* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Biology 30 Student Notes Nervous Reproduction_1
Survey
Document related concepts
Transcript
Mrs. Paulgaard
Biology 30
Notes & Diagrams
Nervous, Endocrine &
Reproductive Systems
Systems Regulating Change in Human Organisms (Homeostasis)
Homeostasis: a process by which a constant internal environment is maintained despite
changes in the external environment (ex. Regulation of blood sugar)
Nervous System (quick & short term response)
Endocrine System (slow & long term response)
Nervous System:
Involves reception, transmission, interpretation and response.
Two main sub-systems:
o Central Nervous System (CNS), (brain and the spinal cord)
o Peripheral Nervous System (PNS) (autonomic [involuntary] and somatic
[voluntary] systems)
CNS
PNS
Receptor
Sensory
Effector
Motor
Neurons: nerve cells (many neurons together = nerve)
specialized to conduct an electrochemical impulse
three types:
o Sensory Neurons: carry an impulse away from the receptors to the spinal cord
or directly to the brain. (Receptors)
o Motor Neurons: carry an impulse away from the brain to the muscles or glands
(Effectors).
o Association or Interneurons: carry impulses across the spinal cord and to the
brain.
link between sensory and motor neurons
found only in the CNS
shorter and slower than sensory or motor neurons
unmyelinated.
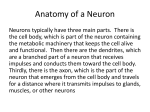
basic components:
o
o
o
dendrite region
receives stimuli either from the environment or from other neurons.
shorter branched extensions of the cell body that receive incoming
signals
cell body
contains the nucleus and most of the usual cell organelles
clusters of cell bodies in the C.N.S. are called "nuclei"; make up the grey
matter
clusters outside the C.N.S. make "ganglia"
axon
"trunk" of the neuron along which impulses travel to reach the next nerve
or effector
many be very long, up to 1 meter such as those that run from the base of
the spine down the leg
terminates in a synaptic junction
o
o
myelinated or non-myelinated fibre
myelin is a fatty protein sheath (white) covering axons of nerves
composed of schwann cells
allows these portions of the axon to be quickly passed over during
nerve transmission
Gaps in between are called Nodes of Ranvier.
o nerve transmission occurs at the node only and skips over
the insulated portion of the axon. nerve impulse move
faster as the current jumps from node to node.
neurilemma: found on myelinated neurons
membrane around the axon which heals damaged neurons and works
with the schwann cell to regenerate damaged nerves.
Myelinated neurons
White matter: has fat/myelin/schwann cells
In PNS and CNS
Can repair damage: has a neurilemma
Impulse travels faster
Unmyelinated neurons
Gray matter: no fat/myelin/schwann cells
Only in CNS
Cannot repair damage: does not have a
neurilemma
Impulse travels slower
Nerve Impulse: Fibre Transmission
1. Neuron at Rest: resting potential
The nerve impulse cannot occur along a neuron unless it is polarized as shown below.
Gates on the membrane that control the movement of Na+ and K+
The ion pump transports 3 Na+ out [+] for every 2 K+ that flows back in [-].
The net result of the ionic gradients is a charge difference across the membrane, the inside
being negative, the outside being positive.
Now polarized (ready to fire) -70mV or -0.07V (potential difference)
2. Impulse: Action Potential
Begins with a stimulus which causes depolarization.
Neuron at Stimulus:
Certain chemicals (neurotransmitters) produced by the body, or external stimuli, stimulate
the membrane of the dendrite which causes the membrane becomes permeable to Na+
(gates open)
Na+ floods in by diffusion and reduces the potential difference to 0.0V
More Na+ diffuses in causing the inside to switch from negative to positive called
depolarization. (+30mV)
Resting membrane adjacent to the area of reversed polarity undergoes a permeability
change and becomes permeable to Na+
An area of reversed polarity sweeps along the neuron. Action Potential Propagation
This charge reversal causes the membrane to become less permeable to Na (Na gates
close)
3. Refractory Period: Recovery
Neuron is returned to its normal resting potential or is repolarized.
The membrane becomes more permeable to K (K gates open)
K will rush out because there is a high concentration of K inside the cell and a low
concentration outside the cell.
The normal negative charge inside the cell is restored, but Na and K are on the reverse
sides.
The Na/K pump moves 3 Na out for every 2 K moved in restoring the membrane back to
resting state.
Polarized
Depolarized
Repolarized
Na gate
K gate
Na/K pump
Ion diffusion
Closed
Open
Closed
Open
Closed
Open
Na out/K in
Na out/K in
Na out/K in
K out
Na in
K out
Membrane
charge
+out/- in
+in/-out
+out/-in
Graph of an Action Potential
Threshold
The minimum level of potential difference (mV) needed to get an impulse to form.
o Must be at or above threshold level in strength to cause depolarization.
o Ex: 50mV
Caused by stimuli like electrical shock, heat, chemicals or mechanical deformation.
(chemical, electrical, light, sound, other)
Different neurons in the same person and the same neuron in different people can have
different threshold values. (Explains the differences in tolerance or sensitivity different
people have to the same stimulus (pain, smell)).
Impulse Characteristics
Once stimulated the action potential will spread over the entire neuron and cannot be
stopped (All or None Response)
Speed of nerve impulses varies depending thickness of the nerve and it is myelinated or
unmyelinated impulses travel at 1 to 120 m/s
inside a neuron impulses always move in one direction: dendrite cell body axon
The stronger the stimulus is the greater the frequency of impulses produced by that neuron
Synapse:
Movement of the impulse from the axon of one neuron to the dendrite of another neuron or
membrane of a gland or muscle.
A synaptic cleft is a junction between the axon of one neuron (presynaptic neuron) and the
dendrite of another neuron (postsynaptic neuron).
On the axon side there is a synaptic knob, a swelling of the end of an axon, which contains
synaptic vesicles.
o Tiny vacuoles which contain acetylcholine or ACH (neurotransmitter) which are
released into the gap or junction.
o They excite or inhibit the neighboring neurons.
o The postsynaptic membrane releases cholinesterase (acetylcholinesterase or ACHase) that breaks down acetylcholine clearing the synapse and preventing further
impulses.
