* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 7: Obstetrics, Gynaecology and Urinary Tract Disorders
Survey
Document related concepts
Pharmacognosy wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Tablet (pharmacy) wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Drug interaction wikipedia , lookup
Prescription costs wikipedia , lookup
Combined oral contraceptive pill wikipedia , lookup
Psychopharmacology wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Transcript
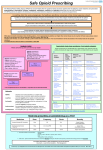
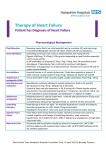
7: Obstetrics, Gynaecology and Urinary Tract Disorders Please select a topic: 7.1 Drugs used in obstetrics 7.3 Contraceptives 7.2 Treatment of vaginal and vulval conditions 7.4 Drugs for genitourinary disorders Changes to the Formulary since previous version (1.7.2013) Section Change Reason for change 7.4 ADDED: Mirabegron Gateshead Medicines Management Committee approval 7.2 REMOVED: Vagifem® 25microgram Product discontinued 7.4 REMOVED: Distigimine Product discontinued 7.4 REMOVED: Doxazosin 4mg and 8mg MR tablets Made non-formulary Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 1 of 15 Date: 22.2.2013 7.1 Drugs used in obstetrics Prostaglandins and oxytocics Carboprost 250 micrograms injection Dinoprostone 3mg vaginal tablets Dinoprostone 10mg/ml extra-amniotic solution Dinoprostone 750 microgram intravenous solution Ergometrine 500 microgram injection Gemeprost 1mg pessaries Oxytocin 10 units/ml injection Syntometrine 1ml injection (containing ergometrine maleate 500micrograms with oxytocin 5units/mL) Mifepristone Mifepristone 200mg tablets Prescribing notes Mifepristone should be ordered in the controlled drug book Myometrial relaxants Atosiban 6.75mg/0.9ml and 37.5mg/5ml injection Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 2 of 15 Date: 22.2.2013 7.2 Treatment of vaginal and vulval conditions Preparations for vaginal atrophy Estriol 0.1% cream (Ovestin) Estriol 0.01% cream (Gynest) Estriol 500 microgram pessaries (Ortho-Gynest) Estradiol 10 microgram MR vaginal tabs (Vagifem) Composition - Ovestin® intravaginal cream (15g pack with applicator): estriol 0.1% intravaginal cream. Gynest® intravaginal cream (80g pack with applicator): estriol 0.1% intravaginal cream. Ortho-Gynest® pessaries (500micrograms): estriol 500 micrograms Vagifem® vaginal tablets m/r (15-applicator pack): estradiol 10microgram vaginal tablets. Prescribing notes Local oestrogens can improve local vaginal and bladder symptoms caused by oestrogen deficiency; systemic therapy is necessary for vasomotor symptoms. Most women with significant vulvo-vaginal problems will require long-term treatment particularly if sexually active. Vagifem® may be useful in women who do not find creams difficult or messy to use. It is more expensive Ovestin®. Women using long-term vaginal oestrogen treatments do not need cyclical progestogen therapy. Symptoms recur when local vaginal oestrogens are discontinued; there is no fixed duration of use and each woman should be assessed individually. The lowest effective dose should be used for the shortest duration possible. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 3 of 15 Date: 22.2.2013 Anti-infective drugs Clotrimazole 1% cream Clotrimazole 200mg and 500mg pessaries Other infections Clindamycin 2% vaginal cream Prescribing notes Management of sexually transmitted disease (general notes) With any genital symptoms always consider the possibility of sexually transmitted infection (STI). If an STI is found, there is a strong possibility of others also being present so it is expedient to check. If facilities and skills are available, this can be done by the GP. Otherwise, refer to GUM especially for tests of cure and contact tracing. Of the conditions considered here, only thrush and bacterial vaginosis are considered non-STIs although they can occur concurrently with STIs. Thrush Clotrimazole is available over-the-counter. There is no evidence that treating the partner of women suffering from candidiasis is helpful. Patients who are inserting intravaginal cream or pessaries into the vagina, may also apply topical clotrimazole cream to the vulva. