* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
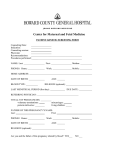
Download maternal and pediatric outcomes of pregnancy
Survey
Document related concepts
Women's health in India wikipedia , lookup
Birth control wikipedia , lookup
Reproductive health wikipedia , lookup
HIV and pregnancy wikipedia , lookup
Prenatal testing wikipedia , lookup
Prenatal development wikipedia , lookup
Women's medicine in antiquity wikipedia , lookup
Maternal health wikipedia , lookup
Fetal origins hypothesis wikipedia , lookup
Prenatal nutrition wikipedia , lookup
Maternal physiological changes in pregnancy wikipedia , lookup
Transcript
MATERNAL AND PEDIATRIC OUTCOMES OF PREGNANCY IN WOMEN WITH CYSTIC FIBROSIS A Thesis Presented in Partial Fulfillment of the Requirements for the Degree Master of Science in the Graduate School of The Ohio State University By Kallirroe Kelly Tzemos, B.S. Graduate Program in Allied Medical Professions ***** The Ohio State University 2011 Master’s Examination Committee: Dr. Kay N. Wolf, Advisor Dr. Christopher A. Taylor Dr. Marcia Nahikian-Nelms Copyright by Kallirroe Kelly Tzemos 2011 Abstract Cystic Fibrosis is a life-shortening autosomal recessive disorder, with the greatest prevalence in the Caucasian population. Advances in medical therapies and treatment of the disease have allowed for a progressively increasing life expectancy which now extends well into the third decade of life. Many women with cystic fibrosis choose to become pregnant and start families of their own, raising the question of what effect pregnancy may have on the disease state. A retrospective chart review was conducted to determine the relationship between pregnancy and the maternal and infant outcomes in women with cystic fibrosis, and describe the nutritional interventions received by these patients during their pregnancies. Subjects included women with cystic fibrosis who had at least one successful pregnancy during the time period from 1996-2011. Subjects were grouped based on severity of pre-pregnancy lung function and BMI. Results showed that there were no significant differences in maternal or pediatric outcomes based on prepregnancy BMI or FEV1 measures. Pre-pregnancy weight and FEV1 were identified as strong predictors of their individual measure 6-12 months after delivery. Outcomes of this study indicate that women with varying degrees of severity of CF can have successful pregnancies and produce healthy infants. It should be the goal of the CF team to provide appropriate pre-natal advice for women with CF who are considering pregnancy, and close monitoring with necessary medical care during pregnancy. The CF dietitian should make every effort to maximize the nutritional status of the pregnant CF patient, and provide a variety of interventions to promote adequate weight gain during pregnancy. Key Words: Cystic Fibrosis, BMI, FEV1 ii DEDICATION Dedicated to my parents Costas and Fay, and my sisters Maria and Alexandra. Thank you for all of your love and support. iii ACKNOWLDGEMENTS I would like to thank my advisor, Dr. Kay Wolf for her guidance, support, and patience throughout this entire process. This thesis would not have been possible without her direction and encouragement. I would like to thank the rest of my thesis committee; Dr. Taylor, and Dr. Nahikian-Nelms, for your involvement and support for this thesis. I appreciate your willingness to help and answer my many questions. I would also like to thank Susan Gemma and Anne Rice, who came up with the idea for this thesis. I have learned a great deal from you both, and I appreciate all of your support. Lastly, I would like to thank my family for pushing me to do as much as I can in life, and for being incredibly supportive throughout the entire Master’s degree and thesis process. iv VITA September 19, 1986… .....................................…………………..Born – Columbus, OH June 2009…………..………..……B.S. Allied Health Professions, Ohio State University 2009-2011 ......................................................…… Master’s program in Clinical Nutrition The Ohio State University FIELD OF STUDY Major Field: Allied Medical Professions v TABLE OF CONTENTS Page Abstract ............................................................................................................................... ii Dedication .......................................................................................................................... iii Acknowledgments.............................................................................................................. iv Vita.......................................................................................................................................v List of Tables ................................................................................................................... viii Chapters: 1. Introduction ........................................................................................................1 Background ..................................................................................................1 Significance of the Study .............................................................................3 Purpose .........................................................................................................3 Study Objectives ..........................................................................................4 Definition of Key Terms ..............................................................................5 Additional Terms .........................................................................................6 2. Review of Literature ..........................................................................................8 Background of Cystic Fibrosis.....................................................................8 Diagnosis of CF ...........................................................................................9 Nutrition Management of CF .......................................................................9 Energy Needs During Lung Infection ........................................................10 Fat-Soluble Vitamins .................................................................................11 Cystic Fibrosis Related Diabetes ...............................................................11 Risks of Pregnancy for Women with CF ...................................................12 Nutrition Management for Pregnant CF Patients.......................................15 Gestational Diabetes Mellitus and Glucose Intolerance ............................16 Vitamins and Pregnancy ............................................................................17 Social Considerations.................................................................................18 vi Health Status After Pregnancy ...................................................................20 Lactation ....................................................................................................21 Pre-term Delivery.......................................................................................22 Low Birth Weight ......................................................................................23 3. Methodology ....................................................................................................25 Research Design.........................................................................................25 Instrumentation and Data Collection .........................................................26 Outcome Measures.....................................................................................26 Data Analysis .............................................................................................27 4. Results and Tables. .......................................................................................28 Content of Nutrition Counseling with RD………………………………....40 5. Maternal Outcomes of Pregnancy in Women with Cystic Fibrosis Abstract .....................................................................................................42 Introduction ................................................................................................44 Methods......................................................................................................46 Statistical Analysis……………………………………………………….47 Results ........................................................................................................48 Content of counseling by the Registered Dietitian....................................55 Discussion ..................................................................................................56 Conclusion .................................................................................................60 Article References......................................................................................63 Appendix A – Pregnancy Questionnaire…………………………………65 Appendix B – Data Collection Sheet………………………………….…66 References…………………………………………………………….….68 vii List of Tables 4.1 Description of Subjects ..................................................................................................... 29 4.2 Pregnancy Outcomes Based on Pre-pregnancy BMI ........................................................ 30 4.3 Pregnancy Outcomes Based on Pre-pregnancy FEV1 ........................................................ 31 4.4 Pregnancy Weight Gain .................................................................................................... 32 4.5 Weight status 6 Months Post-partum ................................................................................ 32 4.6 Diagnosis of CFRD Prior to Pregnancy ............................................................................ 33 4.7 Diagnosis of Gestational Diabetes .................................................................................... 33 4.8 Need For Insulin Management of GDM ........................................................................... 33 4.9 Hospitalizations During Pregnancy .................................................................................. 34 4.10 Need for IV Antibiotic Therapy ........................................................................................ 34 4.11 Number of Visits with RD During Pregnancy .................................................................. 34 4.12 Lactation Frequency ......................................................................................................... 35 4.13 Lactation Subject Characteristics ...................................................................................... 35 4.14 Pre-Pregnancy and Post-Partum Weight Correlations ...................................................... 36 4.15 Pre-Pregnancy and Post-Partum FEV1 Correlations ......................................................... 36 viii 4.16 Pre-Pregnancy BMI and Outcome Correlations ............................................................... 37 4.17 Pregnancy Weight Gain and RD Visits ............................................................................. 37 4.18 Need for IV Antibiotic Therapy Differences in BMI and FEV1 ....................................... 38 4.19 Diagnosis of GDM, Differences in Weight ....................................................................... 38 4.20 BMI and FEV1 Changes Based on Weight Gain ............................................................... 38 4.21 Infant Outcomes ............................................................................................................... .39 5.1 Women with Cystic Fibrosis – Pre-pregnancy and Post-pregnancy characteristics….….50 5.2 Correlations of pregnancy outcomes of women with CF with pre-pregnancy FEV1 and BMI………………………………..………………………………….…………….……53 5.3 Maternal outcomes of pregnancy based on breastfeeding in women with CF…………..54 ix Chapter 1 Introduction and Background Cystic Fibrosis (CF) is an autosomal recessive disorder which causes an abnormal transport of chloride, sodium and water across the epithelial cells of the body (1). These alterations in the sodium and chloride channels cause thick, sticky mucus secretions in the lungs and other body organs. Bacterial colonization in the lungs often leads to chronic airway infection, decline in lung function, and respiratory failure (2). In addition to compromised pulmonary function, patients with CF struggle with a variety of gastrointestinal symptoms including malabsorption of nutrients which often leads to poor weight gain and malnutrition (3). Approximately 5% of Caucasian North American and European populations are carriers of the gene, with an incidence of 1 in 2500 live births having CF (2). Over the last 40 years advances in detection and treatment of CF have led to a dramatic increase in life expectancy for persons with CF, and in 2008 the median age of survival reached 37.4 years with 46% of the CF population age 18 or older (3). As the number of patients living into adulthood grows, pregnancy in women with CF is becoming increasingly common. Historically, women with CF were advised against pregnancy as it was thought to have devastating effects on their disease process and increased rates of mortality (4). This thought has changed however, as there have been increasingly more reports of successful 1 pregnancies with positive outcomes for both the mother and baby. Certain pre-pregnancy health factors such as mild pulmonary disease and good weight status have been identified as having a greater association with positive outcomes and lower risk to mother and baby, indicating the need for pre-pregnancy evaluation to determine if the health status of the mother is appropriate for pregnancy at that time (5). The high metabolic demands related to chronic airway infection in addition to varying levels of gastrointestinal malabsorption place the majority of patients with CF in a constant struggle to gain and maintain an appropriate body mass index (1). All pregnant women must be able to gain adequate weight during pregnancy to support the developmental requirements of the fetus, and this may be more challenging for the woman with CF. Maternal weight gain and nutritional status during pregnancy is associated with fetal growth and infant birth weight. Low birth weight (LBW) is defined as a live birth less than 2.5kg (6). Neonatal birth weight is a key determinant of infant survival, health and development. A low birth weight puts an infant at greater risk for developmental disability and for diseases such as cerebral palsy, visual problems, learning disabilities, and respiratory problems. Maternal nutritional status before and during pregnancy is recognized as one of the most important predictors of maternal and fetal outcomes, therefore it is important for women to receive pre-pregnancy nutritional counseling as well as appropriate nutritional care during and after pregnancy. 