Datta, Hammersmith Hospital, London, W.12)and NCTC 10418 (prototroph) were used as controls. RESULTS The mutants of Proteus mirabilis were isolated from the urine of three patients: M. P., a woman aged 27, presented in January 1971 with cystinuria, chronic pyelonephritis and renal calculi. A strain of Proteus mirabilis, sensitive to co-trimoxazole, was isolated from the urine. She was treated with co-trimoxazole (one tablet of co-trimoxazole contains 80 mg trimethoprim and 400 mg sulphamethoxazole), two tablets twice a day for 7 days: the urine became sterile, and the dose was reduced to one tablet twice a day in February, and to one tablet per night in March. Infection with P. mirabilis recurred in May and June 1971;the organisms grew normally and were sensitive to co-trimoxazole, which was then given in therapeutic dose of two tablets twice a day for 2 I days, after which it was reduced to one twice daily. Again the urine became sterile, and the patient was well until September when the infection recurred again. On this occasion the P. mirabilis isolated grew normally on the routine culture medium (CLED) but failed to grow on DST (Oxoid) sensitivity agar, and the sensitivity of the organism could not be ascertained normally. The patient continued to take one tablet twice daily until December 1971,and during this time P. mirabilis was isolated from the urine. On each occasion the organism grew well on CLED, but not on sensitivity agar. In December the co-trimoxazolewas stopped. In February 1972 the patient had a pyelolithotomy under Downloaded from www.microbiologyresearch.org by IP: 88.99.165.207 On: Fri, 16 Jun 2017 20:44:14 Short communication 534 Table I. Growth responses of Proteus mirabilis mirtants Proteus mirabilis strains derived from patients I Medium M. P. K. R. - - MA MA+ thymine ( 2 . 5 pglml) MA+ thymine (25 pg/ml) MA+ thymine (250 pglml) MA+ PABA* ( 2 0 pg/ml) MA + PABA* (1000pglml) MA+ sulphonamide (200 pglml) MA+ trimethoprim (zoo pglml) - Escherichia coli strains A J. F. - +- + +- - - - - - + - - I * p-Aminobenzoic acid. f - A v w31ro - + + +- - NCTCI0418 + + + + + + + + -, No growth; +, growth, and single colonies after 48 h incubation. nalidixic acid cover, and she was discharged without chemotherapy. In March 1972 infection recurred; once again a strain of P. mirabilis was isolated from the urine. This organism grew normally on sensitivity agar. K. R., a woman aged 60, with rheumatoid arthritis and renal calculi, had had urinary tract infections with Proteus mirabilis during 1968, 1969 and 1970. During this time she was treated with various antibiotics. In February 1972 the patient was referred back to hospital with urinary tract infection and a history that she had been taking co-trimoxazole, two tablets twice daily for the previous 1 2 months. The midstream specimen of urine yielded a growth of P. mirabilis which grew normally on CLED, but not on sensitivity agar. In April 1972 the drug was stopped, and in May the P. mirabilis isolated grew normally on sensitivity agar. J. F., a woman aged 44,had bilateral renal calculi and chronic renal failure. Infection was successfully suppressed with co-trimoxazole, one tablet per night from October 1970. In June 1971 Proteus mirabilis infection recurred ; the organism grew normally on sensitivity agar, and was sensitive to co-trimoxazole. The dose was increased to one tablet twice a day for 3 months and then reduced to one per night in September. The patient continued on this dose until December 1971 when infection recurred; the P. mirabilis strain isolated this time did not grow on sensitivity agar. All the Proteus mirabilis strains, including the mutants, grew normally on CLED, MacConkey agar, blood agar and in nutrient broth. However, the mutants did not grow on DST agar enriched with 5 yo lysed horse blood, except in the vicinity of discs containing: p-aminobenzoic acid, 1000pg; sulphonamide, 200 pg; nitrofurantoin, 200 pg; or cotrimoxazole, 25 pg. In nutritional tests the mutants isolated from M. P. and K. R. required high levels of thymine ( > 20 ,ug/ml) for growth. The third mutant from J. F. may have required thymine, but also required some other unidentified factor (Table I). DISCUSSION Thymine-requiring mutants of various