Types:
Excitatory synapses cause depolarization of the next neuron
o Continuing the impulse (hypopolarization; lowering the threshold level to cause
action potential -60mV)
o Stimulant
Inhibitory synapses prevent depolarization of the next neuron.
o Makes the postsynaptic membrane to become more permeable to K resulting in
hyperpolarization (need more than the normal threshold level to cause action
potential)
o Inhibitor or Depressant
Neurotransmitters:
Most common is acetylcholine - broken down by acetylcholinesterase found at
neuromuscular junctions, in the brain, and at the junctions of internal organs
Noradrenalin or Norepinephrine of the sympathetic nervous system (PNS)
Other transmitter substances include adrenalin (epinephrine), serotonin, endorphin (pain
killer), histamine, dopamine, and many psychoactive drugs—LSD, Psilocybin
Substances that Affect Synaptic Function:
Caffeine and other stimulants increase ease of passage of impulse across synapses.
Nicotine mimics acetylcholine.
aspirin, opium, morphine inhibit passage
decreased H+ ions (alkalosis) increases excitability
increase in H+ ions (acidosis) decreases excitability
low O2 levels (hypoxemia) causes cessation of synaptic activity
Summation:
Accumulation of transmitter chemicals from two or more neurons.
Whether or not a postsynaptic neuron will fire depends on the effects of more than one
presynaptic neuron
Nerve Pathways:
1. Learned Response: conditioned response
Information from the environment goes to the brain, is processed, and the brain
decides what action to take.
We have conscious control over this.
2. The Reflex Arc: spinal cord responsible for reflexes
Reflexes are quick involuntary, not learned, responses or actions that the body takes
to protect itself from danger.
Association Neuron
CNS
Sensor Neuron
PNS
Motor Neuron
PNS
Receptor
Effector ~
Muscle
Sensory organ detecting a dangerous stimulus.
Sensory Receptor
Sensitive to Environmental Factors
Baroreceptor
Sensitive to pressure(found in the skin and blood vessels)
Osmoreceptor
Sensistive to fluid (water) levels(found in blood vessels)
Photoreceptor
Sensitive to light (eyes)
Mechanoreceptor
Sensitive to vibrations (ear)
Thermoreceptors
Sensitive to heat
Proprioreceptors
Sensitive to motion ( found in tendons, muscles, and
ligaments)
An impulse is passed to a sensory neuron, takes the message to the spinal cord
where it is picked up by an association neuron (interneuron).
The interneuron passes the message immediately to the appropriate motor neurons,
and it takes the message to the effectors that can do something to bring about a
change to whatever is causing the stimulus.
Central Nervous System
Includes both the brain and spinal cord
Brain: 2 kg
billions of neurons and “glial” cells that support and nourish the neurons.
connected to the rest of the body by the spinal cord and 12 cranial (found inside the skull or
cranium) nerves.
two distinctive layers: (gray matter and white matter)
o External Grey Matter: cerebral cortex:
thin outer layer composed of nonmyelinated interneurons (gray matter).
most of the brain activities
many folds and wrinkles that increase the surface area so there is more room
for neurons
o
Internal White Matter: below the cerebral cortex
composed of hollow fluid filled spaces and bundles of myelinated neurons
(white matter)
Composed of several parts:
Cerebrum: largest part of the brain.
major center of nerve control in our body and is highly developed
outer surface is the cerebral cortex.
All thoughts, memories, perceptions originate or are processed in the
cerebrum.
Divided into two halves, called hemispheres, connected by a bundle of nerve
fibers called the corpus callosum.
right hemisphere is responsible for more artistic, 3 dimensional,
creative tasks, left body functions
left hemisphere is for more analytic, problem solving, mathematics,
logical tasks, right body functions.
4 lobes
Lobe
Frontal
Location
At the front
Temporal
Occipital
Parietal
The sides
Low at the back
The top and back
Task
Voluntary muscle
movements, basic
intelligence, personality
Hearing
Vision
Skin sensory information
and body position
Cerebellum: responsible for balance, co-ordination of movement, and muscle tone
Medulla oblongata: receives and integrates signals from the spinal cord.
o It sends signals to the cerebellum and thalamus.
o Controls breathing and heart rate, as well as several autonomic functions such as
dilation and constriction of blood vessels, coughing, swallowing, and vomiting.
Pons: it relays impulses between the medulla and other parts of the brain (cerebrum and
cerebellum, right and left hemispheres)
Thalamus: it relays sensory impulses to the cerebral cortex and motor impulses from the
cerebral cortex to the spinal cord
Hypothalamus: receives sensory impulses from the internal organs by way of the thalamus,
and allows us to feel hunger, thirst, aggression, rage, and pleasure.
o It also controls the actions of the autonomic nervous systems.
o It connects to and controls the pituitary gland which them controls the endocrine
system
Pituitary gland- produces hormones that regulate other endocrine glands.
o Endocrine glands produce hormones that enter the blood.
o Exocrine glands produce other body fluids that leave the gland through tubes/ducts.
Midbrain- relays sensory impulses between the spinal cord and the thalamus and relays
motor impulses between the cerebral cortex, pons, and spinal cord.
Brain protection:
There are four structures that protect the brain and spinal cord:
1. Bone: The brain is surrounded by the skull and the spinal cord by all the vertebrae
2. Meninges: This is a 3-layer membrane that wraps around the brain and spinal cord.
From outer to inner the layer names are dura mater, arachnoid layer, and pia mater
3. Blood brain barrier: Blood vessels in the brain act as a filtration system that selectively
lets in molecules that the brain uses, such as glucose and amino acids.
4. Cerebrospinal fluid: Tissues inside the brain produces a fluid that nourish cells and
absorb shock from quick movements of the head.
Spinal cord:
Grey matter on inside and white matter on outside (<1cm)
Each bone (32) of the vertebrae in the spine has nerves passing from the cord out to the body.