2 Significance of the Study The greater life expectancy in the CF population has led to an increase in the number of women with CF who decide to become pregnant and start families. Women with CF are at a constant risk for inadequate weight gain, decreased lung capacity, diabetes, and malabsorption of necessary nutrients. These same health risks put women with CF and pregnant in danger of having a baby born at a significantly low weight or furthering complications of her own health. The health complications associated with pregnancy and CF include diminished lung function, the risk of developing gestational diabetes, inadequate weight gain and poor nutritional status of the mother, which can ultimately affect the health of the infant. The aim of this study was to identify the effect of pregnancy on the course of the cystic fibrosis disease and to establish standards of nutritional care received by women with CF before, during, and after their pregnancy. Purpose of the Study The purpose of this retrospective study was to determine pregnancy outcomes and nutrition-related interventions of pregnant women with cystic fibrosis and establish standards of care for pregnant patients with CF in the future. 3 Objectives of the Study A retrospective chart review was used to: 1. To identify the relationship between the CF disease and the maternal outcomes of pregnancy including weight status and lung function. 2. To determine the relationship between the CF disease and infant outcomes of pregnancy including gestational age and birth weight. 3. To identify the nutritional interventions provided during the pregnancy of women with CF. 4 Definition of Key Terms 1. Maternal Pregnancy Outcomes Operational Definition – Maternal pregnancy outcomes are defined as measurable factors that are affected by pregnancy and influenced by maternal health status. These include weight gain during pregnancy, changes in lung function, and development of gestational diabetes. 2. Infant Outcomes Operational Definition – Infant outcomes are defined as measurements at time of birth which are influenced by maternal health status. These include infant birth weight and gestational age. 3. Nutritional Intervention Operational Definition – Nutritional intervention is defined as patient interaction with a dietitian during time of pregnancy, covering topics related to improvement of nutritional status. These topics include adequate weight gain, need for oral supplements, levels of vitamins and other micronutrients. 4. Severity of CF disease Operational Definition – For this study, mild to moderate pulmonary disease is defined as lung function greater than 60% of patient’s baseline FEV1, without any additional chronic 5 infection. Severe pulmonary disease is defined as lung function below 60% of patient’s baseline FEV1, with or without additional chronic respiratory infection. Additional Terms Cystic Fibrosis (CF) – a recessive genetic disorder that causes thick, sticky mucus to build up in the lungs and other organs of the body. Cystic Fibrosis Transmembrane Conductance Regulator (CFTR) - a protein involved in the transport of chloride ions across cell membranes or the gene that encodes this protein. Body Mass Index (BMI) – ratio of weight and height used to determine appropriate weight status. Weight in kilograms divided by height in meter squared. Pancreatic Insufficiency - inability of the pancreas to produce and/or transport enough digestive enzymes to break down food in the intestine and to allow for proper absorption. Pancreatic Enzyme Replacement Therapy (PERT) – supplementation of pancreatic enzymes to aid in the absorption of food. Malabsorption – inability to adequately absorb nutrients from the intestinal tract into the bloodstream. Forced Expiratory Volume (FEV1) – volume of air expired by an individual in one second during a forced expiration. Measures airway narrowing. Forced Vital Capacity (FVC) - the volume of air that can forcibly be blown out after full inspiration, measured in liters. Sweat Chloride Test – Test to determine if a patient has cystic fibrosis. A chloride concentration >60 mEq/L indicates that the patient likely has CF. 6 Oral Glucose Tolerance Test (OGTT) – A test that measures the body’s ability to metabolize glucose by measuring the glucose levels of the blood 1-2 hours after patient has ingested a glucose load following a fasted state; often used to test for impaired glucose tolerance and gestational diabetes. 7 Chapter 2 Review of Literature Background of Cystic Fibrosis Cystic Fibrosis (CF) is the most common autosomal recessive disorder, with the greatest prevalence of the disease seen in Caucasian populations (1,2). CF is caused by a mutation on chromosome 7, involving the cystic fibrosis transmembrane regulator protein (CFTR). Over 1,000 different mutations of the gene have been identified, with the delta F508 presenting as the most common of the mutations. These mutations cause an abnormal chloride transport within the epithelial cells of the body, affecting the movement of sodium and water across the cell. The altered chloride and sodium channel results in thickened airway surface liquid secretions which affect the lungs and various other body organs. Thickened mucus secretions in the lungs create a prime environment for bacterial colonization which leads to chronic pulmonary disease. The lungs of CF patients are susceptible to infection of many different organisms, particularly Burkholderia cepacia, Pseudomonas aeruginosa, Haemophilus influenza and Staphylococcus aureus (1,2,5). Chronic airway infections lead to progressive decline in lung function and eventual respiratory failure, which is the cause of mortality in over 90% of patients with CF (1). Daily airway clearance treatments may include high frequency chest compression (vest therapy), hand percussions, or a hand8 held flutter device, all of which are used to loosen secretions in the lungs and reduce airway obstruction. Mucus secretions also block the pancreatic ducts, inhibiting the release of lipase, protease, and amylase which are pancreatic enzymes necessary for proper digestion and absorption of macronutrients. This malabsorption of nutrients is partially corrected with the use of pancreatic enzyme replacement therapy (PERT) prior to consumption of meals and snacks. Secondary complications of the disease include diabetes mellitus, cirrhosis of the liver, and low bone mineral density. Diagnosis of CF All 50 states now have newborn screening protocols, which include an immunoreactive trypsinogen (IRT) test as part of their newborn screens, and a positive IRT indicates the need for a sweat chloride test (7). The sweat chloride test is the current “gold standard” for the diagnosis of cystic fibrosis, and a sweat chloride result of greater than 60mmol/L is indicative of CF. This sweat chloride test is followed by genotyping, which confirms the diagnosis of CF. Historically hospitals were not required to screen for CF, so it is not uncommon for an individual to be diagnosed in adulthood. In the 1940’s the median age of survival for a patient with CF was less than 1 year. Fortunately, better understanding of the disease, along with earlier and more aggressive treatments, have raised the age to 37.4 years in 2008 (3). 9 Nutrition Management and CF Eighty-five to ninety percent of patients with CF have pancreatic insufficiency which causes diminished digestive enzyme release resulting in nutrient malabsorption and often leads malnutrition and poor weight gain (8). Gastrointestinal side effects include steatorrhea, abdominal pain, gas, intestinal obstruction, and rectal prolapse. Other common side effects include gastroesophageal reflux and peptic ulcer disease. Growth failure and weight loss are commonly seen among patients with CF. As most patients with CF struggle to maintain a normal body weight, nutrition therapy for these patients often includes a high calorie, high fat diet combined with appropriate pancreatic enzyme dosing. Patients are usually recommended to eat 120-150% of energy requirements for weight and age. Poor nutritional status can result from a variety of factors, such as inadequate caloric and nutrient intake, increased energy demands of the disease secondary to lung infection, and high levels of malabsorption with subsequent stool energy losses (2,8). Energy Needs during Lung Infection With energy requirements already higher than normal, during pulmonary exacerbations energy needs increase further to meet the metabolic response to infection. While it is necessary for patients to consume more energy during this time, appetite often decreases. In children, catch-up growth is usually inadequate and leads to a pattern of slow weight gain with episodes of weight loss during pulmonary infections. In adults there is also a commonly seen pattern of weight loss with decreased respiratory muscle 10 strength and impaired lung function. (2,8) The increased metabolic demands of the disease in conjunction with the diminished appetite during acute illness trigger these episodes of weight loss. It is recommended that the CF patient stay above their desirable body weight for age in between periods of acute illness in order to keep reserves of body fat for times high metabolic demand. The Cystic Fibrosis Foundation recommends that children under 18 maintain a BMI of at least 50% for their age, while adult females maintain a BMI of at least 22kg/m² and adult males maintain a BMI of at least 23kg/m². Fat-Soluble Vitamins Fat-soluble vitamins, which include vitamins A, D, E, and K are often malabsorbed in the individual with CF. Patients rely on vitamin supplementation to ensure that they meet adequate intake levels of these vitamins. It is recommended for fatsoluble vitamin levels to be checked at least annually to determine if additional supplementation is needed. Cystic Fibrosis Related Diabetes Mucus secretions in the pancreas of CF patients lead to an increased risk for a form of diabetes, known at cystic fibrosis-related diabetes (CFRD). Fatty infiltration in the pancreas causes blockage of the exocrine glands and leads to decreased insulin secretion. Decreased peripheral insulin sensitivity is common in CF patients (9). Impaired glucose tolerance without the diagnosis of diabetes is also typical in CF patients. Patients with diabetes may require insulin or oral hypoglycemic agents. Home blood glucose monitoring is often recommended. In some cases it becomes necessary for 11 patients to follow a structured meal and snack plan so as to achieve good control of blood glucose while continuing a high caloric intake in order to prevent diabetes-related weight loss. In the past, tight glucose control was not considered a priority as life expectancy was limited; however the now increased life expectancy has led to reports of long-term diabetes- related complications including nephropathy and retinopathy. It is known that poorly managed CFRD can also lead to hyperglycemia, lethargy, and weight loss, in addition to microvascular complications. Consistently high glucose levels are related to deterioration of clinical status including loss of weight and lung function. Considering the present struggle most patients have with maintaining their weight and needing adequate energy to complete their daily medical therapies, the health consequences of poorly managed CFRD could be even more detrimental than those related to diabetes alone. Therefore CFRD care is now considered an essential part of management for CF disease. Risks of Pregnancy for Women with CF As women with cystic fibrosis are living longer into their adult lives, the issue of fertility and pregnancy is one that must be discussed with female patients and their families. Historically, women with CF were thought to be less fertile than the non-CF population, however recent research has shown no evidence to support this (1). As patients with CF are living well into their fourth decade of life, an increasing number of women with CF choose to become pregnant. The number of pregnancies reported to the CF patient registry had increased to 209 by 2006 and 240 pregnancies by 