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 4 of 15 Date: 22.2.2013 7.3 Contraceptives General notes Most contraceptive failures are due to poor compliance which is strongly influenced by acceptability. It is important therefore to accept that women may prefer one particular method of contraception and even one particular brand to another despite similar or identical composition. Discontinuation rates of all methods of contraception are high and many women change to a less effective method. Good counselling about risks, side effects and benefits should improve continuation. Long acting reversible methods (LARC), particularly implants and intra-uterine methods, have higher continuation rates and are independent of compliance for their effectiveness. NICE concluded that all LARC, but particularly implants and the IUD/IUS, are more cost effective than either the condom or oral contraception even if discontinued after only one year of use. When a contraceptive is used for management of gynaecological conditions, such as menorrhagia or dysmenorrhoea, the risk/benefit ratio changes and it may be prescribed for women who would have relative contra–indications if they were using it solely for contraception. Young people often have difficulties with consistent and correct use of condoms and oral contraceptives. If the progestogen-only pill is chosen the newer pill (Cerazette®) should be the POP of choice as it has a twelve hour window when pills are missed. Some drugs, including enzyme–inducers and antibiotics, may impair the efficacy of oral contraceptives. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 5 of 15 Date: 22.2.2013 Combined oral contraceptives Ethinyloestradiol 20 micrograms plus desogestrel 150 micrograms (Mercilon®) Ethinyloestradiol 20 micrograms plus norethisterone 1mg (Loestrin 20®) Ethinyloestradiol 30 micrograms plus norethisterone 1.5mg (Loestrin 30®) Ethinyloestradiol 20 micrograms plus gestodene 75 micrograms (Femodette®, Millinette 20/75®) Ethinyloestradiol 30 micrograms plus desogestrel 150 micrograms (Marvelon®, Gedarel 30/150®) Ethinyloestradiol 30 micrograms plus gestodene 75 micrograms (Femodene®, Millinette 30/75®) Ethinyloestradiol 30 micrograms plus gestodene 75 micrograms and placebo (Femodene ED®) Ethinyloestradiol 30 micrograms plus levonorgestrel 150 micrograms (Microgynon 30®, Rigevidon®, Ovranette®, Levest®) Ethinyloestradiol 30 micrograms plus levonorgestrel 150 micrograms and placebo (Microgynon 30 ED®) Ethinyloestradiol 35 micrograms plus norgestimate 250 micrograms (Cilest®, Ovysmen®) Ethinyloestradiol with norethisterone, triphasic (Trinovum®) Ethinyloestradiol with levonorgestrel and placebo, triphasic (Logynon ED®) Drospirenone 3mg with ethinylestradiol 30micrograms (Yasmin®) Prescribing notes The following products are considered interchangeable: o Rigevidon®, Ovranette® and Microgynon 30® o Femodene® and Millnette 30/75® o Marvelon® and Gederal 30/150® Different doses of oestrogen may be associated with different side–effect profiles in individual women. For most, a pill containing 30micrograms oestrogen is recommended. The risk of breast cancer appears to be unrelated to the dose of oestrogen. There is no good evidence for any difference in breast cancer, cardiovascular risk or cycle control with different progestogens. The risk of cardiovascular disease (including venous thromboembolism) is higher with pills containing 50 micrograms oestrogen but there is no evidence for a difference in cardiovascular risk between 20 and 30 micrograms. The MHRA has agreed that while evidence suggests that combined oral contraceptives (COCs) have a higher risk of venous thromboembolism, the absolute risk of venous thromboembolism is small. The relative risk of venous thromboembolism in healthy non-pregnant women taking COCs of second generation progestogens is about 3 times that of non-users of COCs or 5 times for COCs of third generation progestogens. However the absolute risk is considerably smaller than that associated with pregnancy. Provided that this is made clear to the user, there is no restriction on prescription of these pills. Women with acne often benefit from the oestrogen component of combined hormonal contraception. If acne is a particular problem, choose a pill containing a less androgenic progestogen (e.g. desogestrel, Marvelon®) or consider co-cyprindiol 2000/35. Co–cyprindiol 2000/35 (composed of cyproterone acetate 2mg, ethinylestradiol 35micrograms) is a treatment for severe acne that has not responded to oral antibiotics or for moderately severe hirsutism and only in those patients may it also be used as an oral contraceptive (see section Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 6 of 15 Date: 22.2.2013 13.6(a)). Most acne improves with any COC; co-cyprindiol is more expensive and recent evidence suggests an increased risk of venous thromboembolism. Some women with acne or hirsutism requiring contraception may benefit. This is a good example of the need to consider a risk–benefit