The dorsal root (back half of the spinal cord) is composed of sensory neurons.
The ventral root (front half of the spinal cord) is composed of motor neurons.
Gray matter (interneurons) carry impulses across the spinal cord (back to front) connecting
sensory and motor neurons. {Reflex Arc}
The outer white matter of the spinal cord moves nerve impulses up and down the spinal cord, to
and from the brain.
Drugs
Stimulants – excitatory - caffeine, nicotine, amphetamines stimulate the sympathetic
nervous system and presumably the control center or hypothalamus
Depressants – inhibitory - alcohol depresses motor and sensory regions of the cortex. It
also depresses the cerebellum (muscular coordination), the midbrain (balance) and the
reticular formation with heavy intake of alcohol.
Opiates depress the thalamus, thus are effective painkillers
Technology:
MRI: magnetic resonance imaging
CT Scan
EEG: electroencephalograph translates electrical activity of the brain.
Peripheral Nervous System:
somatic nervous system (voluntary)
o nerves that extend to and from the spinal cord
o the motor and sensory neurons
autonomic nervous system (involuntary) which are only motor neurons.
o runs separate from the spinal cord connecting the brain to the involuntary organs
o controls functions independent of our conscious control, ex: breathing, digestion,
heartbeat, hormones
o controlled by the hypothalamus and medulla
Autonomic Nervous System
ANS functions through two motor nerves:
Parasympathetic Nervous System: relaxes or returns body back to normal
Sympathetic Nervous System: gets ready for action or stress Flight, Freeze or Fight
Response
parasympathetic neurons:
-slow heart rate
-decreased breathing rate
-constricts bronchioles
-increase peristalsis
-pupil constriction
-vasoconstriction of the
skeletal muscles
-increases stomach activity
-constricts bronchioles
-contracts bladder
-converts glucose to glycogen
-returns body to normal after
an emergency
(cortisol)
sympathetic neurons:
-increase heart rate
-increase breathing rate
-dilates bronchioles
-decrease peristalsis
-pupil dilation
-vasodilation of skeletal
muscles
-decreases stomach activity
-dilated bronchioles
-inhibits bladder
-release glucose
-prepares body for an
emergency
(adrenalin/epinephrine)
Senses: Ear, Nose, Tongue, Eye
Receptor Characteristics:
all are connected to sensory neurons
stimulation of special cells in the receptor organ results in the production of an action
potential
the stronger the stimulus the greater the frequency of action potentials produced by the cell
sensory adaptation or constant exposure to the stimulus leads to increased insensitivity to
that stimulus, (may be decreased ACH production at the synapse).
o The receptor stops sending impulses, or decreases the frequency of impulses
produced. (ex; hot water, cold water, luke water)
Eye:
Increase %
Rods
Decrease %
Cones
From Fovea
Centralis
Eye parts and functions
Eyelids and eyelashes: Protection of the eye
Extrinsic muscles: Movement of the eye, left to right, up and down
Sclera: White outer layer, protective, maintains shape of the eye
Choroid layer: Contains a black pigment that absorbs light preventing light from reflecting
inside the eye
Blind spot: Point at the back of the inside of the eye, on the retina, where are the axons
from the neurons in the retina leave the eye forming the optic nerve. There is no room for
rod or cones cells, consequently this tiny spot is blind.
Cornea: Transparent membrane on the front of the eye, focuses light on the lens and
protects the eye
Iris: Circular muscle with a hole in the middle (pupil). It contracts to constrict the pupil when
focusing on close up objects or light is bright, or relaxes to dilate the pupil when focusing on
far away objects or when light is dim
Pupil: Hole in the middle of the eye that lets light pass through onto the lens
Aqueous humor: Fluid in between the cornea and iris that maintains the shape of and
nourishes the cornea
Vitreous humor: Fluid found behind the lens, helps maintain the shape of the eye
Ciliary muscles: Adjust the curvature (shape) of the lens focusing light on the retina
Lens: Focuses light on the fovea and retina
Retina: contains photoreceptor cells (rods and cones)
Rods:
sensitive to light at low intensity (needs less light for action potential)
produce black and white vision
more than one rod cell per neural circuit (neuron)
vision is not acute or sharp
Cones: Greatest density in the fovea
senitive to light at high intensity (needs more light for action potential)
produce colour vision (green, red, blue)
one cone per neural circuit
vision is acute and sharp
Fovea centralis: Tiny spot on the retina, composed only of cones, upon which light passing
through the lens is focused.
Chemistry of Vision: RODS
Rhodopsin: require vitamin A for production
o Visual pigment found in rod cells
o Helps in the recovery rate of light intensity changes
o Uses ATP
Rhodopsin + light Opsin + Retinene {depolarizes neuron}
Vitamin A + ATP + Opsin + Retinene Rhodopsin {restore resting potential}
Other pigments in Cones
Accommodation: The ability of the lens to change its shape to adjust focusing on near and far
objects
Close up vision: lens short and fat (Ligaments release tension)
Long distance vision: lens thin and long (Ligaments increase tension)
Visual Acquity: The ability of the lens to focus detail
Sensory Adaptation of the eye: Switching from rods to cones or vice versa; increasing light
intensity increases activity of cones and decreases activity of rods, and vice versa with
decreasing light intensity
Eye disorders
Eye disorder
Near sighted
Problem
Eye too short (lens cannot
flatten)
Effect
Image focused before
retina
Far sighted
Eye too long (lens cannot
widen)
Image focused after retina
Astigmatism
Irregular curvature of lens
Blurred vision
Glaucoma
Build up of fluid in eye
Cataract
Lens of cornea clouds
Cuts off blood to
retina=blindness
Block light to
retina=blindness
Hearing and the Ear:
contains receptors sensitive to vibrations (hearing) and for static and dynamic balance
Range of hearing is from 20-20,000 cycles per second (hertz)
Outer Ear: Pinna Ear Canal Eardrum
External Pinna: Collect, funnel sound into the auditory canal
Auditory Canal: Funnel sound to the eardrum
Eardrum (Tympanic Membrane): vibrates in response to sound, causing ossicles to vibrate
Middle Ear: Hammer Anvil Stirrup Oval Window Cochlea (Inner Ear) Round
Window // Eustachian Tube
Ossicles: Very small bones, hammer, anvil, stirrup, that amplify vibrations from the eardrum
Oval Window: Small membrane on the cochlea that transmits sound into the cochlea
Round window: Lets remaining motion out of the cochlea
Eustachian Tube: Connects the outer environment to the middle ear by way of the throat
allowing air pressure to be equalized
Inner Ear: Cochlea Organ of corti (hairs) nerve
Cochlea: Contains lymph fluid, organ of corti and the basilar membrane
o Organ of corti: Made of many neurons that contain microscopic hairs
(mechanorecpetors) that when moved (by vibrations) generate nerve impulses.