2008 (3). Although the number of women deciding to pursue pregnancy has steadily increased, 12 there is still a significant risk of disease morbidity and mortality posed to the mother and fetus. A major concern regarding the effect that pregnancy will have on disease progression is the decline in lung function. Women with mild pulmonary disease are more likely to regain their pre-pregnancy pulmonary status with minimal adverse results to long-term prognosis. Women with moderate to severe lung disease, poor nutritional status, and other CF complications which contribute to poor clinical status are at higher risk during pregnancy (5). Risks include preterm delivery, low birth weight, decline in pulmonary function, need for antibiotic therapy, development of gestational diabetes or decline of pre-pregnancy CFRD, pulmonary hypertension, spontaneous abortion, and patient mortality. Despite the risks that are present, many women with CF have had successful pregnancies. A retrospective study conducted by Edenborough et al (10) examined changes in body weight and lung function during the course of pregnancy in 20 patients with CF. There were 18 completed pregnancies in 17 patients with a mean duration of 37 weeks. A general decline in lung function was observed with an average loss of 13% FEV1 over the course of pregnancy. One year after pregnancy the loss returned to only 5% below pre-pregnancy %FEV1. Four of the 17 patients died within 3 years after delivery, all of which had moderate to severe pulmonary disease and pre-pregnancy FEV1 of 50% or less. Another study conducted by Palmer et al (11) analyzed outcomes of 11 pregnancies in 8 women with CF. Five of the 8 women appeared to have no maternal deterioration during pregnancy and had an average pre-pregnancy FEV1 of 89%. The 13 other 3 women had a mean pre-pregnancy FEV1 of 59% and experienced decline in overall health during pregnancy, with one death at 2 months postpartum and another death at 24 months postpartum. The third woman did not regain her pre-gravid health status. These studies demonstrate that women with poor lung function pre-pregnancy are less likely to tolerate pregnancy than those with good lung function. Although there has not been an absolute cut-off in lung function measure for when pregnancy should be discouraged, these studies and others suggest that an FEV1 of at least 50-60% is associated with decreased risk of morbidity and mortality (10,11,12). In another study conducted by Tanser et al, 31 pregnant women with CF were analyzed, and there appeared to be no significant differences in outcomes between women with pre-pregnancy FEV1 greater than 50% and those with poorer lung function (13) . Nutritional status and body weight were not significantly different between the two groups. Three of the 31 patients died within one week of delivery and one patient died after a spontaneous abortion at 23 weeks gestation. Three of the four patients who died were colonized with Burkholderia cepacia. B. cepacia is associated with a reduced longterm survival in adult patients. This study demonstrated that there can be successful pregnancies with maternal lung function below 50%, however colonization with B. cepacia led to increased mortality. Research by Gilljam et al also identified better outcomes for patients who were negative for B. cepacia (14). Most of the literature agrees that pregnancy itself does not appear to have a detrimental effect on maternal health. Poor lung function, nutritional status, colonization with B. cepacia and presence of diabetes in both pregnant and non-pregnant women are associated with decreased longterm survival (4,5,10,11,13). 14 Nutrition Management for Pregnant CF Patients When a patient decides to become pregnant, pre-pregnancy counseling should be immediately pursued. The patient should meet with their CF specialists and determine the risks posed by their current health condition and what changes in medical care need to take place in order to prepare for pregnancy. Every effort should be made to educate the CF patient considering pregnancy. Nutritional status is considered one of the most important predictors of maternal and fetal outcomes, therefore the patient should be evaluated by the CF Registered Dietitian. Nutrition recommendations for the pregnant patient with CF are similar to those of the non-CF pregnant woman, which include close monitoring of weight status, vitamin supplementation, and impaired glucose tolerance. Energy requirements stay elevated with an additional 300 calories per day during the second and third trimesters (5). BMI at start of pregnancy should be close to 100% of desirable body mass as defined by the CF Foundation. Weight gain during pregnancy should be monitored closely by patient’s obstetrician as well as the CF team. Patients should be advised if weight gain appears to be too slow or too rapid. Slow weight gain has been associated with low birth weight, while rapid weight gain has been associated with higher incidence of gestational diabetes (10) . Weight gain is also dependent on pre-pregnancy weight status. The Institute of Medicine (IOM) of the National Academy of Science has issued weight gain guidelines for the general population during pregnancy based on maternal pre-pregnancy BMI. These guidelines suggest that women who are underweight (BMI< 18.5) gain 28-40lbs, 15 women who are of normal weight (BMI 18.5-24.9) gain 25-35lbs, women who are overweight (BMI 25-29.9) gain 15-25lbs, and women who are obese (BMI >30) gain 1120lbs (15). The study by Edenborough et al(10) revealed a mean weight gain of 5.7kg in the pregnancies of 17 women, which was subsequently lost after pregnancy. Weight status returned to that of pre-pregnancy at 1 year follow-up. The study recognized a negative correlation between need for caesarean section and pre-pregnancy %IBW. A review by Cohen et al (16) conducted a survey of 119 CF centers in North America, and gave details of 129 pregnancies in 100 women with CF. Their results demonstrated poor outcomes associated with maternal weight gain less than 4.5kg, including increased rate of preterm delivery, perinatal death, and maternal mortality. Gestational Diabetes Mellitus and Glucose Intolerance In addition to close monitoring of weight status, glucose tolerance must be assessed earlier in this population as pregnant women with CF are at a higher risk for developing glucose intolerance and gestational diabetes (GDM). In a study done by Hardin and colleagues (9), 8 pregnant women with CF were compared to 9 pregnant controls. Seven of the 8 women with CF developed GDM before the end of their second trimesters, and had significantly lower insulin secretion and more insulin resistance than the controls. All CF pregnant women experienced less weight gain during the first and second trimester, and all were treated with insulin once diabetes was diagnosed. Once insulin was started weight gain became similar to that of the non-CF pregnant women. A study by McMullen et al (17) reviewed the outcomes of 216 pregnant women with CF and found that the prevalence of diabetes more than doubled during pregnancy 16 (9.3% to 20.6%) and over half of the women (55%) who developed GDM needed to continue DM therapy after pregnancy, compared to only 35% of non-pregnant agematched controls with CF. Presence of DM was also associated with pulmonary function decline. From baseline to approximately 1 year after pregnancy, FEV1 decreased by 6.8% in the pregnant women, and 4.6% over the same time period in the non-pregnant controls. These results suggest that pregnant women with CF experience similar respiratory and health trends as non-pregnant women with CF over the same time period. This increased risk of GDM and related complications warrants the need for frequent glucose monitoring. The above studies suggest pre-pregnancy oral glucose tolerance testing using 100 grams glucose and 2 hour post prandial test before pregnancy and one OGTT during each trimester (5,9,17). Vitamins and Pregnancy Vitamin supplementation for pregnant patients with CF continues to include the fat soluble vitamins which are malabsorbed secondary to pancreatic insufficiency. Pregnant patients should have their fat-soluble vitamin levels checked at baseline and continue vitamin therapy as recommended by their CF center. Proper fetal growth requires additional folic acid, iron, and calcium which are included in prenatal vitamins. Typical recommendation during pregnancy is one prenatal vitamin in addition to one CF vitamin (high dose of fat-soluble vitamins) daily. Doses of vitamin A greater than 10,000 IU red day may be teratogenic, so patients on individual Vitamin A supplementation might be advised to discontinue for the duration of the pregnancy. Additional vitamin D supplementation is dependent on the patient’s vitamin D status, and levels below 32ng/dL 17 are considered deficient and warrant supplementary vitamin D intake (18). Over the past 20 years there have been increasing reported cases of infants born with rickets, which is directly associated with the mother’s vitamin D status (19). Considering that women with CF already have decreased absorption of this vitamin, it is necessary to follow Vitamin D status closely if a woman with CF is considering pregnancy. As optimal nutritional care during pregnancy is vital for the outcome of the mother and the fetus, early and aggressive intervention is recommended for most women with CF. Monitoring weight gain, glucose tolerance, vitamin intake and appropriate interventions will help improve the nutritional status of the mother and increase the likelihood of a successful pregnancy. Social Considerations for Family In addition to thinking about the physical demands of pregnancy, women with CF must consider the psychological and social implications of having a child. This includes the effect that their disease will have on the child, the effect a child will have on their ability to balance child-care with their myriad of daily therapies, and the impact that the child will have on the family who may be needed to care for the child, the mother, or both. The social and psychological impact of having a child should be discussed with the CF team, as the challenges of coping with the increased stress of motherhood may take a toll on the mother’s physical condition and her ability to care for herself. A study reviewing the reproductive decision-making of mothers with CF showed that the main factors for women considering pregnancy are: health risks, genetic risk to 18 offspring, psychological well-being of partner, and the financial and child-care responsibilities associated with impaired health and shortened life expectancy (20). Although this data reveals that some patients with CF are well aware of the issues they may face in parenthood, it is also documented that currently 40-50% of pregnancies in the general non- CF population are unintended, occurring without prior consultation of a healthcare professional or considering the pertinent social issues (20). After considering her own health risk, it is important for the mother to give thought to the increased risk of her offspring having CF. All infants born to mothers with CF will be carriers of the CFTR gene, but the risk of developing CF depends on the father. If the father is tested and found to be a carrier of the gene, the infant’s risk of being born with CF is 50%. If the father tests negative for the CF gene mutation, the chance the baby will have the disease is very small, as the result from genetic testing can never eliminate risk 100%. This becomes an important issue as an increased risk to the fetus might discourage a mother from pregnancy on the basis of not wanting her child to suffer with this disease as she may have. Genetic testing of the partner is becoming more common and it is recommended by the National Institute of Health that CF carrier screening be offered to all couples actively planning pregnancy. Although it is unpleasant to think that a mother will not be able to raise her child into adulthood, it must be considered by the CF mother. Due to the lower life expectancy of CF patients, the mother must make plans for care of her child in case of severe illness or death. For many women, this does not change their decision to become pregnant, but requires a strong support from family and planning for future care of the child. Living to 19 see their child grow up may even be seen as motivation for a mother to take better care of herself. Another issue that may become increasingly more prevalent is pregnancy in the CF patient following a double lung transplant. Although cases are still rare, a growing number are being reported. Currently, there appears to be little additional risk to the mother or the child, assuming that rejection and infection are treated properly if they occur, and enough time is allowed to pass following the transplant (1). As with all CF pregnancies, it is important for the CF team to provide as much information as possible for the patient to be able to make an informed decision about pregnancy, and provide the highest quality care regardless of what she chooses to do. Health Status After Pregnancy The mother’s health status after pregnancy is closely related to the severity of her disease before the pregnancy. A study done by by Fiel et al (12) reviewed information on 271 pregnant women with CF from the North American Cystic Fibrosis database, and attempted to determine whether specific factors put the health of a woman with CF at greater