* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Agitated Patient - Modbury On-Line
Survey
Document related concepts
Transcript
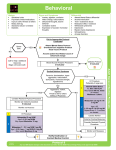
Management of Severe Agitation Key Points 1. The management of the severely agitated or violent patient embraces psychological, physical and pharmacological approaches. 2. Psychological methods focus on controlling the environment through the establishment of communication and trust. 3. Physical measures involve show of force and physical restraint. Physical restraint should always be followed by pharmacological sedation. 4. Pharmacological methods use strong sedatives to control behaviour. Regimes for sedation include : Olanzapine wafer + Oral Lorazepam. IM Olanzapine + Clonazepam IV Midazolam + Haloperidol 5. If restraint is used ensure appropriate procedures for documentation, observations and mental health review are followed. Dealing with a severely agitated or violent patient is an essential skill for clinicians working in the ED or in rural practice. Knowing how to recognise and anticipate the potential for violence is as important as in being able to manage it when it occurs unexpectedly. Particular issues that need consideration when dealing with a violent patient include the protection of yourself, staff and other patients from injury, rapid control of the violence and the presence of underlying disease causing or contributing to the violence. A rapid and well-coordinated approach is required in response to the threat of violence. It relies on both teamwork and the implementation of specific protocols formulated in advance to manage the violence. Too aggressive or too passive a response can result in significant complications for the patient or staff. The response must be proportional and appropriate to the threatened or actual violence. Identifying the Potentially Violent Patient There are number of features which assist in anticipating violence. Most are intuitive and include : Historical features • Past history of impulsive behaviour • Verbalisation about future planned violence • Alcohol and / or drug abuse • Psychotic illness : Paranoid delusions, Suicidal ideation • Past history of personality disorder: Antisocial, Borderline, Paranoid Features on examination • Loud, Aggressive, Insistent speech • Tense posture • Apparent suspiciousness • Restlessness, Agitation ABCDs of Emergency Medicine © Peter Stuart, Jason Bament, 2011 1 Medical Conditions associated with Violence Always view agitation and violence as a symptom of possible underlying medical illness. In a study examining the causes of callout for a violence management team in a major hospital in Australia, organic brain syndrome was responsible for 75% of the calls whilst Psychiatric illness (including affective disorders and psychosis) was responsible for 10%. Personality disorders accounted for the remaining 15%. In the study the most common causes for organic brain syndrome were hypoxia, alcohol intoxication, CNS related (epilepsy, meningitis), alcohol withdrawal and substance abuse. Organic disease and violence are linked and the management should always focus on identifying or excluding underlying disease. Organic diseases that need consideration in the setting of violence include : • Infection (eg CNS, Sepsis) • Metabolic diseases (eg Hypoglycaemia, Liver failure, Renal failure, Hyperthyroidism) • Structural CNS Lesions (eg Intracerebral bleed, Trauma, Subarachnoid Haemorrhage) • Drug related (Overdose, Intoxication, Withdrawal) • Seizure / Postictal causes Important psychiatric causes for violence include psychosis, schizophrenia, affective disorders and personality disorders including antisocial, borderline and paranoid personality disorder. Differentiating Organic From Psychiatric Disease Clinical features that signal the presence of underlying organic disease in a patient with violent behaviour include : • Clouding of Consciousness (drowsy, difficult to rouse) • Altered Cognition (Disorientation, Memory, Poor Serial 7’s) • Abnormal Vital signs • Abrupt onset of symptoms A patient with any one of these features should be assumed to have an organic cause and investigated further. Patients with a past or concurrent psychiatric illness should not be assumed to have a psychiatric cause for their altered behaviour / mental state until an organic cause is ruled out. Other clues from the history and examination that suggest a medical (organic) aetiology include : the presence of visual or tactile hallucinations, a recent history of surgery or hospitalisation, use of prescribed medications and substance abuse and age > 40 years with no past history of psychiatric disease. Management of Severe agitation / Violence The management of the severely agitated or violent patient embraces psychological, physical and pharmacological approaches. Psychological methods focus on controlling the environment through the establishment of communication and trust. Physical measures involve a show of force and physical restraint whilst pharmacological methods use strong sedatives to control behaviour. Where a patient requires restraining, a detention order is generally required. Psychological approach The psychological approach uses an unrestrained technique and is suitable only if there is no immediate danger to the patient or to others. It begins with speaking with the patient using open ended questions (becoming more specific as trust is established), careful observation of the patient’s behaviour and explanation of what is happening and why. Try to diffuse the patient’s anger by acknowledging and exploring their concerns and emotions. It is important to emphasise to the patient your concern for their safety and well being and explain this in the context of the need to perform an examination and investigations (eg “I would like to examine you to make sure you are safe from serious disease”). It is crucial that you consider your personal safety at all times and arrange to have physical assistance nearby. Ensure the patient does