Long hairs generate impulses interpreted as low sounds
Short hairs are for high frequency sounds.
o Basilar membrane: A membrane that anchors the hair cells in the organ of Corti.
o Auditory nerve: Sensory neurons that carry impulses to the temporal lobe from the
cochlea
Vestibule: contains two soft sacs of fluid, the utricle and saccule.
o
Contain fluid and tiny stones (otholiths) that stimulate sensory hairs to generate
nerve impulses for position of the head (static equilibrium)
Tension
sends an
impulse
Stones
attached to
hairs that
transmits
messages
with respect
to gravity
Semicircular Canals: Fluid filled chambers containing sensitive nerve hairs that are
responsible for detection of a change in motion [speed & direction] (dynamic equilibrium)
o Right-angles to each other (one in each plane)
semicircular canal
Ear Disorders:
Tenitus: temporary or constant ringing in the ear
Nerve Deafness: due to damage to sensory hair cells on organ of corti or auditory nerve or
brain damage in the temporal lobe.
Conduction deafness: due to damage to the eardrum, ossicles, oval window, or basilar
membrane.
Effectors: composed of muscles and glands. Cause a response.
Exocrine glands: produce secretions (enzymes, sweat) which are released into tubular
ducts out of the body or into a body cavity. (ex. Saliva glands, liver, pancreas)
Endocrine glands: are ductless glands and generally produce hormones that are released
into the blood (ex. Pituitary, pancreas, adrenal)
Major Endocrine Glands:
Pituitary Gland: master gland that influences all the other endocrine glands
Thyroid Gland: influences metabolic rate, decreases blood calcium & stores it in bones
Parathyroid Gland: increase blood calcium for muscle contraction & blood clotting
Thymus Gland: aids in immunity reactions (t-cells)
Adrenal Gland: prepares the body for stress
Pancreas: controls blood sugar
Ovaries (female gonads): produces female sex hormones & influences secondary sex
characteristics.
Testes (male gonads): produces male sex hormones & influences secondary sex
characteristics.
Hormones: a chemical released into the blood steam from an endocrine gland and cause a
response in a target organ/tissue.
Protein hormones: made from amino acids.
o combine with specific receptor sites on the cell membrane of the target tissue and
trigger the formation of cyclic AMP from ATP.
o Cyclic AMP acts as a messenger inside the cell, activating enzymes in the cell.
o (ex: insulin, growth hormone, and adrenaline)
Protein Hormone Action
Steroid hormones: made from cholesterol (a lipid/fat compound).
o The steroid hormone molecule passes into the cell, combines with a receptor
molecule, and then activates a gene in the nucleus.
o The gene directs the production of a specific protein.
o (ex: male and female sex hormones and cortisol)
Steroid Hormone Action
Human Hormones:
Gland
produced by
Hormone
Growth hormone
(GH),
Somatotropin
(STH), or Human
Growth Hormone
(HGH)
Target tissue
All body tissues
Function/action
Increase growth and
metabolism
hyposecretion causes
midgets
hypersecretion causes
pituitary giants as a
child or acromegaly as
an adult
Anterior
pituitary
Thyroidstimulating
hormone (TSH)
Adrenocorticotrop
ic hormone
(ACTH)
(ad-reen-oe-cor-ticoe-troe-fik)
Thyroid
Increase thyroxin production
Adrenal cortex
Releases cortisol and
aldosterone
hypersection results in
the adrenal gland
hypercortisolism
(Cushing’s Disease)
Posterior
pituitary
(released from)
Secreted by
Hypothalamus
Follicle
stimulating
hormone (FSH)
Luteinizing
hormone (LH)
Ovaries and
testes
Stimulates growth of egg and
sperm cell (gametes)
Ovaries and
testes
Prolactin (PRL)
Mammary
glands
Skin
Causes ovulation and
progesterone and
testosterone production
Stimulates and maintains
milk production
Produces skin pigments
Sleep patterns
Melanocytestimulating
hormone (MSH)
(mel-an-oe-site)
Antidiuretic
hormone (ADH)
Oxytocin
Thyroxin
Kidney
nephrons
Uterus
muscles,
breasts
Body cells
Thyroid
Calcitonin
(cal-si-tone-in)
Bones
Increases water reabsorption
hyposecretion causes
diabetes insipidus
Contraction of muscles,
secretion of breast milk, “love”
Increases metabolism
hypothyroidism in
childhood causes
mental retardation &
dwarfism (cretinism)
hypothyroidism in
adults causes
myxedema (weight
gain, high blood
pressure, hair loss,
sluggishness and fluid
collection in the
tissues)
hyperthyroidism
causes irritability,
weight loss, high blood
pressure, high pulse
rate and bulging eyes
Stimulates bones to remove
calcium from the blood
Parathyroid
Parathormone
(PTH)
Adrenal
medulla
Adrenaline
(Epinephrine))
Stress hormone
Aldosterone
(aldo-ster-one)
Cortisol
Stress hormone
Adrenal cortex
Pancreas
(Islets of
Langerhans)
Bones
Stimulates bones to increase
calcium in the blood
hyposecretion causes
spasms of muscles
and disrupts nervous
conduction
hypersecretion causes
brittle bone and kidney
disease
All body cells
Accelerate body reactions and
functions
Kidney
nephrons
Liver
Increased salt absorption
Release of amino acids which
are converted into glucose.