risk following a successful pregnancy when compared to non-pregnant CF controls. Specific factors that were analyzed included poor nutritional status prior to pregnancy, poor pulmonary status, multiple pregnancies, and diabetes requiring insulin. Evaluation of the data showed that in women with CF, the rate of decline in FEV1 two years after pregnancy did not differ significantly between the two groups. The three year survival rate was 94% for pregnant women and 91% for controls. The outcomes of this study demonstrated that general survival was worse for all women with CF who had poor 20 lung function and poor nutritional status, regardless of pregnancy status. The study also mentioned that women who become pregnant may improve their general care and have closer supervision by their physician. This may explain the why in some cases maternal health status, regarding CF specifically, improves during pregnancy. As an overall decline of pulmonary function is often seen during pregnancy, a general decline of FEV1 and FVC observed in patients with mild pulmonary disease is regained in most women postpartum (7). Patients with FEV1 of greater than 50-60% seem to do well with low reported rates of maternal mortality. Patients with FEV1 less than 50% have shown to have a higher rate of mortality and faster progression of the disease postpartum (10,11,12). In general, women who intentionally prepare themselves in terms of nutrition and pulmonary function before becoming pregnant, and continue strict therapies during and after their pregnancy, can expect to have better long-term survival (21,22). Lactation Studies show that the breast milk of mothers with CF is usually sufficient to provide the energy needs of their nursing infant (14). The electrolyte content of their breast milk is normal but the fat content is slightly lower than normal, specifically in essential fatty acids, however there is enough to nourish the infant. There are a variety of non-CF specific recommendations that should be followed by all women who decide to breastfeed their infants. Supplementation of Vitamin D is recommended for all breastfeeding infants, as breast milk is very low in Vitamin D. The American Academy of Pediatrics currently recommends that all breastfed infants be supplemented with 400 International Units of Vitamin D beginning at birth (19). Other nutrients that need to be 21 consumed in adequate amounts by the mother during this time include iron, zinc, and calcium. It is recommended that mothers continue to take their prenatal vitamin or a multivitamin if their diet is deficient. Mothers following a vegan diet should also take a vitamin B12 supplement, as their diet may not provide a reliable source of this vitamin and it is necessary for proper nervous system development in the infant. Mothers must also remember that during lactation they require higher caloric intake to balance the increased energy demands of milk production. Although many women consider this an advantage for losing the weight gained during pregnancy, women with CF must be careful not to lose weight too rapidly as they may continue to breastfeed long after they reach their pre-pregnancy weight, and it may be harder to maintain their weight status at that time. An additional 500 calories daily is recommended for breastfeeding mothers, which adds to the already high caloric requirements of women with CF. In most cases breastfeeding should be encouraged, and the weight and health status of both the mother and infant be followed regularly. Pre-term Delivery Prenatal death is higher for infants born to mothers with CF as a result of the increased rate of preterm delivery. Risks of premature birth include disabilities and complications in growth and mental development. The etiology of preterm labor is likely due to poor maternal nutritional status and poor weight gain during pregnancy. It is also thought that chronic hypoxia on the fetus may play a role in preterm labor, especially in women with severe pulmonary disease (4). In the study by Gilljam et al (14), the mean gestational age was 40 weeks with 6 out of 50 infants born preterm (<37 weeks 22 gestation). Of the infants born to mothers with pre-pregnancy diabetes, two of three were preterm. In the study by Palmer et al (11) four of the five infants born to mothers with mild pulmonary disease were born at term. All three of the infants born to mothers of moderate to severe pulmonary disease were born prematurely. The ability of the mother to carry her pregnancy to term appears to be related closely to her pre-pregnancy lung function, nutritional status and weight gain during pregnancy (1,7,14). Low Birth Weight Infants born to mothers with cystic fibrosis have a higher incidence of low birth weight. LBW is associated with infant mortality and morbidity. LBW babies are forty times more likely to die within their first four weeks of life than normal birth weight infants and three times more likely to have neurodevelopmental complications (6). Poor nutritional status of the mother and inadequate weight gain are associated with LBW infants. A study conducted by David and Hofferth (15) on non-CF pregnant women discovered a significant association between maternal weight gain during pregnancy and infant birth weight. Infants born to women who had inadequate weight gain during gestation (based on IOM guidelines) had a risk of infant death 2.23 times higher than that of infants born to mothers of normal pregnancy weight gain. In the study conducted by Palmer et al (11), infants born to mothers with pre-pregnancy weight status of 80% or less weight for height were at higher risk for LBW. Infants who were born prematurely were also at higher risk for LBW. The possible risks associated with pregnancy in the woman with CF are well documented in the literature. Further insight into the relationship between prenatal care, 23 particularly nutritional interventions, and maternal and fetal outcomes will help guide current practitioners to establish standards of care and nutrition protocols for this specific patient population. 24 Chapter 3 Methodology Research Design A retrospective chart review of 23 pregnancies in 18 women with cystic fibrosis was conducted to determine the effects of pregnancy on the mother's disease state. Women with CF who attended a CF center in the Midwestern United States hospital and had a completed pregnancy in the period from 1996-2011 were included in this study. Information was obtained from the patients' medical charts and questionnaires given to patients during CF clinic appointments. Approval for this study was obtained from the Hospital’s Institutional Review Board. Data that was collected included pre-pregnancy anthropometric and clinical data, including age, height, last pre-pregnancy body mass index, mean forced expiratory volume per one second for 12 months preceding pregnancy, and pre-existing cystic fibrosis related diabetes mellitus. During pregnancy, maternal weight gain, diagnosis of gestational diabetes mellitus, need for intravenous antibiotics, number of hospitalizations, number of visits with the CF dietitian and content of nutritional counseling, as well as last FEV1 measure before delivery were collected. Postpartum body mass index and lung function were collected based on first measures taken at least 6 months after delivery. Infant data included birth weight and gestational age. Type of delivery and decision to breastfeed were also analyzed. 25 To determine differences caused by disease severity, subjects were grouped based on severity of pulmonary disease, greater or less than FEV1 of 60%. To determine differences based on nutritional status, subjects were then grouped based on BMI of greater or less than 22kg/m2. Instrumentation and Data Collection Data regarding the patients’ health status and pregnancy outcomes were collected through paper and electronic chart review and patient questionnaires. Consent was obtained and questionnaires were completed during routine clinic visits. A sample questionnaire is included in appendix A, and includes questions that would not likely be documented in the subjects’ charts at the cystic fibrosis center, such as infant birth weight and gestational age. Anthropometric and other clinical data were collected from the chart review. A sample data collection sheet indicating specific sources of each data point in included in Appendix B. Outcome Measures: Pregnancy Outcomes that were measured include: Weight status before and after pregnancy Weight gain during pregnancy Pulmonary function before, during, and after pregnancy Development of gestational diabetes Infant gestational age Infant birth weight 26 Nutritional Interventions during pregnancy which were examined include: Interactions with CF dietitian during pregnancy Topics of nutrition counseling and specific interventions Other variables of interest that were analyzed: Hospitalization during pregnancy Need for IV antibiotics during pregnancy Vaginal delivery or caesarean section Decision to breastfeed and duration Data Analysis: Clinical data from this study were expressed as mean and standard deviation. Statistical analysis of data was conducted using SPSS software. Pearson product-moment correlation coefficient was used, as well as paired t-tests where indicated. Significance was set at <0.05, unless otherwise noted. The data were examined using each subject rather than each pregnancy to reduce bias towards subjects with multiple births. 27 Chapter 4 Results A retrospective chart review of 18 women with cystic fibrosis and child birth was conducted to determine the effects of pregnancy on the mother’s CF disease state. Based on the data collected for this study, the different variables were analyzed to determine if any differences were present in maternal outcomes of BMI and lung function and infant outcomes of gestational age and birth weight. The primary objectives were: 1. To identify the relationship between the CF disease and the maternal outcomes of pregnancy. 2. To determine the relationship between the CF disease and infant outcomes of pregnancy. 3. To identify the nutritional interventions provided during the pregnancy of women with CF. 28 Age at conception (yr) Age at delivery Height (cm) Weight (last pre-preg) Body mass index (k/m2) Body mass index (6-mo post pregnancy) BMI change from pre-pregnancy to 6-mo post Total weight gain during pregnancy (lbs) Total weight gain during pregnancy (kg) Post-pregnancy weight (6 mo. post partum) Difference in wt from pre-pregnancy to postpregnancy (kg) Length of time post-pregnancy for weight & FEV1 (months) % FEV1 average 1 yr prior Last %FEV1 measure prior to delivery First %FEV1 measure post 6 mo. post partum # of hospitalizations during pregnancy Infant Gestational Age # of visits with RD during pregnancy Lactation duration (weeks) Infant weight (g) Minimum 15 15 139 44.5 15.4 16.0 -4.7 Maximum 28 29 170 61.9 27.5 28.4 3.0 Mean 21.2 21.9 160 52.1 20.6 20.6 .0 Std. Deviation 3.84 3.92 8.2 4.66 2.64 2.55 1.67 10.0 4.5 40.7 -10.9 48.0 21.8 63.7 8.7 26.2 11.9 52.3 .3 9.72 4.42 5.82 4.20 6.0 14.0 7.7 2.16 30.4 33.0 29.0 119.5 107.0 107.0 81.7 80.0 78.8 21.95 19.50 20.76 .00 30 2 6 1360.8 3.00 41 6 52 3756.3 .89 36.5 4.2 23 2696.0 .963 2.66 1.31 16.28 575.21 Table 4.1 Description of subjects Table 4.1 describes the 18 subjects, with data for first pregnancy only (18 infants). Thirteen of the 18 subjects had one pregnancy, 4 of the 18 subjects had 2 pregnancies, and 1 subject had 3 pregnancies. One of the 14 subjects with one pregnancy had twins, however only one infant weight was used for data analysis. One subject had not reached 6 months post-partum at the time of data analysis so data for this subject is missing for the 6-month post outcomes. Mean age at conception of subjects was 21.2 years +/-3.84, with mean BMI of 20.6kg/m2 +/-2.64. 