ratio in women with relative contra−indications. In accordance with MHRA guidance, co–cyprindiol 2000/35 should be withdrawn 3–4 cycles after the treated condition has completely resolved. For acne, substitution with another COC is likely to maintain the improvement but hirsutism is likely to recur. A COC containing a less androgenic progestogen e.g. Gedarel® 30/150, could be substituted but co-cyprindiol 2000/35 may need to be continued. In women with severe hyperandogenism, symptoms usually recur when treatment with cocyprindiol is stopped. In these women treatment may be continued until the symptoms are judged unlikely to recur. The decision of when to stop, should be judged on a case by case basis. Cycle control is no better with triphasic or biphasic COCs and they are more complicated to use. Mercilon® and Gedarel 20/150® (ethinylestradiol 20 micrograms, desogestrel 150 micrograms) contain a lower dose of oestrogen and may be associated with a better side– effect profile in women complaining of oestrogenic symptoms such as breast enlargement/mastalgia. Women aged over 40 years can be advised that no contraceptive method is contraindicated by age alone and that that combined hormonal contraception can be used unless there are co-existing diseases or risk factors. Transermal Combined Hormonal Contraceptives Evra® patch Prescribing notes Evra® patches should be restricted for use in women who are unlikely to comply well with combined oral contraceptives. Side-effects, risks and benefits of Evra® patches are likely to be the same as those for the combined oral contraceptive pill. Evidence suggests no benefit of the transdermal route for COC in terms of reducing the risk of VTE. Progesterone only contraceptives Norethisterone 350 micrograms (Micronor) Desogestrol 75 micrograms (Cerazette) Etynodiol diacetate 500 micrograms (Femulen) Prescribing notes Progestogen-only pills (POPs) are associated with irregular bleeding in up to 40% of users. Bleeding patterns do not tend to improve with time and are not likely to be any different with a different progestogen. There is no evidence for any clinical advantage of any one brand of POP; Micronor® is currently less expensive than alternatives. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 7 of 15 Date: 22.2.2013 Norgeston® contains levonorgestrel, a slightly less androgenic progestogen; it may be the preferred brand for women with oily skin. Cerazette® is more expensive but has been shown to inhibit ovulation to a substantially greater extent than other POPs. It should be reserved for women who cannot tolerate oestrogen containing contraceptives or in whom those preparations are contraindicated. It may also be recommended for women with a history of ectopic pregnancy who take a POP. Cerazette® is also recommended for less compliant women as they are still protected up to 12 hours after missing a pill, whereas only 3 hours with other POPs. It is no longer recommended that women who weigh over 70kg are prescribed two progestogen-only pills (POPs) a day. Parenteral Progesterone only contraceptives Medroxyprogesterone acetate 150mg/ml injection (Depo-provera) Etonogestrel 68mg implant (Nexplanon) Dose - Depo-Provera® injection (medroxyprogesterone acetate 150mg/mL aqueous suspension): by deep intramuscular injection, 150mg within first 5 days of cycle or within first 5 days after parturition (delay until 6 weeks after parturition if breast-feeding); for long-term contraception, repeated every 12 weeks (if interval greater than 12 weeks and 5 days, exclude pregnancy before next injection and advise patient to use additional contraceptive measures (e.g. barrier) for 14 days after the injection). - Nexplanon® implant (etonogestrel 68mg in one flexible rod): by subdermal implantation, Consult product literature for insertion instructions. Prescribing notes Nexplanon® insertion and removal requires specialist training. Nexplanon® is a low dose long–acting progestogen which suppresses ovulation in all women. Contraceptive effect lasts for 3 years and there have been no pregnancies reported. No more than 20% of women will experience amenorrhoea; the rest will have unpredictable and sometimes prolonged bleeding. This point should be covered carefully during counselling. Nexplanon® is more cost effective than either the combined pill or condoms even if used for only one year. Depo-Provera® can cause menstrual dysfunction and weight gain. By the end of the first year of use, 80% of women will have become amenorrhoeic or have scanty infrequent periods. When Depo-Provera® is stopped ovarian activity can take up to a year to recover. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 8 of 15 Date: 22.2.2013 Depo-Provera® is associated with hypoestrogenism and amenorrhoea; recent data have suggested that this is unlikely to have long-term detrimental effects on bone mineral density. The effectiveness of Depo-Provera® is unaffected by enzyme-inducing drugs and the interinjection interval need not be altered. The CSM advises that Depo–Provera® can be used by adolescents who have yet to achieve their peak bone mass if other methods are unacceptable or unsuitable. Young women often find compliance with condoms or oral contraceptives difficult. Emergency contraception Levonorgestrel 1500 microgram tablets (Levonelle One-Step) Ulipristal acetate tablets 30mg (EllaOne®) - Restricted Dose - Levonelle® One-Step tablets containing levonorgestrel 1500 micrograms: 2 tablets to be taken together, as soon as possible, preferably within 12 hours, and no later than 72 hours after unprotected intercourse. Ulipristal acetate tablets 30mg: 1 tablet to be taken as soon as possible following UPSI, but no later than 120 hours Prescribing notes There is no evidence that hormonal EC is teratogenic. It does not work if a woman is already pregnant. Pregnancy can usually be excluded on the basis of the menstrual history; pelvic examination and/or pregnancy testing is only indicated if pregnancy is suspected on clinical grounds. Levonelle®-1500 is available over-the-counter as Levonelle® One-Step. Women who require emergency contraception while using liver-enzyme-inducing drugs should be advised that an intrauterine device is the preferred option. Those that prefer to take a hormonal emergency contraceptive may be advised to double the dose of levonorgsetrel i.e 2 tablets of Levonelle®–1500. Ulipristal acetate, is metabolised by cytochrome P450 and its efficacy may be reduced by enzyme-inducing drugs. Increasing the dose of ulipristal is not currently recommended as there is no evidence that this is effective. If vomiting occurs within 2 hours of taking Levonelle®–1500 or 3 hours of taking ulipristal, a replacement dose can be given. If an antiemetic is required domperidone is preferred. A copper IUD is an alternative form of emergency contraception. It can be inserted up to 5 days after UPSI. An IUD (or advice on how to obtain one) should be offered to all women attending for EC even if presenting within 72 hours of UPSI. If the timing of the ovulation can be estimated, insertion of an IUD can be beyond 5 days of UPSI as long as it is not beyond 5 days of ovulation. Contraceptive devices Femidom, Multiload 375, and Nova-T Levonorgestrel 20 micrograms/24 hours intra-uterine device (Mirena) Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 9 of 15 Date: 22.2.2013 Flat spring diaphragm, practice diaphragm Dose - Mirena® intra-uterine device releasing levonorgestrel 20micrograms/24hours: insert into uterine cavity within 7 days of onset of menstruation (anytime if replacement); effective for 5 years. Prescribing notes Mirena® is a highly effective method of contraception. Many women experience quite frequent and prolonged spotting for the first 3-6 months; thereafter amenorrhoea is common. Patients should be counselled accordingly. Systemic absorption may cause sideeffects e.g. acne or greasy skin. IUD insertions should be performed by someone who has been properly trained, regularly updated and performs regular insertions. Copper IUDs provide long-acting highly effective contraception for at least 5 years and do not rely on compliance for their efficacy. Devices which contain less than 300mm of copper should no longer be used as they are less effective. Condoms are available free of charge from Family Planning Services, and certain GPs. Condoms are the only method which protect against sexually transmitted diseases including HIV; condom users should be informed about emergency contraception. Spermicidal contraceptives Gygel® Composition - Gygel® gel: nonoxinol '9' 2% in a water-miscible base. Prescribing notes Spermicides are not recommended for use as the sole method of contraception but have been traditionally advised for use with the diaphragm and/or for lubrication for male condoms. All currently available spermicides contain nonoxinol '9' (N9) as the active compound. While N9 has been shown to be toxic to HIV in vitro, concerns have been raised regarding its detrimental effect on vaginal integrity and thereby on a possible increase in the risk of HIV/AIDS transmission. Research is ongoing. In the meantime there is no reason to alter the advice that contraceptive diaphragms should be used together with a spermicidal preparation. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 10 of 15 Date: 22.2.2013 7.4 Drugs for genito-urinary disorders Drugs for urinary retention Alfuzosin 10mg m/r tablets Alfuzosin 2.5mg tablets Doxazosin 1mg, 2mg and 4mg tablets Prazosin 1mg tablets Terazosin 2mg and 5mg tablets Tamsulosin 400 microgram tablets Dose - Alfuzosin tablets 2.5mg: elderly, initially 2.5mg twice daily. Max 10mg daily. - Alfuzosin tablets m/r 10mg: 10mg once daily. - Tamsulosin tablets m/r 400micrograms: 400micrograms daily. - Doxazosin tablets 1mg, 2mg, 4mg: initially 1mg daily; dose may be doubled at intervals of 1-2 weeks according to response, up to max 8mg daily; usual maintenance 2-4mg daily. - Prazosin tablets 1mg: 500micrograms twice daily, increased to max 2mg twice if necessary. - Terazosin tablets2mg, 5mg: initially 1mg at bedtime, if necessary dose may be doubled at intervals of 1-2weeks up to a max 10mg once daily. Prescribing notes Tamsulosin should be prescribed generically as tamulosin MR. Watchful waiting may be preferable to treatment in men with mild to moderate symptoms. Alpha-blockers are the treatment of choice for benign prostatic obstruction, and are likely to provide symptom relief in men with prostates of any size. The effect should be noticed within several days, with full response after 4-6 weeks, and the benefit may be maintained for up to 3 years in those who continue to take the drug. There is a lack of published data on effect beyond 3 years. All alpha-blockers are equally effective but there are differences in tolerability. Alfuzosin and tamsulosin are the same in terms of effectiveness and cost. Doxazosin is also a once daily preparation which may be prescribed if side-effects are encountered. Alpha-blockers reduce blood pressure, and first doses may cause drowsiness and dizziness. Patients also receiving antihypertensives may need lower doses and supervision. Parasympathomimetics Distigmine 5mg tablets Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 11 of 15 Date: 22.2.2013 Dose - Distigmine tablets 5mg: 5mg daily Prescribing notes Bethanechol is considered less suitable for prescribing and use been superseded by catheterisation. Distigimine may be useful in patients with an upper motor neurone neurogenic bladder. Drugs for urinary frequency, enuresis and incontinence Duloxetine (Yentreve®) 20mg & 40mg capsules (Restricted) Oxybutinin 2.5mg, 3mg and 5mg tablets Oxybutinin 2.5mg/5ml elixir Oxybutinin MR 5mg and 10mg tablets Propantheline 15mg tablets Solifenacin 5mg and 10mg tablets Tolterodine 1mg tablets Tolterodine 4mg MR capsules Fesoterodine fumerate 4mg & 8mg MR tablets Mirabegron 25mg and 50mg tablets Dose - Oxybutynin hydrochloride tablets 2.5mg, 3mg, 5mg: initially 2.5-5mg 2-3 times daily increased if necessary to max 5mg 4 times daily. - Oxybutynin hydrochloride m/r tablets 5mg, 10mg: over 18 years, initially 5mg daily, adjusted according to response in 5mg steps at weekly intervals; max 30mg daily taken as a single dose. - Duloxetine (Yentreve®) capsules 20mg, 40mg: 40mg twice daily, assessed after 2-4 weeks and reduced to 20mg twice daily if side effects troublesome. - Tolterodine tartrate tablets 1mg, 2mg: 2mg twice daily; reduce to 1mg twice daily if necessary to minimise side-effects. - Tolterodine tartrate m/r capsules 4mg: 4mg once daily. - Solifenacin tablets 5mg,10mg: 5mg daily, if necessary increased to 10mg once daily. - Fesoterodine fumerate m/r tablets 4mg, 8mg: over 18 years, 4mg once daily, increased if necessary to max 8mg once daily. - Mirabegron tablets 25mg, 50mg: over 18 years, see BNF. Prescribing notes The use of oxybutynin may be limited by side-effects. These may be reduced by commencing with a low dose and increasing gradually; modified-release oxybutynin is better tolerated. As it is as effective, as well tolerated and substantially less expensive, oxybutynin m/r may be used in preference to standard release tolterodine (1mg, 2mg). Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 12 of 15 Date: 22.2.2013 Solifenacin is substantially more expensive but may be an option for those who do not tolerate oxybutynin. Antimuscarinic therapy should be reviewed after 6 months and if symptoms are wellcontrolled therapy may be reduced or discontinued as symptoms may not recur. There is no evidence that oestrogens cause subjective or objective improvement of symptoms of urge and urge incontinence. Duloxetine (Yenetreve®) should be prescribed by brand name and is restricted to use in moderate to severe stress urinary incontinence in women. Patients should be reviewed after 12 weeks of therapy to assess progress and the treatment discontinued if no improvement is demonstrated. Drugs used in urological pain Potassium citrate mixture Dose - Potassium citrate mixture BP (potassium citrate oral solution containing potassium citrate 30%, citric acid monohydrate 5% in a suitable vehicle with a lemon flavour): 10mL 3 times daily well diluted with water. Prescribing notes Many patients obtain good relief from the symptoms of cystitis with over-the-counter medicines. Sodium bicarbonate is used as a urinary alkalinising agent in some metabolic and renal disorders. Bladder instillations and urological surgery Sodium chloride bladder 0.9% irrigation (Urotrainer M) Uro-Tainer Suby G Chlorhexidine 0.02% bladder irrigation (Urotrainer C) Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 13 of 15 Date: 22.2.2013 Drugs for impotence Alprostadil 10 microgram and 20 microgram injection (Caveject Dual Chamber) Alprostadil 250, 500 microgram and 1mg urethral applications (MUSE) Sildenafil 25mg, 50mg and 100mg tablets Limited prescribers - please contact Pharmacy for advice Tadalafil 10mg and 20mg tablets Limited prescribers - please contact Pharmacy for advice Vardenafil 5mg, 10mg and 20mg tablets Limited prescribers - please contact Pharmacy for advice Dose - Sildenafil (Viagra®) tablets 25mg, 50mg, 100mg: start with 50mg tablets and increase to 100mg if necessary. Try at least 8 times before abandoning if ineffective. Max dose 100mg in 24 hours. - Tadalafil tablets 10mg, 20mg: initially 10mg approx. 30 minutes to 12 hours before sexual activity, subsequent doses adjusted according to response to 20mg as a single dose; max. 1 dose in 24 hours. - Vardenafil tablets 5mg, 10mg, 20mg: initially 5-10mg approx. 30-60 minutes before sexual activity, subsequent doses adjusted according to response to 20mg as a single dose; max. 1 dose in 24 hours. - Alprostadil (Caverject® Dual Chamber) injection 10microgram, 20microgram: by direct intracavernosal injection, initially 2.5micrograms, titrated to response (usually 10-20micrograms); max 60micrograms. The required dose should be injected no more than once daily and no more than 3 times weekly. - Alprostadil (Muse® Dual Chamber) uretheral application 250microgram, 500microgram, 1mg: by direct urethral application, initially 250micrograms, titrated to response (usually 0.125-1mg). Max 2 doses in 24 hours and 7 doses in 7 days. Prescribing notes NHS Regulations (1999) limit the use of NHS prescriptions by GPs for treatment of erectile dysfunction. NHS prescriptions (endorsed "SLS") can be issued for sildenafil, alprostadil, tadalafil and certain vacuum tumescence devices to men suffering from erectile dysfunction who have these medical conditions: diabetes, multiple sclerosis, Parkinson's disease, poliomyelitis, prostate cancer, prostatectomy (including TURP), radical pelvic surgery, renal failure treated by dialysis or transplant, severe pelvic injury, single gene neurological disease, spinal cord injury, and spina bifida. Treatment should be available from specialist services in cases where erectile dysfunction is causing severe distress. Examination of the patient is important to check for anatomical abnormalities and Peyronie's disease which may need referral to Urology. Diabetes needs to be excluded and cardiovascular risk factors addressed because they are commonly present. Tadalafil may be a suitable alternative for patients who develop visual disturbances with sildenafil or for whom a longer duration of action is required. Sildenafil and tadalafil are contra-indicated in men receiving nitrates in any form, and nicorandil. Consider discontinuing nitrates if no longer needed. Cardiovascular disease and multiple antihypertensive drug regimens are not contraindications to sildenafil or tadalafil therapy provided the man is capable of ordinary daily tasks (and therefore sexual activity) without cardiac symptoms. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 14 of 15 Date: 22.2.2013 Intracavernosal self-injection with alprostadil is a suitable second choice to sildenafil if treatment with sildenafil fails or is contra-indicated. The recommended alprostadil preparation is Caverject® Dual Chamber, which is supplied with an injector device. All patients commencing intracavernosal injection therapy require supervised instruction on its use and advice on action required should a prolonged erection (>6 hours) occur. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber 1 = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 15 of 15 Date: 22.2.2013