Increased glucose production.
hypocortisolism
(Addison’s Disease)
Decreases blood sugar
(glucose)
Makes cell membranes more
permeable to absorb glucose
hyposecretion causes
diabetes mellitus
(hyperglycemia)
hypersecretion causes
low blood sugar
(hypoglycemia)
Increases blood sugar
(glucose)
Makes cell membranes less
permeable to absorb glucose
Insulin
Liver and
muscles
Glucagon
Liver and
muscles
Estrogen
Uterus, breasts
Secondary sex characteristics
and growth of endometrium
hyposecretion causes
failure of female to
mature sexually
Uterus
Maintains endometrium and
inhibits uterine contractions
Ovary
Progesterone
Testes
Testosterone
Testes
(sertoli cells)
Chorion or
Placenta
Inhibin
Human chorionic
gonadotropin
(HCG)
Skin, muscles,
bones, brain
Secondary sex characteristics
(Increases growth of sperm
cells, body hair, muscles and
bones)
hyposecretion causes
failure of male to
mature sexually
Pituitary
Inhibits FSH production
Ovary
Maintains corpus luteum
progesterone production
Homeostasis: negative feedback (How the body will counteract a change.)
Negative Feedback: regulation of metabolic rate:
Metabolism: the sum of all the reactions that occur in the body and the cellular level.
Measured by monitoring body temperature because a high body temperature means higher
metabolic rate. It is controlled by the interaction of three hormones. TRF, TSH, and Thyroxin.
(- feedback)
Hypothalamus
(Thyroid Releasing Hormone)
(TRH)
HEAT
Increased Metabolic Rate
Anterior Pituitary
Inhibition
(Thyroid Stimulating Hormone)
(TSH)
(Thyroxin)
Thyroid
Goiter (lack of iodine) enlarged thyroid
b/c it doesn’t produce enough thyroxin
yet is being stimulated by TSH
o
Body temperature can also be controlled through vasoconstriction and vasodilation,
sweating, shivering, and goosebumps.
Negative Feedback: regulation of blood sugar:
maintaining proper blood sugar concentration by regulating insulin and glucagon production
High Blood Sugar
(- feedback)
INSULIN
Pancreas
Glucose Glycogen
Cell Membranes Permeable
Liver
GLUCAGON
Glycogen Glucose
Cell Membranes Impermeable
Low Blood Sugar
(- feedback)
Comparison of nervous system to endocrine system
Characteristic
Nervous system
Mode of action
Neuron
Method of action
Nerve impulse
Response time
Immediate
Duration of effect
Short
Endocrine system
Blood stream
Hormone
Short-long term
Long
Stress: a physical or psychological stimulus that cause a change in the body, it alters
homeostasis.
Drug: any substance, other than food, that alters normal body functions or is used to treat
disease
General Adaptation Syndrome
Shock: a sudden physical or mental disturbance. (High stress both the nervous system and the
endocrine system respond with a series of automatic responses together)
Issues or Views:
Technological: Use and knowledge of tools, techniques, and skills that are an application of
science.
Ethical: concepts of good and bad, right and wrong, and justice. Individual viewpoint rooted in
morality and religious values.
Societal: culture economics, politics, customs, and human society. Group viewpoint.
Reproduction and Development
Male vs. Female:
Males posses an X and Y chromosome (master switch of sexual development). Sexdetermination is controlled by a gene located on the Y chromosome.
o XY: the gene turns on other genes (at around 38 days)
primitive gonads turn into testes which secrete androgens (testosterone)
external genitalia become masculinized
germ cells into spermatogonia (sperm cells)
Females two X-chromosomes
o XX: in the absence of Y
gonads develop as ovaries
germ cells become oogonia (egg cells).
Gametes: sex cells that contain 23 chromosomes (Sperm or Ova/Ovum/Egg) and are
considered haploid (n)
Sperm:
Head:
Contains the nucleus 23 chromosomes (either an X or Y sex chromosome)
Acrosome contains enzymes that are used to break through the outer layer of the egg
during fertilization
Neck:
Many mitochondria that provide the energy for movement of the tail
Tail:
Flagella
Millions of Sperm:
Two fallopian tubes and one ovum
Vagina is acidic
Fertilize any sphere
100 to 500 acrosomes to break through the ovum’s covering
Immature and mutated sperm
Male Reproductive Anatomy:
Parts:
Penis:
o External sex organ
o Contains vascularized spongy erectile tissue around the urethra that fills with blood
when sexually excited.
o Controlled by the parasympathetic nervous system
o Sympathetic nervous system responsible for the release of sperm (ejaculation ~ orgasm)
[smooth muscles]
Urethra:
o Passageway for urine & semen. 20 cm. long.
Vas deferens:
o Tubes that carry sperm from testicles to urethra.
Scrotum:
o Out-pouching of abdomen, contains testes.
o Regulates their temperature by contraction of cremaster muscle.
o Cold: it contracts. Warm: relaxes. Goal: keeps testes 3° C. below body temperature.
Testes:
o Sperm-producing organ, source of male hormone testosterone.
o composed of seminiferous tubules that produce the male gametes, the sperm cells
o The interstitial cells surround the seminiferous tubules and produce testosterone.
(androgens ~ male sex hormomoes).
Minimal amounts produced in the ovaries, and adrenal cortex. (Females)
It will attach to receptors and develop secondary sex characteristics. Excess
amounts will be converted into estrogen in males
o Epididymis stores sperm and contracts during ejaculation
o Sertoli cells provide nourishment and anchor the developing sperm cells. They also
produce the hormone inhibin (inhibits male FSH and LH)
Spermatogenesis (gametogenesis):
About 300 million immature sperm cells are made every day.