29 Maternal and Pediatric Outcomes by Severity of CF Disease Subjects were divided into two groups based on disease severity according to lung function and body mass index (BMI). When grouped according to BMI, subjects who had a BMI less than 22kg/m² (or below 50th percentile for age for subjects younger than 20 years) were placed in group 1, while subjects with BMI greater than 22 kg/m² (or above 50th percentile for age for subjects younger than 20 years) were placed in group 2. Group 1 BMI < 22 N=14 Mean 19.66 20.14 .47 1.35 Group 2 BMI > 22 N=4 Mean 23.82 22.36 -1.46 -3.53 P value* BMI (kg/m2) pre-pregnancy 0.002 BMI 6 months post-pregnancy 0.127 BMI change from pre to 6 months post pregnancy 0.037 Difference in weight from pre to 6 months post pregnancy 0.036 (kgs) Total Weight gain during pregnancy (lbs) 26.32 25.75 0.921 Post pregnancy weight (kgs) 53.09 49.75 0.327 %FEV1 average 1 year prior 80.6 85.6 0.697 First FEV1 measure 6 months post 80.36 73.50 0.576 Infant Gestational Age (weeks) 36.86 35.38 0.342 Infant Birth Weight (g) 2730.6 2569.3 0.635 *Significance was determined based on a P value of less than .05. Table 4.2 Pregnancy outcomes of women with cystic fibrosis based on pre-pregnancy BMI In the sample (n = 18), 14 women had a low pre-pregnancy BMI (<22), while 4 women had a BMI greater than 22. Of the 18 births, there was a significant difference between the mean scores for BMI pre-pregnancy for those who had an initial BMI below 22 (mean = 19.66) and those who had a BMI greater than 22 (mean = 23.82). However, there was no significance difference between the two groups six months post-pregnancy. While the two groups had no significant difference in weight gain during pregnancy, the 30 women with a low BMI had a significantly higher change in BMI (.47 increase in BMI) as compared to those with a normal pre-pregnancy weight (-1.46). Subjects were divided into two groups according to average FEV1 measure for the 12 months prior to pregnancy. Subjects with average FEV1 less than 60% were placed into group 1, while subjects with average FEV1 greater than 60% were placed into group 2. Group 1 Group 1 FEV1 < 60% FEV1 > 60% P value* BMI (kg/m2) pre-pregnancy N=3 Mean 18.90 N=15 Mean 20.92 0.787 BMI 6 months post-pregnancy 18.72 21.01 0.667 BMI change from pre-pregnancy to -.18 .09 0.282 6 months post pregnancy Total weight gain during pregnancy (lbs) 19.67 27.50 <0.001 Post-pregnancy weight (6 months post) 46.67 53.48 <0.001 Difference in weight from pre -.23 .37 0.289 to 6 months post pregnancy %FEV1 average 1 year prior 44.9 89.0 0.175 First FEV1 measure 6 months post 47.67 85.07 .072 Infant Gestational Age 35.67 36.70 0.038 Infant Birth Weight (g) 2485.4 2736.6 0.057 *Significance was determined based on a P value of less than .05. Table 4.3 Pregnancy outcomes of women with cystic fibrosis based on pre-pregnancy FEV1 In the sample of 18 women, 3 were at high risk (moderate-severe FEV1 status) due to a mean pre-pregnancy FEV1 of less than 60%, while 15 were at lower risk (mildmoderate FEV1 status) with a mean pre-pregnancy FEV1 of less than 60%. Interestingly, women who were in the high risk group experienced a slight increase in their FEV1 from pre-pregnancy to 6 months post (44.9% +/-13.4 to 47.7% +/-17.6), while women in the 31 lower-risk group experienced an overall decrease in their FEV1 (89.0% +/-14.6 to 85.1% +/-15.1), however these values did not reach statistical significance (p=0.175 and p=0.072, respectively). . These numbers suggest that while pregnancy and birth appear to not significantly affect FEV1 within 6 months after delivery, women will remain within their pre-pregnancy FEV1 range. Subjects with FEV1 >60% gained significantly more weight during pregnancy compared to subjects with FEV1 <60% (19.7lbs +/-10 and 27.5lbs +/-9.5, respectively). However pre-pregnancy and post-pregnancy weight between these two groups was not significantly different. Other Descriptors: gained <25 lbs Gained at least 25 lbs Frequency 7 11 Percent 38.9 61.1 18 100.0 Total 4.4 Pregnancy Weight Gain of women with cystic fibrosis Table 4.4 shows the distribution of women by weight gain of at least 25 pounds during pregnancy, as recommended by the Institute of Medicine. Seven of the 18 women gained at least 25 pounds during their first pregnancy (38.9%). Above pre-pregnancy weight Frequency 10 Percent 55.6 8 44.4 Below pre-pregnancy weight Total 18 100.0 Table 4.5 Weight status 6 months post-partum of women with cystic fibrosis 32 Table 4.5 shows the distribution of women who were able to maintain at least their pre-pregnancy weight status at 6 months after delivery. Of the 18 women, 10 were above their pre-pregnancy weight at 6 months after delivery (55.6%). No Frequency 17 Percent 94.4 1 18 5.6 100.0 Yes Total Table 4.6 Diagnosis of CFRD prior to pregnancy of women with cystic fibrosis Frequency Percent No 9 50.0 Yes 8 44.4 Previous DM Diagnosis 1 5.6 Total 18 100.0 Table 4.7 Diagnosis of gestational diabetes of women with cystic fibrosis Eight of the 18 women (44.4%) were diagnosed with GDM, excluding the one subject with previous CFRD diagnosis. No Frequency Percent Valid Percent* 14 77.8 82.4* Yes Total N/A 3 17 1 16.7 94.4 5.6 Total 18 100.0 17.6* 100.0 Table 4.8 Need for insulin for treatment of gestational diabetes of women with cystic fibrosis Three of the 8 subjects (37.5%) who were diagnosed with GDM during their first pregnancy required insulin therapy. 33 Frequency Percent 0 8 44.4 1 5 27.8 2 4 22.2 3 1 5.6 Total 18 100.0 Table 4.9 Hospitalizations during pregnancy of women with cystic fibrosis Eleven patients required at least one hospitalization during their pregnancy (55.6%). Four patients required two hospitalizations and one patient required 3 hospitalizations during the course of her pregnancy. The number of patients requiring hospitalizations in not particularly alarming, as doctors may have been more conservative in the medical care of pregnant patients with pulmonary exacerbation and preferred to administer IV antibiotics in the hospital rather than at home. Frequency Percent No 7 38.9 Yes 11 61.1 Total 18 100.0 Table 4.10 Need for IV antibiotic therapy during pregnancy of women with cystic fibrosis Eleven of the 18 subjects required IV antibiotics (61.1%) during pregnancy. This number is not alarming as it is common during the course of a year for a patient to need IV antibiotic therapy for a pulmonary exacerbation. No. of RD visits Frequency Percent 2 1 5.6 3 6 33.3 4 3 16.7 5 4 22.2 6 4 22.2 Total 18 100.0 Table 4.11 Number of visits with RD during pregnancy of women with cystic fibrosis 34 Decision to breastfeed infant Frequency Percent No 11 61.1 Yes 7 38.9 Total 18 100.0 Table 4.12 Lactation decision making of women with cystic fibrosis Eleven of the 18 patients decided to breastfeed their infants. Table 4.1 above shows the mean duration of breastfeeding for subjects who selected to do so was 23 weeks (minimum of 6 weeks, maximum of 1 year). Lactation Height (cm) Weight (last pre-preg) Body mass index (kg/m2) Body mass index (6-mo post pregnancy) BMI change from pre-pregnancy to 6-mo post Total weight gain during pregnancy (lbs) Total weight gain during pregnancy (kg) Post-pregnancy weight (1st measure 6 mo. post partum) Difference in wt from prepregnancy to post-pregnancy (kg) % FEV1 average 1 yr prior First %FEV1 measure 6 mo. post partum No N=7 Mean 159.0 53.1 21.2 21.2 SD 9.4 4.7 3.1 3.0 Yes N=11 Mean 160.4 50.4 19.6 19.8 SD 6.6 4.4 1.3 1.2 .0 2.0 .2 1.2 28.5 9.8 22.6 9.1 13.0 4.5 10.3 4.1 53.2 5.8 51.1 6.0 .0 5.0 .6 3.0 80.3 76.5 20.1 18.1 83.8 82.4 26.2 25.6 Table 4.13 Group Characteristics of women with cystic fibrosis who do breastfeed and those who do not breastfeed and outcomes Patients were grouped based on whether they breastfed their infants, and weight and lung function data were compared. Women who breastfed their infants had a lower mean BMI prior to pregnancy than women who did not breastfeed (19.6 compared to 21.2). Although the group of women who did not breastfeed had a greater average 35 weight gain during pregnancy, the two groups were very similar regarding mean difference in weight from pre-pregnancy to 6 months post pregnancy, and were both able to maintain their pre=pregnancy weight status. Post-pregnancy Weight (1st measure 6 mo. post partum) .700** Pre-pregnancy Weight r (last pre-pregnancy wt.) p .001 N 18 Table 4.14 Association between pre-pregnancy and post-partum weight of women with cystic fibrosis When comparing the subjects’ pre-pregnancy weight with the first weight measure 6 months post-partum, a moderate, positive relationship was observed (r=.700). This correlation suggests that the subjects’ pre-pregnancy weight status is a good indicator as to what the subjects’ weight status will be greater than 6 months after delivery. %FEV1 Post (First %FEV1 measure post 6 mo. post partum) r .949** %FEV1 Pre (% FEV1 average p .000 1 yr prior to pregnancy) N 18 **. Correlation is significant at the 0.01 level. Table 4.15 Association between pre-pregnancy and post-partum lung function Correlation When comparing the subjects’ average %FEV1 for 1 year prior to pregnancy with the first %FEV1 measure 6 months post-partum, a very strong positive relationship was observed (r=.949). This correlation suggests that the subjects’ pre-pregnancy average lung function is a very good indicator of their lung function 6 months after delivery. 36 r Total weight gain during pregnancy Body mass index (kg/m2) .061 p .808 N 18 -.163 First %FEV1 measure post 6 mo. post partum r p .518 N 18 r .273 # of hospitalizations during pregnancy p .274 N 18 Table 4.16 Association between pre-pregnancy body mass index and total weight gain during pregnancy of women with cystic fibrosis No significant correlation was observed when comparing pre-pregnancy BMI to weight gain, postpartum FEV1, or number of hospitalizations during pregnancy. A weak, positive relationship was observed between pre-pregnancy BMI and number of hospitalizations during pregnancy (r=.273: p<.05). RD Visits Total weight gain during pregnancy (kg) r .043 p .867 N 18 Table 4.17 Association between total weight gain during pregnancy of women with cystic fibrosis and number of visits with the dietitian There is no significant relationship between weight gain during pregnancy and number of visits with the dietitian. 37 N Yes IV ATB No IV ATB 11 7 Mean and SD Mean and SD P-value 19.1 +/- 1.98 Pre-pregnancy BMI 21.5 +/- 2.61 (kg/m2) Average %FEV1 79.8% +/- 22.37 84.6% +/- 22.68 (1 year prior) .674 .603 Table 4.18 Need for IV antibiotic therapy and differences in BMI and FEV1 of women with cystic fibrosis There was no significant difference in BMI or FEV1 observed between subjects who did and who did not need IV antibiotics during pregnancy. N Yes No 8 9 Mean and SD Mean and SD P-value Weight Gain During Pregnancy (lbs) 12.0 +/- 3.47 12.7 +/- 4.85 .753 Table 4.19 Diagnosis of gestational diabetes, and differences in weight gain of women with cystic fibrosis There was no significant difference in amount of weight gained between subjects who were and were not diagnosed with GDM, indicating that GDM is a risk for all pregnancy women with CF, regardless of pregnancy weight gain. N Gained < 25 lbs Gained > 25 lbs 7 11 Mean and SD Mean and SD P-value -.5 +/- 2.10 .4 +/- 1.33 .248 BMI change from pre-pregnancy to 6-mo post 72.7 +/- 25.64 87.4 +/- 18.25 .418 % FEV1 average 1 yr prior 85.8 +/- 15.04 .113 First %FEV1 measure post 6 67.9 +/- 24.78 Table 4.20 BMI and lung function change based on weight gain of at least 25lbs of women with cystic fibrosis When comparing changes in BMI and %FEV1 between subjects who gained greater than or less than 25 pounds during pregnancy, no significant differences in BMI or %FEV1 were observed between the two groups. 38 Infant Outcomes Infant Weight Infant Gestational Age 1 .898 Infant wt r Infant Gestational Age p N r 18 .898 <.001* 18 1 % FEV1 average 1 yr prior p N r p N r <.001** 18 .403 .097 18 .399 18 .450 .061 18 .313 Weight (last pre-preg) p N r .101 18 -.027 .206 18 .101 p N r p N r .916 18 -.279 .263 18 -.155 .689 18 -.173 .492 18 .042 Total weight gain during pregnancy (kg) Body mass index (k/m2) Body mass index (6-mo post pregnancy) p .539 .868 N 18 18 BMI change from pre-pregnancy r .203 .337 to 6-mo post p .419 .171 N 18 18 *Correlation is significant at the 0.01 level. Table 4.21 Infant outcomes based on maternal BMI, weight gain, and %FEV1 No significant correlations were observed for infant outcomes. Significant positive relationship was observed with infant gestational age and infant birth weight when these two variables were compared, excluding maternal factors. This data suggests that regardless of maternal disease severity, based on either lung function or BMI, infant weight and gestational age is not adversely affected. 39 Content of Nutrition Counseling with Dietitian As reported in table 4.17, there was no significant correlation between the number of visits with the dietitian and weight gain during pregnancy. Table 4.11 shows that subjects had between 2 and 6 visits with the CF dietitian during their pregnancy. It is interesting to note that there was a slight, negative relationship (although not significant) between visits with the RD and weight gain during pregnancy. This is likely due to a greater number of ill visits to clinic or hospitalizations, which led to more dietitian interactions. Topics discussed during nutrition counseling with the dietitian were similar among all subjects. Topics included vitamin and mineral needs during pregnancy, including folic acid, iron, and calcium. Patients who were not already taking a prenatal vitamin were recommended to begin doing so. In some cases patients were recommended to begin taking a separate calcium or iron supplement (n=3). All patients were already on a high calorie diet, however the dietitian increased their calorie goal by 300-500 calories to promote adequate weight gain during pregnancy. Three of 18 patients were given specific calorie goals during pregnancy, while 2 others were encouraged to keep food diaries. For one patient, adjustment in her pancreatic enzyme dose was recommended. Protein sources and high calorie snacks were recommended for most. High calorie recipes for milkshakes were provided for 2 patients. For 9 patients, high calorie oral supplements were recommended and samples were provided. Based on the results of the oral glucose tolerance test, 5 patients were counseled on carbohydrate-controlled diets. One patient with GDM was recommended a low40 carbohydrate high calorie, oral supplement. If the patient had no record of an oral glucose tolerance test up to that point, the dietitian recommended that she have one done. In the second and third trimesters the dietitians discussed the topic of breastfeeding with 7 patients and referred one patient to a certified lactation consultant. The dietitians also offered government-assistance programs for food and oral supplements to qualifying patients. Women were encouraged to take advantage of WIC during their pregnancy if they qualified, and to continue on the program after their child was born. 41 Chapter 5 Maternal and Infant Outcomes of Pregnancy in Women with Cystic Fibrosis Kallirroe K. Tzemos, RD, KayN.Wolf, PhD, RD, Christopher A. Taylor, PhD, RD, Marcia Nahikian-Nelms, PhD, RD, Susan Gemma, MS, RD, Anne Rice, RD. Background: Advancement in medical care for patients with CF has led to an increased life expectancy for the CF population. A growing number of women with CF are reaching reproductive age and having successful pregnancies. There are increased risks associated with pregnancy in this population, and concern remains regarding the effect that pregnancy in the woman with CF may have on maternal and infant health. Objectives: To determine the relationship between CF disease and maternal and infant outcomes and describe the nutritional interventions provided to women with CF during pregnancy. Methods: Retrospective chart review including all women with CF who had successful pregnancies between 1996 and 2011 who still attended the CF Center at a Midwestern Hospital. Measures collected include age, BMI, FEV1, weight gain during pregnancy, pre-existing CFRD, diagnosis of gestational diabetes, hospitalizations during pregnancy, need for IV antibiotic therapy, type of delivery, infant weight, gestational age, decision to breastfeed infant, and nutrition topics discussed during counseling with the CF dietitian. 