not come between you and the exit and that you stay a safe distance (at least two arms length) at all times. Avoid eye contact and maintain a submissive posture. ABCDs of Emergency Medicine © Peter Stuart, Jason Bament, 2011 2 Physical Approach Physical restraint may be required to ensure the safety of patients who are at high risk of suicidal or homicidal ideation or have an underlying organic brain syndrome with altered cognitive state such as possible head injury, meningitis or severe drug intoxication. Where the interview destabilises or if violence is threatened or likely, restraint becomes essential. Methods include a show of force (ie overwhelming numbers of security staff / orderlies) combined with a reasoned explanation of why it is in the interests of the patient to cooperate. If the patient responds it is best to explain the need for and administer medication to assist to calm them. Where the patient does not respond to a show of force the next step is to restrain the patient and apply shackles. First explain to the patient what will happen (eg “we will need to restrain you to protect you from injury”) and then with at least 4 orderlies or security staff approach from 4 directions and secure a limb. Shackle all four limbs to the bed either in the supine, side or prone position and do not remove restraints until it is clear that control is achieved and violence is no longer a threat. Take care to document the reason for the restraint and any verbal threats made by the patient. Once the patient is physically restrained proceed to pharmacological restraint. Do not leave the patient physically restrained without proceeding immediately to chemically restrain the patient. Pharmacological restraint Pharmacological restraint refers to the use of tranquillising drugs to relax and sedate the patient. This is essential to protect the patient from self-harm as a result of their extreme agitation and to allow the clinician to perform an adequate assessment to exclude life-threatening illness. In addition it provides a method for reducing the degree of stress experienced by the patient as a result of their condition. The indications for pharmacological restraint are identical to those outlined for physical restraint and include severe agitation, delusions / hallucinations with bizarre speech or behaviour. If a patient can be talked into taking medications without the use of restraint this is the preferred option. If this is not possible physical restraint is used to temporarily control the situation and permit administration of pharmacological agents. Several options are available for sedation including neuroleptics (eg Haloperidol), Non-Neuroleptic Antipsychotics (eg Olanzapine, Risperidone) and Benzodiazepines (eg Clonazepam, Midazolam, Lorazepam). It has been found that using two agents is preferable to using only one as this reduces the dose of the individual sedating agents and as a consequence reduces the risk for side effects. One approach is outlined below. Oral Sedation Oral : Olanzapine + Lorazepam • Olanzapine wafer (2.5 mg to 20 mg sublingual) • Lorazepam 0.5 mg to 5 mg orally Olanzapine (2.5 – 20 mg SL 4 hourly PRN with a max of 40 mg / 24 hours) is a non-neuroleptic antipsychotic with low cardiotoxicity and little risk of causing extrapyramidal reactions. The wafer preparation dissolves on the tongue and improves compliance. Onset of clinical action is within 5 to 30 minutes and duration of effect is between 4 to 24 hours. Lorazepam (0.5 – 5 mg orally 4 hourly PRN with a max of 20 mg / 24 hours) is well absorbed and has a duration of action varying from 2 to 10 hours. Apart from respiratory depression in high doses it is relatively free of adverse effects. Risperidone (0.5 mg – 2 mg PO 4 hourly PRN with a max of 6 mg / 24 hours) is an alternative to Olanzapine and is available as a tablet or in liquid form and has an onset of action within 10 to 30 minutes with a duration of effect between 6 to 10 hours. Postural hypotension may sometimes be a problem with the initial doses. As with Olanzapine it has a low risk of extrapyramidal side effects and low cardiotoxicity. ABCDs of Emergency Medicine © Peter Stuart, Jason Bament, 2011 3 Intramuscular Sedation Intramuscular : Olanzapine + Clonazepam (or Midazolam) • Olanzapine is administered in a dose of 5 – 10 mg IM • Clonazepam is administered in a dose of 0.5 mg to 2 mg IM • Midazolam is administered in a dose of 2.5 mg – 10 mg IM Olanzapine is a non-neuroleptic antipsychotic with low cardiotoxicity and little risk of causing extrapyramidal reactions. It is administered intramuscularly in doses of 5 – 10 mg. It has a rapid onset of clinical action (within 5 to 10 minutes) and duration of effect is between 4 to 24 hours. Clonazepam or Midazolam are the most appropriate parenteral benzodiazepines and may be administered IM or IV The major side effect is respiratory depression and close observation of the patient is required during this process. Both agents have an onset of action of between 1 and 15 minutes. Clonazepam has a duration of action of 2 to 24 hours while Midazolam has a shorter duration of action of between 1 and 2 hours. Commonly reported side effects with benzodiazepines include ataxia, confusion, memory impairment and paradoxical disinhibition. Intravenous Sedation Intravenous : Clonazepam (or Midazolam) +/- Haloperidol • Clonazepam is administered in a dose of 0.25 IV titrated to response (max 2 mg) • Midazolam is administered in a dose of 1 mg IV titrated to response (max 10 mg) • Haloperidol is administered in a dose of 2.5 mg IV titrated to response (max 20 mg) Clonazepam or Midazolam administered intravenously are the agents of choice for rapid control of the agitated patient where IV access is available. Both may cause respiratory depression and careful titration of the dose is required to ensure breathing is not compromised. Haloperidol If an antipsychotic is required intravenously Haloperidol may be used. It is an older antipsychotic that provides rapid control of agitation