If they are not used they get reabsorbed by the seminiferous tubules
Spermatogonia are the parent cell (46 chromosomes) that divides by meiosis to
produce 4 haploid spermatocytes (23 chromosomes) cells. (sperm ~ outside)
Spematogonia
(Diploid)
Meiosis
Spermatocytes
(Haploid)
2x
46
92
46
23
÷2
÷2
46
23
23
23
Sperm cell production is best a few degrees below body temperature. The rapid division of
cells produces heat. This heat can destroy the cells produced. This is why the testes are
found outside the body suspended in the scrotum.
Glands of the Male Reproductive System:
o Contribute secretions to sperm that make up semen
Prostate:
o Surrounds the urethra and secretes fluid that contains milky fluid (mucus) that aids in
sperm motility as well as sodium bicarbonate that protects sperm cells from the acidic
environment of the vagina.
o Contracts during an ejaculation to move the semen out into the urethra through the vas
deferens
Cowper’s Gland:
o Produces a basic fluid that neutralizes the acid in the male urethra
o Adds mucous rich fluid to the seminal fluid and assists in sperm cell movement.
Seminal Vesicles:
o Fructose solution that provides energy for the movement of the tail of the sperm.
o Fluid also has prostaglandins (hormones) that cause contractions of the muscles of the
uterus to help the sperm cells move.
Semen:
o Spermatozoa
o Fructose
o Prostaglandins (activating agent)
o Bases
Regulation of Male Sex Hormones:
Hypothalamus
GnRH
Anterior Pituitary
FSH
Inhibin
LH
Primary Sex
Characteristics
Secondary Sex
Characteristics
TESTS
Sertoli
Cells
Seminiferous
Tubules
Interstitial
Cells
SPERM
Spermatogenesis
Testosterone
GnRH: (Gonadotropic Releasing Hormone)
FSH (follicle stimulating hormone): (gonadotropic hormone) stimulates the seminiferous tubules
to produce sperm cells
LH (Luteinizing hormone): (gonadotropic hormone) stimulates the interstitial cells to produce
testosterone
Testosterone: stimulates seminiferous tubules to produce sperm cells, secondary sex
characteristics. (Androgens)
o Produced in the testes, with minimal amounts produced in the ovaries, and
adrenal cortex.
o Excess amounts will be converted into estrogen in males.
Inhibin: inhibits FSH
Sex characteristics
Primary
Characteristics required for
successful reproduction
Secondary
Characteristics that
enhance but NOT required
for successful reproduction
Males
Testes, sex organ development
Females
Ovary, sex organ development
Body & facial hair, increased
muscle mass, increased bone
density, aggression, lengthen
larynx
Breast development, soft skin,
increased body fat, skeletal
changes
Female Reproductive Anatomy:
o
o
o
o
o
o
Ovaries:
o produces eggs
o produces sex hormones estrogen & progesterone
o produces minimal amounts of androgens or testosterone (also in adrenal
cortex)
Oviduct (fallopian tube):
o Conducts eggs to the uterus (usually where fertilization occurs)
o fimbriae funnel like opening surrounded with cilia that sweep the egg towards
the uterus
Uterus:
o Houses and nurtures the developing fetus (implantation occurs)
o Endometrium is the inner layer that is supplied with blood vessels and is the
location where a fertilized egg attaches.
o Myometrium is the uterine muscle.
Cervix:
o a circular muscle that is the opening from the uterus to the vagina
o holds the growing fetus in the uterus in the later stages of pregnancy and must
dilate to allow the baby to be pushed out the uterus.
Vagina:
o Thin walled chamber serves as a repository for the semen
o Birth canal
o Lined by a mucous membrane and very elastic walls
o pH ~ 4-5
o Several days before ovulation the vagina begins producing mucus. This provides
a better environment for the survival and movement of the sperm cells.
External Genitalia:
o Vulva consists of the labia major and the labia minor
o Protects the clitoris, erectile tissue, & produces secretions for lubrication
Oogenesis (gametogenesis):
o Each ovary has about 2 million eggs at birth, only 300,000 survive to puberty and only
450 mature throughout the reproductive life span of the woman
o Follicles are sacs containing the oocytes (immature egg cells)
o The eggs are haploid, produced by meiosis.
o Unequal division of the cytoplasm results in only one cell surviving of the 4
daughter cells.
o The other 3 cells, called polar bodies, degenerate
Oogonia
(Diploid)
Meiosis
Polar Bodies
(Haploid)
46
2x
46
92
23
÷2
÷2
46
Oocyte
(Haploid)
o
o
o
23
23
23
During the development of the egg the follicle cells produce estrogen.
After ovulation left over structures in the follicle, now called the corpus luteum, now
produce progesterone
If fertilization occurs the corpus luteum lasts 3-6 months, otherwise lasts about 10 days
Regulation of Female Sex Hormones:
Hypothalamus
GnRh
Anterior
Pituitary
Secondary sex
characteristics
Thickening of
endometrium
Excites
myometrium
(uterine
muscle)
FSH
LH
Ovarian
Follicle
Estrogen
Mature
Follicle
Ovulation
Ruptured
Follicle
Corpus
Luteum
Progesterone
& Little
Estrogen
Maintains
endometrium
Calms
myometrium
activity
FSH stimulates egg production
LH stimulates release of the egg (ovulation)
Estrogen develops and maintains the female reproductive structures, thickens the
endometrium, causes secondary sex characteristics
Progesterone works with estrogen to prepare (maintain) the endometrium for
implantation, prepares the breasts to secrete milk, and inhibits uterus contractions during
pregnancy
Prolactin milk production during breast-feeding (nerves in the nipple are stimulated by
baby suckling which causes the pituitary to release prolactin)
Oxytocin contraction of the muscles of the uterus during labor. Progesterone inhibits the
pituitary production of oxytocin
Testosterone/Androgen (produced in the ovaries & adrenal cortex)
Menstrual Cycle:
Estrogen, progesterone, FSH, and LH all interact in the female reproductive system to
produce the menstrual cycle.