42 Results: Eighteen women in the study had 23 successful pregnancies. Mean prepregnancy BMI was 20.6kg/m2 with a mean weight gain of 26.2lbs during pregnancy. Mean FEV1 was 81.7% for the 12 months prior to pregnancy. Pre-pregnancy weight and FEV1 were shown to be strong predictors of weight and FEV1 status postpartum. Women with pre-pregnancy FEV1 greater than 60% experienced significantly greater weight gain during pregnancy than women with pre-pregnancy FEV1 <60%.Women who gained at least 25lbs during pregnancy were shown to have significantly greater FEV1 measures before, during, and after pregnancy, compared to women who gained less. Women with a BMI <22 had mean increase in BMI of 0.5 after pregnancy, compared to women with an initial BMI >22 who experienced a mean decrease in BMI of 1.5. Infant weight and gestational age did not differ based on maternal factors, however there was a 40% rate of premature births, and 30% rate of low birth weight infants in this study. Conclusions: Maternal and infant outcomes are positive for most women with cystic fibrosis who have sub-optimal body max index. Pre-pregnancy maternal BMI and FEV1 remain strong predictors of these measures 6 months after delivery. Women with milder pulmonary disease may be more successful in gaining the recommended amount of weight during pregnancy, however all women are likely to return to their pre-pregnancy BMI status. Women with CF who chose to breastfeed are likely able to return to and maintain their pre-pregnancy BMI just as successfully as women who do not breastfeed. There is much variability in the health outcomes during pregnancy regardless of weight and pulmonary status, suggesting that all women with CF remain at risk for adverse health outcomes due to pregnancy and should be monitored closely and frequently during this time. Nutrition interventions to promote adequate weight gain and overall optimal 43 nutritional status for pregnancy should begin in the prenatal period, and continue throughout the patient’s pregnancy. Cystic Fibrosis (CF) is an autosomal recessive disorder which causes an abnormal transport of chloride, sodium and water across the epithelial cells of the body (1). These alterations in the sodium and chloride channels cause thick, sticky mucus secretions in the lungs and other body organs. Bacterial colonization in the lungs often leads to chronic airway infection, decline in lung function, and respiratory failure (2). In addition to compromised pulmonary function, patients with CF struggle with a variety of gastrointestinal symptoms including malabsorption of nutrients which often leads to poor weight gain and malnutrition (3,4). Data has shown an association between higher body mass index and better lung function in patients with CF. The Cystic Fibrosis Foundation recommends that patients with CF have BMI standards greater than the general population. The goal BMI for adult females is 22kg/m2. Over the last 40 years advances in detection and treatment of CF has led to a dramatic increase in life expectancy for persons with CF, and in 2008 the median age of survival reached 37.4 years with 46% of the CF population age 18 or older (5). As the number of patients living into adulthood grows, pregnancy in women with CF is becoming increasingly common. Historically, women with CF were advised against pregnancy as it was thought to have devastating effects on their disease process and increased rates of mortality (1,2,6,7). This thought has changed however, as there have been increasingly more reports of successful pregnancies with positive outcomes for both the mother and 44 baby (8,9,10,11,12). There are still increased risks to the health of both the mother and baby, including diminished maternal lung function, development of gestational diabetes, premature delivery, low birth weight, and both infant and maternal mortality (8,11,12). Prepregnancy health factors such as mild pulmonary disease and good weight status have been identified as having a greater association with positive outcomes and lower risk to mother and baby, indicating the need for pre-pregnancy evaluation to determine if the health status of the mother is appropriate for pregnancy at that time (4,7,8,9,10,11,12). Despite the risks that are present, many women with CF have had successful pregnancies. Previous studies have been published showing that pre-pregnancy body weight and lung function (especially FEV1), and maternal weight gain during pregnancy are useful in predicting maternal and fetal outcomes (8,9,10,11,12). The greatest focus of these studies is on severity of maternal lung function and the effect that severe pulmonary disease during pregnancy has on maternal and infant health. Women with CF tend to have a higher rate of pre-term infants when compared to the general population, and risks associated with pre-term birth and low birth-weight infants are of concern to the CF population (8,11,12,13). In this study, both lung function, body mass index pre-pregnancy and maternal pregnancy weight gain were used to determine relationships these factors may have on the mother and the fetus during and after pregnancy. The aims of the study were (i) to determine the relationship between CF and the maternal outcomes of pregnancy, (ii) to determine the relationship between CF and the infant outcomes of pregnancy, and (iii) to identify nutritional interventions provided to CF patients during their pregnancy. 45 Methods A retrospective chart review of 18 women with cystic fibrosis who had given birth was conducted to determine the effects of pregnancy on the mother's disease and newborn outcomes. Women with CF who attended a CF center in a Midwestern United States hospital and had a completed pregnancy in the period from 1996-2011 were included in this study. Information was obtained from the patients' medical charts and questionnaires given to patients during CF clinic appointments. Approval for this study was obtained from the hospital’s Institutional Review Board. Data that were collected included pre-pregnancy anthropometric and clinical data, including age, height, last prepregnancy body mass index, mean forced expiratory volume per one second for 12 months preceding pregnancy, and pre-existing cystic fibrosis related diabetes mellitus. Number of FEV1 measurements varied between subjects, depending on number of tests each subject had during that 12 months period, ranging from one subject who had only 2 FEV1 measurements, to one subject who had 12 measurements taken that year. FEV1 measures for the 12 months prior to pregnancy were averaged for each subject, resulting in one pre-pregnancy FEV1 measure per subject. Pre-pregnancy weight was the weight measured at the last clinic appointment prior to pregnancy. During pregnancy, maternal weight gain, diagnosis of gestational diabetes mellitus, need for intravenous antibiotics, number of hospitalizations, number of visits with the CF dietitian and content of nutritional counseling, as well as last FEV1 measure before delivery were collected. Timing of last FEV1 measure prior to delivery varied among subjects depending on when they had CF clinic appointments. All measurements 46 were taken during either 2nd or 3rd trimesters. Postpartum body mass index and lung function were collected based on first measures taken at least 6 months after delivery. Time frame for these measures ranged from 6 to 14 months post-partum, based on subjects’ first clinic appointment and measurements of weight and FEV1 at least 6 months after delivery. Infant data included birth weight and gestational age. Type of delivery and decision to breastfeed were also analyzed. To determine differences related to disease severity, subjects were grouped based on severity of pulmonary disease, greater or less than FEV1 of 60%. To determine differences based on nutritional status, subjects were then grouped based on BMI of greater or less than 22kg/m2. For subjects who were under the age of 20 at time of conception, BMI grouping was determined based on whether subject’s BMI was greater or less than 50th percentile on CDC growth chart for BMI for age. If BMI was greater than 50th percentile, subject was placed grouped adult subjects with adequate BMI in the “BMI >22 category”. To determine differences related to weight gain during pregnancy, subjects were divided based on weight gain of greater or less than 25 pounds, based on the Institute of Medicine’s recommended weight gain during pregnancy. Statistical Analysis Clinical data from this study were expressed as mean and standard deviation. Statistical analysis of data was conducted using SPSS software. Pearson product-moment correlation coefficient was used, as well as paired t-tests where indicated. Significance was set at <0.05, unless otherwise noted. The data were examined using each subject rather than each pregnancy to reduce bias towards subjects with multiple births. 47 Results The study included eighteen women with CF who had a minimum of one successful pregnancy during the time period 1996-2011. There were a total of 23 births, resulting in 24 live infants. Of the 18 subjects, 13 women had one pregnancy (one set of twins), 4 women had 2 pregnancies and one woman had 3 pregnancies. Outcome data for this study used only the first pregnancy to prevent bias towards women who had multiple pregnancies. Weight for only one of the two infants of the woman who had twins was used for the infant outcomes. The mean age at conception was 21.2 (+/-3.8 years). The mean weight was 52.1kg (+/-4.7), the mean BMI was 20.6kg/m2 (+/-2.5), and the mean FEV1 was 81.7% (+/-21.9), all of which were measured at the last CF clinic appointment prior to pregnancy. Total mean weight gain during pregnancy was 11.9kg (+/-4.4) and weight status 6 months after delivery was 52.3kg (+/-5.8). At the time of postpartum weight measure, 10 women (55.6%) were above their pre-pregnancy weight, while 8 women (44.4%) had dropped below their pre-pregnancy weight status. Last FEV1 measure prior to delivery was 80.0 (+/-19.5%) and mean FEV1 6 months after delivery was 78.8 (+/20.8%). Ten patients (55.6%) were hospitalized during pregnancy, with 5 patients (27.8%) requiring 1 hospitalization, 4 patients (22.2%) requiring 2 hospitalizations, and 1 patient (5.6%) requiring 3 hospitalizations during pregnancy. Eleven of the 18 patients (61.1%) required IV antibiotics during the course of their pregnancy. Eight patients (44.4%) were diagnosed with gestational diabetes mellitus, 3 of which required insulin therapy. All patients had at least 1 visit with the CF dietitian during their pregnancy, with 48 a minimum of 2 visits to a maximum of 6 visits. Three women (16.7%) gave birth via caesarian section. Pregnancy outcomes are shown in table 1. Subject data were analyzed based on groupings of BMI, disease severity, and minimum weight gain. 49 Total BMI under 22 kg/m2 BMI BMI <22 >22 P Weight gained during pregnancy FEV1 Measure <60% >60% N=3 N=15 0.576 24.7 (3.5) 25.3 (4) 158.3 (10.4) 46.9 (3.8) 20.5 (3.6) 21.2 (3.6) 159.8 (8.2) 53.1 (4.2) P <25 lbs >25 lbs N=7 N=11 0.062 20.7 (4.3) 21.4 (4.4) 155.4 (10.1) 49.5 (4.7) 21.5 (3.7) 22.2 (3.8) 162.2 (5.9) 53.7 (4) P N=18 N=14 N=4 21.2 (3.8) 21.9 (3.9) 159.6 (8.2) 52.1 (4.7) 22 (3.8) 22.8 (3.8) 162.3 (6.4) 51.7 (5.1) 18.3 (2.8) 18.8 (3) 150 (7.3) 53.3 (2.7) BMI (kg/m ) pre-preg 20.6 (2.6) 19.7 (1.8) 23.8 (2.8) 0.002 18.9 (3.1) 20.9 (2.5) 0.787 20.8 (3.9) 20.4 (1.6) 0.236 BMI (6 mo. post preg.) BMI change from prepreg to 6-mo post Total weight gain during pregnancy (lbs) Total weight gain during pregnancy (kg) 20.6 (2.5) 20.1 (1.7) 22.4 (4.3) 0.127 18.7 (3.1) 21 (2.4) 0.677 20.3 (3.9) 20.8 (1.3) 0.161 0 (1.7) 0.5 (1.2) -1.5 (2.4) 0.037 -0.2 (1.5) 0.1 (1.8) 0.282 -0.5 (2.1) 0.4 (1.3) 0.811 26.2 (9.7) 26.3 (10.2) 25.8 (9.2) 0.921 19.7 (10) 27.5 (9.5) 0.000 16.5 (4.5) 32.4 (6.4) 0.212 11.9 (4.4) 12 (4.6) 11.7 (4.2) 0.921 8.9 (4.6) 12.5 (4.3) 0.000 7.5 (2) 14.7 (2.9) 0.212 52.3 (5.8) 53.1 (6) 49.8 (4.9) 0.327 46.7 (6.2) 53.5 (5.2) 0.018 48.4 (5.4) 54.8 (4.8) 0.062 0.3 (4.2) 81.7 (21.9) 1.4 3.2) 80.6 (22.5) -3.5 (5.6) 85.6 (22.7) 0.697 -0.2 (3.4) 44.9 (13.4) 0.4 (4.4) 89 (14.6) 0.175 -1.1 (5) 72.7 (25.6) 1.1 (3.6) 87.4 (18.2) 80 (19.5) 79.1 (21.1) 83.3 (14.6) 0.720 54.3 (23.2) 85.2 (14.7) 0.155 71.7 (21.5) 85.3 (17) 78.8 (20.8) 2696.0 (575.6) 36.5 (2.7) 80.4 (21.3) 2730.0 (564.2) 36.9 (2.6) 73.5 (20.7) 2568.5 (689.0) 35.4 (2.9) 47.7 (17.6) 2486.3 (504.6) 35.7 (1.5) 85.1 (15.1) 2735.7 (595.4) 36.7 (2.8) 67.9 (24.8) 2375.7 (584.0) 34.9 (3) 85.8 (15) 2897.3 (490.4) 37.5 (1.9) Age at conception (yr) Age at delivery Height (cm) Weight (kg) last pre-preg 2 6 mo. postpreg wt. (kg) Difference in wt from pre to post preg. (kg) % FEV1 avg. 1 yr prior Last %FEV1 measure prior to delivery First %FEV1 6 mo. post preg. Infant wt (g) Infant gest. Age (weeks) 0.084 0.068 0.004 0.036 0.576 0.635 0.342 0.703 0.704 0.090 0.289 0.072 0.057 0.038 Table 5.1. Women with cystic fibrosis - pre-pregnancy and post-pregnancy characteristics 50 0.083 0.096 0.788 0.030 0.829 0.000 0.008 0.002 0.506 0.556 When grouped based by BMI of greater or less than 22, mean pre-pregnancy BMI for the two groups were 19.7kg/m2 (+/- 1.8) and 23.8kg/m2 (+/-2.8). Post-pregnancy, the mean BMI values for the two groups were 20.1kg/m2 (+/- 1.7) and 22.4kg/m2 (+/-4.3), respectively. A significant difference in BMI change was observed between the two groups from pre-pregnancy to post-partum, with a mean BMI increase of 0.5kg/m2 (+/1.2) in the BMI <22 group, and a mean BMI decrease of 1.5kg/m2 (+/- 2.4) in the BMI >22 group, with a p value of 0.037. Pre-pregnancy, the mean BMI values for the two groups were significantly different from each other (p=.002), however when compared post-pregnancy, the mean BMI values were no longer significantly different (p=0.127). These results show that based on BMI alone, women in the lower BMI group were able to maintain their pre-pregnancy weight by 6 months after delivery, while women in the higher BMI group experienced an overall decrease. Subjects who had a BMI less than 22 had a mean FEV1 of 80.6% for 1 year prior to pregnancy, which they were able to maintain 6 months after delivery (mean = 80.4% postpartum). Subjects with a BMI greater than 22 had a mean FEV1 of 85.6% for the year prior to pregnancy, which dropped to a mean FEV1 of 73.5% at 6 months after delivery. Between the two groups, FEV1 was not significantly different before or after pregnancy. When grouped by severity of pulmonary disease, of the 18 subjects, 3 (16.7%) were at high risk (moderate-severe FEV1 status) due to a mean pre-pregnancy FEV1 of less than 60%, while 15 were at lower risk (mild-moderate FEV1 status) with a mean prepregnancy FEV1 of less than 60%. Subjects with FEV1 >60% gained significantly more 51 weight during pregnancy compared to subjects with FEV1 <60% (19.7lbs +/-10 and 27.5lbs +/-9.5, respectively). However pre-pregnancy and post-pregnancy weight between these two groups was not significantly different. Women who were in the high risk group experienced a slight increase in their FEV1 from pre-pregnancy to 6 months post (44.9% +/-13.4 to 47.7% +/-17.6), while women in the lower-risk group experienced an overall decrease in their FEV1 (89.0% +/-14.6 to 85.1% +/-15.1), however these values were not statistically significant. (p=0.175 and p=0.072, respectively). These numbers suggest that while pregnancy and birth appear to not significantly affect FEV1 within 6 months after delivery, women will remain within their pre-pregnancy FEV1 range. Eleven of the 18 women (61.1%) gained at least 25 pounds during pregnancy (11.4kg), meeting the minimum pregnancy weight gain recommendation set by the Institute of Medicine. When grouped based on weight gain of at least 25lbs, results show that women who gained 25lbs or more during pregnancy had significantly higher FEV1 measures for the year prior to pregnancy (72.7% +/-25.6 and 87.4% +/-18.2, with a pvalue of <0.001). Women who gained at least 25lbs also had significantly higher FEV1 values when measured during pregnancy and at first FEV1 measure 6 months postpartum. Women in both weight gain groups were able to maintain their FEV1 from prepregnancy to post-partum, however the data suggest that women with FEV1 >60% had greater success in gaining weight during pregnancy. Weight gain during pregnancy was not associated with BMI status post-partum, nor was it related to more favorable infant outcomes of birth weight and gestational age. Weight gain during pregnancy also showed 52 no correlation to diagnosis of gestational diabetes, and diagnosis of GDM did not appear to have a relationship with infant outcomes in this group of women and their offspring. Pre-pregnancy FEV1 and BMI were shown to have strong positive relationships with their respective measures 6 months post-pregnancy. As seen in table 2, FEV1 before and after pregnancy had a correlation of r=.949 with p<0.001. These results suggest that pre-pregnancy lung function was a good predictor of postpartum lung function 6 months after delivery. Pre-pregnancy BMI also appeared to be a good predictor of postpartum BMI, with r=.700, and p=0.001. Correlations Maternal Outcomes Body mass index pre-preg. (kg/m2) Age at conception (yr) Age at delivery Weight (last pre-pregnancy) Body mass index (6-mo post pregnancy) BMI change from pre-pregnancy to 6-mo post Total weight gain during pregnancy (lbs) Total weight gain during pregnancy (kg) Post-pregnancy weight (1st measure 6 mo. post partum) Difference in wt from pre-pregnancy to post-pregnancy (kg) %FEV1 post-pregnancy (1st measure 6 months post) Infant Outcomes Infant Gestational Age Infant wt % FEV1 average 1 yr prior R (P) -0.04 (0.873) -0.43 (0.074) -0.43 (0.073) 0.18 (0.476) 0.11 (0.65) Prepregnancy BMI (kg/m2) R (P) 1 (0) -0.01 (0.962) -0.01 (0.972) 0.52 (0.026) 0.79 (0.001) 0.24 (0.34) 0.38 (0.117) 0.38 (0.117) -0.37 (0.129) 0.06 (0.808) 0.06 (0.808) 0.32 (0.196) 0.13 (0.615) 0.24 (0.33) -0.4 (0.096) .95 (<0.001) -.16 (0.518) 0.31 (0.206) -0.17 (0.492) 0.4 (0.101) -0.28 (0.263) Table 5.2. Correlations of pregnancy outcomes of women with cystic fibrosis with pre-pregnancy FEV1 and BMI 53 Seven of the 18 subjects (38.9%) chose to breastfeed their infants. Duration of breastfeeding ranged from 6 weeks to 1 year. The mean BMI of women who did not breastfeed their infants was 21.2kg/m2 +/-3.1 prior to pregnancy, and returned to 21.2kg/m2 +/-3.0 when measured 6 months after pregnancy. This group gained an average of 28.5lbs +/-9.8 during pregnancy. For women who did breastfeed their infants, mean pre-pregnancy BMI was 19.6kg/m2 +/-1.3 and returned to 19.8kg/m2 6 months postpartum. This group had an average weight gain of 22.6lbs +/-9.1. These data suggest that women who breastfed their infants were able to maintain their pre-pregnancy BMI just as successfully as women who did not breastfeed. Lactation Height (cm) Weight (last pre-preg) Body mass index (kg/m2) Body mass index (6-mo post pregnancy) BMI change from pre-pregnancy to 6-mo post Total weight gain during pregnancy (lbs) Total weight gain during pregnancy (kg) Post-pregnancy weight (1st measure 6 mo. post partum) Difference in wt from prepregnancy to post-pregnancy (kg) % FEV1 average 1 yr prior First %FEV1 measure 6 mo. post partum No N=7 Mean 159.0 53.1 21.2 21.2 SD 9.4 4.7 3.1 3.0 Yes N=11 Mean 160.4 50.4 19.6 19.8 SD 6.6 4.4 1.3 1.2 .0 2.0 .2 1.2 28.5 9.8 22.6 9.1 13.0 4.5 10.3 4.1 53.2 5.8 51.1 6.0 .0 5.0 .6 3.0 80.3 76.5 20.1 18.1 83.8 82.4 26.2 25.6 Table 5.3. Maternal outcomes of pregnancy based on breastfeeding in women with cystic fibrosis 54 Mean gestational age of infants was 36.5 (+/-2.7 weeks), with a range of 30 to 41 weeks. Mean infant birth weight was 2696.0 grams (+/-575.6), with a range of 1360.8 to 3742.1 grams. When maternal variables of body weight and lung function were compared to infant birth weight and gestational age, no significant correlations between these variables were observed. This data suggests that regardless of maternal disease severity, infant weight and gestational age is not adversely affected. A significant positive relationship was observed between infant gestational age and infant birth weight when these two variables are compared excluding maternal factors (r=.898 and p<0.001). Counseling by the Registered Dietitian Subjects had between two to six visits with the CF dietitian during their pregnancy. Topics discussed during nutrition counseling with the dietitian were similar among all subjects. Topics included vitamin and mineral needs during pregnancy, including folic acid, iron, and calcium. Patients who were not already taking a prenatal vitamin were recommended to begin doing so. In some cases patients were recommended to begin taking a separate calcium or iron supplement. All patients were on a high calorie diet, however the dietitian increased their calorie goal by 300-500 calories to promote adequate weight gain during pregnancy. Three of 18 patients were given specific calorie goals during pregnancy, while 2 others were encouraged to keep food diaries. For one patient, adjustment in her pancreatic enzyme dose was recommended. Protein sources and high calorie snacks were recommended for most. High calorie recipes for milkshakes were provided for 2 55 patients. For 9 patients, high calorie oral supplements were recommended and samples were provided. Based on the results of the oral glucose tolerance test, 5 patients were counseled on carbohydrate-controlled diets. One patient with GDM was recommended a lowcarbohydrate high calorie, oral supplement. If the patient had no record of an oral glucose tolerance test up to that point, the dietitian recommended that she have the test done. In the second and third trimesters, the dietitians discussed the topic of breastfeeding with 7 patients and referred one patient to a certified lactation consultant for more information. The dietitians also offered government-assistance programs for food and oral supplements to qualifying patients. Women were encouraged to take advantage of WIC during their pregnancy if they qualified, and to continue with the program after their child was born. Discussion The results of this study determined that mothers with CF were able to deliver babies without significant change to their nutritional or pulmonary status at least 6 months post-delivery. Unlike previous studies, the findings showed that regardless of pulmonary function severity, all women were able to retain their pulmonary function and nutritional status at 6 months to 1 year postpartum (8,9,10,11,12). When looking at the two groups of women in this study divided by lung function, there was no significant difference in BMI or FEV1 status postpartum between those with 56 a pre-pregnancy FEV1 greater than 60% and those with a pre-pregnancy FEV1 less than 60%. Women with greater lung function pre-pregnancy did gain significantly more weight during pregnancy than women in the lower FEV1 group. No difference was observed in infant outcomes between the two groups. Pre-pregnancy FEV1 did, however appear to be a good indicator of FEV1 status 6-12 months postpartum, indicating a generally stable pulmonary status during that time frame. In the study of 17 pregnant women with CF conducted by Edenborough et al (8), a general decline in lung function was observed in all women, with an average loss of 13% FEV1 over the course of pregnancy, and one year after pregnancy the loss returned to only 5% below pre-pregnancy %FEV1. In another study conducted by Tanser et al (14), 31 pregnant women with CF were analyzed, and there appeared to be no significant differences in outcomes between women with pre-pregnancy FEV1 greater than 50% and those with poorer lung function. Results of the present study support the findings of these studies in that women with CF are able to return to their pre-pregnancy FEV1, regardless of pre-pregnancy FEV1 status. When looking at BMI status before pregnancy, neither group of women (those with a BMI greater than 22 and those with a BMI less than 22) experienced a significant difference in FEV1 status when measured 6 months to 1 year postpartum. The results show that women with a BMI less than 22 experienced a slight increase in BMI and women with BMI greater than 22 experienced a decrease in BMI, however it is essential to consider the differences in group size, 14 subjects in the <22 group and 4 subjects in the >22 group, and important to note that the single largest decrease in BMI was 57 experienced by a subject in the >22 group. Her BMI loss of 4.7kg/m2 was more than 2 times the BMI change of any other subject, resulting in a greater mean loss of BMI for the entire group. Sixty-one percent of women in this study gained at least 25 pounds during pregnancy, based on the Institute of Medicine's recommendation of pregnancy weight gain. Average weight gain for all subjects during pregnancy was 26.2lbs (11.9kg), which is slightly greater than the weight gain reported by Gilljam et al (11) (10.4kg), and more than double the weight gain reported in the study by Edenborough et al (8) (5.4kg). In this study, women who gained at least 25 pounds were shown to have better lung function before, during, and after pregnancy than women who did not gain this amount. It is interesting to note that the women in the sub-optimal BMI group maintained an average lung function of about 80% from pre-pregnancy to post partum, while the women with a BMI greater than 22, began with a mean FEV1 of 85.6% which dropped to a mean of 73.5% at 6-12 months after delivery. Again it is important to consider the difference in group sizes. It is interesting to point out, however, that all 4 women in the >22 BMI group experienced a similar decrease in their lung function post partum. When comparing weight status and lung function to other pregnancy