and hyperactivity with minimal significant side effects. It is contraindicated in patients with anticholinergic poisoning and is not the agent of choice in patients with head injury (where intubation and hyperventilation should be used) and alcohol withdrawal (where diazepam is the preferred agent). Side effects of haloperidol include confusion, hypotension and anticholinergic effects (hot, dry, visual disturbance, urinary retention, confusion). Haloperidol has a strong propensity for extrapyramidal reactions (acute dystonia : treated with benztropine 1-2 mg IM) and may rarely trigger seizures in a patient predisposed to convulsions. In the cases where rapid control of the patient is required (such as following physical restraint) IV haloperidol is extremely useful as the onset of action is seen within 5 to 10 minutes and repeated doses can easily be given to achieve rapid pharmacological restraint. Although higher doses of Haloperidol may be used safely, in a patient in whom adequate sedation has not been achieved with 20 mg of Haloperidol, the preferred management is to use a benzodiazepine. Give Haloperidol slowly IV in 1 mg - 2.5 mg aliquots (0.5 mg in the elderly). Monitor blood pressure closely as hypotension may occur and is managed with a 250 ml – 500 ml fluid bolus. Haloperidol may also be given orally or IM. ABCDs of Emergency Medicine © Peter Stuart, Jason Bament, 2011 4 Clinical Guideline for Managing Acute Agitation Context Acute agitation has the potential for harm the patient, staff and visitors. A search for the underlying cause of the agitation should be made. If treatable this alone will greatly reduce the risk of harm. If treatment of the cause does not control agitation attempts should be made at defusing the agitation using psychological methods. Where these measures are not successful sedation is indicated. Sedation Regime – Three Options In the following guideline there are three steps of pharmacological intervention. These should be applied according to the clinical context. All patients receiving sedation must be monitored carefully to identify serious side effects including respiratory depression, hypotension or cardiac arrhythmias. Step 1 : Oral Lorazepam + Oral Olanzapine • Oral Lorazepam (1 – 2 mg) May be repeated at 30 minutes if required • Olanzapine wafer (2.5 to 5 mg) May be repeated at 30 minutes if required Step 2 : IM Clonazepam + IM Olanzapine Used where first line therapy not possible or has failed Violence team response should be initiated and an attempt made to de-escalate the situation • IM Clonazepam (0.5 mg – 2 mg) Repeat dose at 15 minutes if required • IM Olanzapine (5 – 10 mg) Repeat dose at 1 hour if required All patients receiving IM therapy must have a nurse special attached to them to monitor their clinical condition. Continuous non-invasive monitoring should be initiated. Step 3 : IV Midazolam + IV Haloperidol This step mandates the presence of a medical officer with advanced airways skills and a high dependency monitored area. Full oxygen saturation, BP, ECG monitoring must be initiated. • IV Midazolam 1 mg Titrate to a maximum of 10 mg. Watch for respiratory depression • IV Haloperidol 2.5 mg Titrate to a maximum of 20 mg. Monitor blood pressure closely All patients receiving IV therapy must have continuous nursing observation and managed in an area with monitoring and resuscitation equipment. ABCDs of Emergency Medicine © Peter Stuart, Jason Bament, 2011 5 Managing the Restrained Patient Where a patient is restrained it is essential that the incident is well documented and that appropriate procedures with respect to the management of restrained patients are followed by medical and nursing staff. All staff should be familiar with these procedures. Principles of restraint A restrained patient should not be left to thrash about in an uncontrolled manner. Poor management of the restrained patient increases the risk of complications from the procedure including rhabdomyolysis, soft tissue injury, fracture, airway obstruction, cardiac arrhythmias and cardiac arrest. Once physical restraint has been performed, sedation will be required to control behaviour and reduce the risk to the patient from injury. All patients that are restrained should be observed regularly with special attention to identifying respiratory depression (secondary to sedation), asphyxia, pressure sores, vascular impairment to extremities and unrecognised underlying organic disease. The risk to the patient from restraint should never be underestimated. Restraint is associated a significant risk of morbidity and mortality. Procedure for restraint Where a patient has been restrained local procedures and policies in relation to documentation, observation and mental health review should carefully followed. In general these will cover the following clinical areas in relation to restraint. Documentation The medical officer should document all episodes of restraint on the clinical record. In particular the medical record indicate : • Clinical issue requiring restraint • Person responsible for initiating restraint • Reason for instituting restraint rather than another intervention (eg open therapy) • Date, time and location that restraint commenced • Specific type of restraint implemented • Anticipated and actual duration of restraint • Status of the patient under the mental health act or guardianship act • Whether the next of kin/family/guardian was notified Observation All restrained patients should have documented evidence of : • Regular Observation (15 minutely is the standard) • Frequent clinical assessment (hourly if feasible) • Removal of restraint to all the limbs for 10 minutes every hour (performed by removing one limb at a time for 10 minutes and then reapplying the restraint and removing another limb for 10 minutes) Mental Health Review Arrangements for mental health review will be required in the case of a patient who has been restrained as a result of mental illness. ABCDs of Emergency Medicine © Peter Stuart, Jason Bament, 2011 6