Four Phases:
Flow Phase (Menstrual Phase): first few days (1-5)
o Estrogen and progesterone are at their lowest causing the endometrium to be
shed (menstruation)
Follicular Phase: days 6-13
o Period of repair and preliminary thickening of the endometrium.
o FSH promotes follicle development in the ovary.
o As follicle develops it produces estrogen it causes the endometrium to begin to
grow again.
High estrogen levels increase LH production and decrease FSH
production.
Low estrogen causes the pituitary to produce FSH.
Ovulation: day 14
o LH causes an egg to released from the follicle
Luteal Phase: day 14 to day 28
o Final preparation of endometrium to receive the fertilized ovum
o LH stimulates development of the Corpus Luteum.
o Corpus Luteum causes progesterone and estrogen levels to increase.
o Estrogen and progesterone inhibit GnRH, thereby decreasing LH and FSH
levels.
o This low level of hormones initiates the flow phase and the cycle starts all over.
o If implantation does occur then the embryo begins producing HCG that
stimulates the corpus luteum to continue to produce progesterone, preventing
menstruation, and the menstrual cycle is suspended during pregnancy
Menopause:
Between ages of 45 and 55, the uterine and ovarian cycles cease.
Ovaries no longer respond to gonadotropic hormones (FSH & LH) from the AP.
Ovaries no longer secrete estrogen or progesterone
While the body adapts to hormonal changes women may experience any of circulatory
irregularities (hot flashes), dizziness, insomnia, sleepiness and depression. Osteoporosis: loss
of Calcium and bone mass due to a decrease in estrogen
Great variation among women, hormone replacement therapy may help some
Estrus cycle: “heat”
Most mammals have mating seasons, usually in the fall or spring.
Reproductive cycle found in other mammals that does not involve a menstrual flow
phase.
males are capable of breeding year-round
females will mate only when they are in “heat” or estrus
o frequency of estrus varies from mammal to mammal:
1/year = deer
1/6 months = dogs
1/3 weeks = cows, horse, and pigs
1/4 days = mice.
o During the estrus phase the females’ urine contains chemicals that indicate
estrus is taking place. The male can detect these chemicals often resulting in
competition for breeding among males.
Hermaphrodites:
Organisms that posses both male and female reproductive organs (primarily the ovaries
and testes).
Some can self fertilize, but most do not.
Examples include earthworms.
Fertilization: (Fusion)
fertilization usually takes place in the upper portion of the fallopian tube
fertilization can only occur within a span of 24 hours after ovulation
most of the sperm cells die, a few thousand may meet the ovum
enzymes in the acrosome of the sperm cells dissolve the corona (cells) around the egg this usually
requires many sperm cells
only one sperm cell breaks through the membrane surrounding the ovum (pellucida)
once a sperm cell enters the membrane changes so no other sperm cells may enter (the enzymes
are unable to dissolve it further)
the fertilized egg is called a zygote (single cell)
Twins:
Fraternal: two separate ova are fertilized by two different sperm. (Two different placenta)
Identical: one ovum fertilized by one sperm. (One placenta). Same genetic traits.
Conjoint: one ovum, one sperm, and the cell mass separates partly
Implantation:
During implantation, the outer layer of cells (chorion) produces a gonadotropic
hormone, HCG (human chorionic gonadotropin) which destroys the cells and blood
vessels of the endometrium.
HCG prevents degeneration of the corpus luteum (up to 4-9 months) and stimulates it to
secrete larger quantities of progesterone, which maintains the uterine lining and
prevents contractions
pregnancy tests identify the presence of HCG in the urine of women
Embryo Development:
Zygote (single cell) undergoes mitosis becoming a hollow ball of cells, now called a
blastocyst, as it travels down the fallopian tube (3 to 5 days).
o If it attaches in the fallopian tube this is called an ectopic pregnancy and must be
terminated
o Will embed into the endometrium, occurs about 2 to 4 days after it reaches the
uterus (about a week after fertilization)
The inner layer of cells of the blastocyst will form the embryo.
Gastrulation: formation of germ layers within the embryo (differentiation)
All body systems develop from the three germ layers:
o Endoderm: digestive, endocrine glands and respiratory organs
o Mesoderm: reproductive systems, muscle, bone and blood vessels (circulatory
system)
o Ectoderm: epidermis (skin, hair, etc) and the nervous system.
The outer cell layer of the blastocyst will form the extra embryonic membranes:
o Chorion
Embryonic portion of the placenta.
It produces important hormones (HCG, estrogen, and progesterone).
Surface for exchange of nutrients, minerals, hormones, antibodies,
gasses and wastes between the fetal and maternal blood supplies.
o Yolk sac
Source of red blood cells before the embryo produces its own.
Supply nutrients to bird, reptile and amphibian embryos.
Form a portion of the digestive tract, and is the source of the primordial
germ cells
o Amnion
This fluid-filled sac that surrounds the embryo
Cushioning the embryo from impact to the mother,
Temperature control
Protection from infection,
Enhancing muscle development, joint development and neural
connections by allowing the fetus to move more freely.
Fetal Development:
Gestation Period: The period of time the embryo/fetus is developing in the uterus. Divided
into three, three month segments called trimesters. (40 weeks)
Trimester
First
From
fertilization to
end of the third
month
Second
From third to
sixth month
Third
From sixth to
ninth month.
Embryo/fetal development
2nd Week: Three germ layers form. (Gastrulation)
4th Week: Heart has formed, arms, legs, fingers, toes start to form.
8th Week: Bone tissue begins to form
End of First Trimester: Arms and legs are formed and can move.
Placenta is grown enough to make its own progesterone. HCG
declines and progesterone increases maintaining the endometrium,
placenta, and the embryo is now called a fetus
All organs have formed and begin to function. Bones form. Fetus
grows from about 57 mm to 350 mm and 680 g.
A period of rapid growth, the fetus increases in size and mass as all
organs and systems become more developed. At birth the baby is on
average 530mm and 3400g.