outcomes such as diagnosis of gestational diabetes, need for IV antibiotics, and hospitalizations during pregnancy, there was no significant correlation. Again, this finding differs from previous studies which reported a more severe disease process during pregnancy for women with FEV1 less than 60% (8,11,12,14). This is a positive finding for this group of women, as they are often discouraged from becoming pregnant if their lung-function is 58 sub-optimal. It is also important for all pregnant women with CF to consider that although they are likely able to maintain their BMI and lung function after pregnancy, they are still at risk for developing gestational diabetes, and requiring IV antibiotics or hospitalization for acute infection during pregnancy. This study also shows similar post-pregnancy weight outcomes between women who did breastfeed their infants and well as women who did not breastfeed. Despite the additional metabolic demand breastfeeding has on a woman’s body, women in the present study who breastfed their infants were able to maintain their pre-pregnancy BMI when measured 6-12 months postpartum, suggesting that breastfeeding does not have a negative impact on the mother’s weight status. Infant outcomes in this study were overall positive, and showed no difference based on health status of the mother. The percentage of infants born prematurely (<37 weeks) was 40%, which was slightly higher than the 35% reported by Edenborough et al (8) , and much greater than the 9% reported by Gilljam and colleagues (11). The number of infants born with a low birth weight (<2500 grams) was 30%, which did not differ greatly from the other two studies. It is important to note that all 7 of the infants who were born with a low birth weight in our study were also born preterm, indicating that they were not necessarily small for gestational age. The other 3 of the 10 infants that were born preterm weighed greater than 2.5kg. There was no correlation between nutritional or pulmonary status of the mother and her infant's birth weight or gestational age, so preterm delivery and low birth weight infants were not necessarily a result of disease severity of the mother. 59 Conclusions The results of the present study support the findings of recent studies which report that pregnancy can be well tolerated in the woman with cystic fibrosis (8,9,10,11,12,15). For the time frame studied, no detrimental effect on maternal health was observed. Maternal BMI and FEV1 status 6-12 months postpartum were comparable to pre-pregnancy BMI and FEV1. Women with higher BMI and FEV1 did not have different outcomes in weight or lung function following pregnancy compared to women with lower BMI and FEV1. The literature suggests that women with CF tolerate pregnancy better when they have mild pulmonary disease and good nutritional status (1,2,3,4,8,11,12,15). The data from this study suggest that women with CF can maintain their weight status and lung function following pregnancy, even if these measures are not optimal prior to pregnancy. It is likely that doctors advise their patients against pregnancy if they have severe pulmonary disease or poor nutritional status. It is common knowledge, however, that not all pregnancies are planned. Even with proper warning, a woman with severe CF may become pregnant, and at that time it is imperative for the CF team to do everything to improve the pulmonary and nutritional status of the patient. The CF dietitians should continue to counsel on topics of vitamins, minerals, and calorie needs, with an emphasis on adequate weight gain. The results of this study demonstrate that over half of the women gained at least 25lbs as recommended by the Institute of Medicine for maternal weight gain during pregnancy, with significantly greater weight gain seen in the FEV1 >60% group (13). Although this study did not show a difference in maternal or pediatric outcomes based on weight gain during pregnancy, a 60 significant relationship between weight status before pregnancy and weight status after pregnancy was observed. Lactation is encouraged in the non-CF population for the health benefits breast milk offers to the infant. Whether breastfeeding should be recommended to the CF mother is not clearly reported in the literature, as the increased metabolic demands of lactation may promote excessive and unwarranted weight loss. Based on the findings of this study, women who did not breast feed had gained more weight during pregnancy than women who did breast feed, yet both groups returned to their pre-pregnancy weights 6 months post-partum. This suggests that women who decide to breastfeed their infants are able to maintain their post-partum weight just as well as women who do not breastfeed. Based on these findings, the CF dietitian should educate all pregnant women with CF on the benefits of breastfeeding, and encourage them to make their decision with less worry that breastfeeding may have a negative impact on their weight status. The primary limitation of this study is the difference in group size when subjects were grouped based on BMI and lung function. One group was 3-4 times larger than the other in both cases, and this likely had significant effect on statistical power. A large change in BMI or FEV1 in just one subject significantly changes the mean outcome for the entire group. The overall group size was also small, with only 18 subjects. To further understand the long-term effects of pregnancy on the health of a woman with CF, a study which analyzes BMI and lung function for several years after pregnancy is warranted. This study measured only outcomes in BMI and FEV1 until approximately 6 months after delivery, which was likely long enough to show the direct physical effect pregnancy has 61 on the body of the woman with CF. This study does not show long-term changes in health after pregnancy, which are often associated with changes in the daily life of a new mother who is now taking care of a child along with trying to manage her own health (16,17) . As new medical therapies and treatments become available for individuals with CF, and the life expectancy continues to increase, more and more women with CF will be pursuing pregnancy and having families of their own. It is imperative that healthcare teams understand both the short and long-term effect that pregnancy has on their bodies, as to provide them with the best medical advice and healthcare. 62 Article References 1. Edenborough, Peter, “Pregnancy in Women with Cystic Fibrosis,” Acta Obstet Gynecol Scand. 2002; 81: 689-692. 2. Kent NE, Farquharson DF, “Cystic Fibrosis in Pregnancy,” Canadian Medical Association Journal. 1993;149:809. 3. Dowsett J. “An overview of nutritional issues for the adult with cystic fibrosis” Nutrition. 2000;16;566. 4. Whitty, Janice, “Cystic Fibrosis in Pregnancy,” Clinical Obstetrics and Gynecology. 2010; 53;2;369-376. 5. Cystic Fibrosis Foundation. 2008. Cystic Fibrosis Foundation National CF Patient Registry 2008 Annual Data Report. 2008 The National Cystic Fibrosis Foundation Bethesda, MD. 6. Edenborough F R “Women with Cystic Fibrosis and their potential for reproduction” Thorax. 2001;56:649-655. 7. Olson, Gayle, “Cystic Fibrosis in Pregnancy,” Seminars in Perinatology, 1997;21; 4; 307-312. 8. Edenborough FR, Stableforth DE, Webb et al. “Outcomes in pregnancy in women with cystic fibrosis,” Thorax. 1995;50;170-174. 9. Palmer J, Dillon-Baker C, Tecklin JS, et al. “Pregnancy in patients with cystic fibrosis,” Annals of Internal Medicine. 1983;99:596. 10. Fiel, S.B et al “Pregnancy in Patients with Cystic Fibrosis,” Pediatric Pulmonology. 1997; Supplement 16:111-112. 11. Gilljam, Antoniou, Shin et al. “Pregnancy in Cystic Fibrosis: Fetal and Maternal Outcomes,” Chest. 2000; 118; 85-91. 12. McMullen, Pasta, Frederick et al. “Impact of Pregnancy on Women with Cystic Fibrosis” Chest. 2006;129;706-711. 63 13. Davis, Hofferth “The Assocaition Between Inadequate Gestational Weight Gain and Infant Mortality Among U.S. Infants Born in 2002”. Maternal and Child Health Journal. 2010 Nov 18. 14. Tanser, Hodson, Geddes. “Case reports of death during pregnancy in patients with cystic fibrosis- Three out of four patients were colonized with Burkholderia cepacia.” Respiratory Medicine. 2000;94:1004. 15. McArdle, John “Pregnancy in Cystic Fibrosis” Clinical Chest Medicine. 32 (2011) 111-120. 16. Simcox, Duff, Morton et al “Decision making about reproduction and pregnancy by women with cystic fibrosis,” British Journal of Hospital Medicine. 2009;70;11;639-639643. 17. Connors, Ulles. “The Physical, Psychological, and Social Implications of Caring for the Pregnant Patient and Newborn with Cystic Fibrosis,” The Journal of Perinatal and Neonatal Nursing . 2005: 19;24; 301-315. 64 Appendix A Questions included on Pregnancy Questionnaire: Name: Date of Birth: Date of Baby’s birth: Weight Gained During Pregnancy: Did you need IV antibiotics during pregnancy? Were you hospitalized during your pregnancy? Were you followed by a high risk OB? Infant’s gestational age: Infant’s Birth weight: Did you have any secondary complications? Vaginal delivery or a caesarian section: Did you breastfeed? 65 Appendix B – Data collection Sheet Subject Number__________ VARIABLE Subject Birth date Measurement Date of Measurement birth Collection Method to be used (chart/ questionnaire/ interview) chart only Age at conception Age at delivery chart only chart only Height Weight (last pre-preg) chart only chart only BMI (last pre-preg) chart only Total weight gain during pregnancy Post-pregnancy weight (1st measure 6 mo. post partum) questionnaire Diagnosis of CFRD prior to pregnancy (y/n) chart only Diagnosis of gestational diabetes (y/n) Needed insulin? (y/n) questionnaire chart only % FEV1 pre-preg (all w/in 12 mo. prepreg) Mean pre-preg %FEV1 chart only Will use mean of all available measurements up to 12 mo. prepreg Last %FEV1 measure prior to delivery calculated chart only weeks gestat: 66 First %FEV1 measure post 6 mo. post partum chart only #months post preg: # of hospitalizations during pregnancy questionnaire Need for antibiotic therapy during pregnancy (y/n) VARIABLE questionnaire Measurement Date of Measurement Collection Method (chart/ survey/ interview) Infant Gestational Age At infant birth questionnaire Infant Birth Weight At infant birth questionnaire # of visits with RD during pregnancy chart only Nutrition interventions and topics covered during nutrition counseling: chart only Vaginal Delivery or Caesarian Section Lactation (y/n) If Y, duration questionnaire questionnaire 67 References 1. Edenborough, Peter, “Pregnancy in Women with Cystic Fibrosis,” Acta Obstet Gynecol Scand. 2002; 81: 689-692. 2. Dowsett J. “An overview of nutritional issues for the adult with cystic fibrosis” Nutrition. 2000;16;566. 3. Cystic Fibrosis Foundation. 2008. Cystic Fibrosis Foundation National CF Patient Registry 2008 Annual Data Report. 2008 The National Cystic Fibrosis Foundation Bethesda, MD. 4. Kent NE, Farquharson DF, “Cystic Fibrosis in Pregnancy,” Canadian Medical Association Journal. 1993;149:809. 5. Whitty, Janice, “Cystic Fibrosis in Pregnancy,” Clinical Obstetrics and Gynecology. 2010; 53;2;369-376. 6. Singh, Chouhan, Sidhu. “Maternal Factors for Low Birth Weight Babies.” Medical Journal Armed Forces India. 2009: 65;1; 10-12. 7. Olson, Gayle, “Cystic Fibrosis in Pregnancy,” Seminars in Perinatology, 1997;21; 4; 307-312. 8. Connors, Ulles. “The Physical, Psychological, and Social Implications of Caring for the Pregnant Patient and Newborn with Cystic Fibrosis,” The Journal of Perinatal and Neonatal Nursing . 2005: 19;24; 301-315. 9. Hardin, Dana “The Metabolic Effects of Pregnancy in Cystic Fibrosis,” 2006 Cystic Fibrosis Conference. 10. Edenborough FR, Stableforth DE, Webb et al. “Outcomes in pregnancy in women with cystic fibrosis,” Thorax. 1995;50;170-174. 11. Palmer J, Dillon-Baker C, Tecklin JS, et al. “Pregnancy in patients with cystic fibrosis,” Annals of Internal Medicine. 1983;99:596. 68 12. Fiel, S.B et al “Pregnancy in Patients with Cystic Fibrosis,” Pediatric Pulmonology. 1997; Supplement 16:111-112. 13. Tanser, Hodson, Geddes. “Case reports of death during pregnancy in patients with cystic fibrosis- Three out of four patients were colonized with Burkholderia cepacia.” Respiratory Medicine. 2000;94:1004. 14. Gilljam, Antoniou, Shin et al. “Pregnancy in Cystic Fibrosis: Fetal and Maternal Outcomes,” Chest. 2000; 118; 85-91. 15. Davis, Hofferth “The Assocaition Between Inadequate Gestational Weight Gain and Infant Mortality Among U.S. Infants Born in 2002”. Maternal and Child Health Journal. 2010 Nov 18. 16. Cohen, di Sant’Agnes, Friedlander “Cystic fibrosis and pregnancy. A national survey” Lancet. 1980; 2: 842-844. 17. McMulle, Pasta, Frederick et al. “Impact of Pregnancy on Women with Cystic Fibrosis” Chest. 2006;129;706-711. 18. Taylor, Sarah et al, “Vitamin D Supplementation during Lactation to Support Infant and Mother,” Journal of the American College of Nutrition. 2008; 27; 6;690-701. 19. Hollis, Bruce et al “Assessment of vitamin D requirements during pregnancy and lactation,” American Journal of Clinical Nutrition. 2004;79;717-26. 20. Simcox, Duff, Morton et al “Decision making about reproduction and pregnancy by women with cystic fibrosis,” British Journal of Hospital Medicine. 2009;70;11;639-639643. 21. McArdle, John “Pregnancy in Cystic Fibrosis” Clinical Chest Medicine. 32 (2011) 111-120. 22. Edenborough F R “Women with Cystic Fibrosis and their potential for reproduction” Thorax. 2001;56:649-655. 69