organisms, such as Escherichia coli (Okada, Yanagisawa & Ryan, 1960), Salmonella typhimurium (Okada, Homma & Sonohara, 1962), Aerobacter aerogenes (Harrison, I 965) and Streptococcus faecalis (Andrew, I 979, have been selectively isolated using trimethoprim in vitro. Our findings suggest that in vivo selection of thymine-requiring mutants of Proteus mirabilis may occur in the presence of co-trimoxazole, probably due to its trimethoprim content. It is likely that such mutants occur only rarely, because further similar isolates have not been obtained from more than IOO other patients known to have had co-trinioxazole for periods of a year or longer. Enhancement of growth with p- aminobenzoic acid, nitrofurantoin and sulphanomides Downloaded from www.microbiologyresearch.org by IP: 88.99.165.207 On: Fri, 16 Jun 2017 20:44:14 Short communication 535 occurred only in the presence of blood, and the explanation for this is not clear to US. A similar observation has also been made by McGhie, Hutchison and Finch (1972). There are two practical implications of these findings. First, in routine bacteriological work, the failure of an organism such as a Proteus species to grow on sensitivity agar (in marked contrast to its normal behaviour) might lead to its being reported as sensitive to all the agents tested on the sensitivity plate. Secondly, the observation that the mutants grew in the vicinity of sulphonamide and co-trimoxazole discs suggests the possibility that in these patients, co-trimoxazole may be helping to maintain infection rather than suppressing it. This suggestion may be of clinical importance, and can be supported theoretically since it is known that thymine-requiring mutants of Escherichia coli are able to metabolize exogenous thymine (Crawford, 1999, and gain advantage over wild-type bacteria when thymine is present with trimethoprim (Bertino & Stacey, 1966). Andrew (1973) also showed that wildtype Streptococcusfaecalis was able to utilize exogenous thymine to reverse trimethoprim inhibition. It is interesting that I to 3 months after the co-trimoxazole was stopped in two of the patients (M.P. and K.R.), Proteus mirabilis isolated from the urine grew normally on sensitivity agar, suggesting that wild-type bacteria again predominated over thyminerequiring mutants. We are grateful to Professor A. Polak and Dr H. A. Lee for permission to publish details of these patients and to Dr N. Datta for advice and supply of Escherichia coli strain W ~ 10. I REFERENCES ANDREW, M. H. E. (1973). Use of trimethoprim to obtain thymine-requiring mutants of Streptococcus faecalis. Journal of General Microbiology 74, 195-199. BERTINO, J. B. & STACE,Y, K. A. (1966). Suggested mechanism for the selective procedure for isolating thymine requiring mutants of Escherichia coli. Biochemical Journal 101, 326-336. CATTELL, w. R.,CHAMBERLAIN, D. A., FRY,I. K., MCSHERRY, M. A., BROUGHTON, c. & O’GRADY,F. (I97 I). Long-term control of bacteriuria with trimethoprim-sulphonamide. British Medical Journal I, 377-3 79. COWAN,S. T. & STEEL,K. J. (1966). Manual f o r the Identification of Medical Bacteria, p. 78. Cambridge: Cambridge University Press. CLOWES, R. C. & HAYES, W. (1968). Experiments in Microbial Genetics. Oxford : Blackwell. L. V. (1958). Thymine metabolism in strains of Escherichia coli. Biochemica et biophysica aeta CRAWFORD, 30,428-429. HARRISON, A. P. (1965). Thymine incorporation and metabolism by various classes of thymine-less bacteria. Journal of General Microbiology 41,321-334. MCGHIE,D., HUTCHISON, J. G. P. & FINCH,R. G. (1972).Stimulation of growth on a deficient medium of a KIebsiella aerogenes species by sulphonamide, para amino benzoic acid, nitrofurantoin, and some other substances. Journal of Clinical Pathology 25, 976-978. MACKEY, J. P. & SANDYS, G. H. (1966). Diagnosis of urinary infections. British Medical Journal I, I 173. OKADA, T., HOMMA, J. & SONOHARA, H. (1962). Improved method for obtaining thymineless mutants of Escherichia coli and Salmonella typhimurium. Journal of Bacteriology 84,602-603. OKADA, T., YANAGISAWA, K. & RYAN,F. J. (1960). Elective production of thymineless mutants. Nature, London 188,340-341. Downloaded from www.microbiologyresearch.org by IP: 88.99.165.207 On: Fri, 16 Jun 2017 20:44:14