Placenta:
Placenta forms a physical barrier between the mother and the fetus. (no blood cell mixing)
Osmotic exchanges of chemicals like organic chemicals, oxygen, water, drugs, alcohol, viruses,
and antibodies can move into the fetus, and wastes, water, and carbon dioxide can move out of
the fetus.
Attached to the fetus through the umbilical cord attached at the navel.
o Umbilical artery: carries fetal blood and wastes to the placenta to be exchanged with
nutrients and oxygen from the mother
o Umbilical vein: oxygenated blood with nutrients are brought from the placenta to the
fetus
Allantois – Extra-embryonic layer -> umbilical cord
Teratogens:
Environmental agents that induce developmental abnormalities in the growing embryo
and fetus.
Cross over from the maternal blood into the embryo/fetal blood in the placenta.
Examples:
Teratogen
Most common congenital abnormaltiies
Streptomycin
Hearing loss
Testosterone
Masculinization of external female genitalia
(high doses)
Cigarette smoke
Pregnancy loss, low birth weight
Chronic
Fetal alcohol syndrome, growth and developmental retardation,
alcoholism
abnormal facial features
Parturition: Labour and Delivery ~ 266 days after conception (fertilization)
Birth occurs in 3 stages:
1. Dilation: 2-24 hours
Opening of the cervix enlarges from 0cm to 10cm (fully dilated)
2. Deliver: 5 – 60 min
Contractions of the uterus combine with voluntary pushing by the mother to push the baby
out of the uterus (head first) and through the vagina.
3. Discharge of the Placenta (afterbirth): 1 – 60min
Uterus continues to contract to cause the placenta to be removed, this is the afterbirth.
Hormones used during birth:
o Oxytocin:causes contractions of the uterus
released by the pituitary
o Relaxin: inhibits progesterone production, brings about contractions of the uterus, and
relaxes the ligaments that hold the pelvic bones together allowing some expansion of the
birth canal.
produced by the placenta
o Prostaglandins: cause or intensify the contractions previous to birth (labor pains)
made by the uterus
Lactation: breast feeding
Hypothalamus and Pituitary Glands are stimulated when the baby sucks on the nipple
nerves in the nipple and areola.
Prolactin and Oxytocin are released into the blood stream causing both breasts to
release milk.
Milk contains important organic molecules (glucose, amino acids, lipids) as well as
antibodies.
Reproductive Technologies:
Prevention of pregnancy
Birth control pills:
o Usually simulate estrogen and/or progesterone.
o They inhibit the pituitary production of FSH and LH preventing any eggs/follicles
from developing or being ovulated.
Sterilization:
o Vasectomy:
o Removing a portion of and tying off the vas deferens to prevent passage of
sperm cells only.
o Tubal-ligation:
o Removing a portion of and tying off the fallopian tube to prevent passage of
eggs.
o Disadvantages of sterilization - hard to reverse
o
Barrier methods
o Some give protection against STIs
o Diaphragms, cervical caps, vaginal sponges, condoms, IUD
o "Natural family planning"
o Requires knowledge of the day of ovulation
o If known, can avoid the 4 days either side of ovulation to account for unusually long lived sperm or eggs.
o Women need exceptionally regular cycles to be effective
o "Basal" body temperature measurements (Temperature raises at ovulation), vaginal
pH measurements (more basic), mucus thickness can help time ovulation
Encouragement of pregnancy
Fertility drugs:
Usually simulate FSH and cause multiple eggs to develop in the ovaries
Artificial Insemination:
Sperm is introduced into the uterus of a women in a clinical procedure.
Artificial Involution:
Placing select embryos into surrogate mothers.
In vitro fertilization:
Involves the fertilization of an egg outside the uterus in a petri dish.
Eggs are extracted from the uterus and placed in a petri dish with sperm.
The resulting embryos are transplanted into the uterus and hopefully one will implant in
the endometrium
Technologies to Monitor Pregnancy:
Ultrasound:
The use of high frequency sound to make a picture/examine the developing fetus
Amniocentesis:
Involves taking a sample of the amniotic fluid that contains cells of the baby.
The cells are cultured (grown) so that the chromosomes can be examined (often a
karyotype is produced)
Chorionic Villus Sampling:
A small sample of the chorion is removed for analysis of the chromosomes in the
nucleus of the cells
Sexually Transmitted Infections:
STIs cause infections in the tubes that carry the sperm or egg (reproductive organs)
Cause temporary or permanent blockages or cessation of function of those organs
Gonorrhea:
o Bacterial infection
o Attacks urogenital tract and rectum, joints (arthritis), brain, and cardiovascular system.
o Male Symptoms: frequent urination and burning sensations
o Female Symptoms: similar to male symptoms however in females there might not be any
symptoms
o Scars form in the reproductive tract of both genders causing infertility
Chlamydia:
o Bacterial infection
o Same symptoms as gonorrhea
o Leads to pelvic inflammatory disease in females
o Males experience problems with the prostate gland and testes
Syphilis:
o Bacterial infection
o Attacks mainly the nervous system (insanity)
o Symptoms include sore throat, bone pain, fever, headaches, loss of hair, and sores in the
mouth
o Famous People: Beethoven, Columbus, Abraham Lincoln, van Gogh, Adolf Hitler
Herpes Simplex B – II:
o Viral Infection
o Causes small blisters to form on the genital area.
AIDS – HIV Infection:
o Viral infection
o Destroys the immune system
o Symptoms include weight loss, swelling of lymph glands, persistent cough.
Male Infertility:
Inability to make a female pregnant
Caused by:
o STIs
o Insufficient ICSH (low sperm count)
o Impotence (premature ejaculation or failure to obtain or maintain an erection)
caused by stress, fear, embarrassment, excessive use of alcohol.
o Malformation or absence of a part of the reproductive system.
Female Infertility:
Inability to get pregnant and carry a fetus to full term
Caused by:
o STIs
o Imbalance in gonadotropic hormones
o Failure to ovulate due to stress, diet, rigourous exercise, and breastfeeding.
o Weak cervix that can lead to a miscarriage
o Malformation or absence of a part of the reproductive system.