* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Cardiorespiratory arrest
Survey
Document related concepts
Transcript
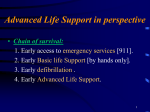
File 15 Cardiorespiratory arrest (adult and child) Cardiorespiratory arrest (adults and child) Recommend Defibrillate in a Ventricular Fibrillation (VF) or pulseless Ventricular Tachycardia (VT) arrest Witnessed arrest - check for pulse & connect patient to monitor - if shockable rhythm, defibrillate Unwitnessed arrest – perform 2 minutes of uninterrupted CPR then assess for shockable or non shockable rhythm Background The aim of management is to restore a normal cardiac output as soon as possible through CPR / defibrillation / airway management / vascular access and drug administration In adults cardiac arrest may occur because of heart attack and/or cardiac arrhythmia. Urgent defibrillation may be lifesaving In children, the majority of cardiorespiratory emergencies are due to either a primary respiratory problem (eg. inhaled foreign body, anaphylaxis) or lack of adequate tissue perfusion (eg. blood loss, severe dehydration). Once cardiorespiratory arrest has occurred, the chances of survival for the child are low. The aim therefore is to recognise and provide appropriate and rapid treatment to the critically ill child to prevent cardiorespiratory arrest Management will be different according to quick accessibility of resuscitation equipment including a defibrillator and drugs, and will either be based on: BLS (Basic Life Support) or ALS (Advanced Life Support) as below Related topics: Basic life support, see DRABC Resuscitation / the collapsed patient, page 35 Acute coronary syndrome, page 79 Cardiac arrhythmias, page 89 Electrocution / electric shock, page 90 1. May present with: Sudden collapse As complication of heart attack As part of clinical picture of most conditions that can be regarded as emergencies 2. Immediate management: See Basic Life Support Flow chart Witnessed arrest - check for pulse & connect monitor and, if shockable rhythm, defibrillate Unwitnessed arrest – 2 minutes uninterrupted CPR then assess for shockable or non shockable rhythm If semiautomatic defibrillator follow instructions If manual defibrillator the most important initial assessment is a division of ECG rhythm into shockable rhythm (VF or VT ) or non -shockable rhythm File 15 Cardiorespiratory arrest (adult and child) Shockable rhythm Ventricular fibrillation Non shockable rhythm Asystole Ventricular tachycardia Pulseless electrical activity (PEA) Sinus rhythm 3. Clinical assessment: As per immediate management Monitor response to defibrillation, medication, improved oxygenation 4. Management: Call MO immediately if on site Shockable rhythms: VF and pulseless VT defibrillation in witnessed arrest o this is best done as three (3) shocks in quick succession with brief assessment of rhythm in between each shock defibrillation in unwitnessed arrest o commence 2 minutes of uninterrupted CPR then o subsequent single defibrillation attempt every 2 minutes (or as best possible) airway and breathing bag and mask (as per basic life support) with high flow oxygen or Laryngeal Mask Airway (LMA) vascular access insert IV cannula drugs Adrenaline child - Adrenaline 0.01 mg/kg IV (RN only) adult - Adrenaline 1 mg IV (RN only) -can be repeated every 3 minutes Amiodarone (on MO order only) adult – Amiodarone 300mg IV bolus - additional dose of 150mg could be considered, followed by an infusion 15mg/kg over 24 hours (MO must order) File 15 Cardiorespiratory arrest (adult and child) Lignocaine adult – Lignocaine IV first dose: 1 mg/kg bolus; second and last dose 0.5 mg/kg (MO must order) It is not recommended to commence Lignocaine infusion until return of spontaneous circulation Magnesium, Potassium maybe ordered by MO Cycles of CPR are 2 minutes before doing a rhythm check and shocking Cessation of resuscitation may not always follow a definite timeframe but will obviously be determined by response to treatment – usually asystole will intervene and generally 20 minutes of asystole after resuscitative efforts would be sufficient for a MO to advise stopping CPR Non-shockable cardiac rhythms: asystole, bradycardiac arrest do not defibrillate airway & breathing o bag and mask (as per basic life support) with high flow oxygen o or Laryngeal Mask Airway (LMA) vascular access o insert IV cannula drugs o Adrenaline child - Adrenaline 0.01 mg/kg IV (RN only) adult – Adrenaline 1 mg adult IV (RN only) can be repeated every 3 minutes if no response o Atropine child – Atropine 0.02 mg/kg IV (RN only) adult – Atropine or up to a total of 3 mg IV(RN only) to completely remove sinus node inhibition (MO must order) Usually 10 minutes in asystole after resuscitative efforts would be sufficient for MO to advise stopping CPR Non-shockable cardiac rhythm: Pulseless Electrical Activity (PEA) Correct reversible causes (4 H’s and 4 T’s) hypoxaemia hypovolaemia hypo / hyperthermia hypo / hyperkalaemia (and other metabolic disorders) tamponade (cardiac) tension pneumothorax toxins / poisons / drugs thrombosis (pulmonary / coronary) File 15 Cardiorespiratory arrest (adult and child) File 15 Cardiorespiratory arrest (adult and child) File 15 Cardiorespiratory arrest (adult and child) Pulseless Electrical Activity (PEA) This describes the presence of a cardiac rhythm on the monitor, but no palpable pulse. In effect, no discernable cardiac output despite the presence of electrical activity in the heart. Also known as Electromechanical Dissociation (EMD) PEA can either occur: in a heart with little functional viable myocardium (ie. dying heart) secondary to reversible medical conditions including the 4 H’s and 4 T’s The history will often guide to the possible causes; if trauma, eg. motor vehicle accident (MVA), hypovolaemia, tension pneumothorax, pericardial tamponade should be considered early if known to be on a calcium antagonist or beta blocker medication, appropriate management needs to be considered early Management in these situations involves working through and correcting the possibilities outlined under non-shockable cardiac rhythm. DO NOT DEFIBRILLATE Airway and breathing o bag and mask (as per basic life support) with high flow oxygen o or Laryngeal Mask Airway (LMA) vascular access o insert IV cannula o give IV fluid bolus of Normal Saline up to 20 mL/kg (adult and child) drugs o child - Adrenaline 0.01 mg/kg IV (RN only) o adult – Adrenaline 1 mg (RN only) o Adrenaline can be repeated every 3 minutes if no response Further management even with an obvious reversible cause will certainly be very difficult. Consult MO and discuss what further intervention is reasonable and feasible File 15 Cardiorespiratory arrest (adult and child) Asystole and PEA Flowchart Consider Hypoxia Hypovolaemia Hyper/ Hypo o electrolyte imbalance o glycaemia Hypothermia Tension pneumothorax Cardiac Tamponade Toxins / Drug overdose Thrombus MI / PE and treat appropriately Bag valve mask ventilate high flow O2 Consider LMA or ETT CPR 30:2 IV / IO access IV or IO Adrenaline 1mg every 3 minutes IV Normal Saline 1 Litre CPR 30:2 2 minutes Symptomatic Bradycardia / Peri-Arrest Situation Inadequate cardiac output in the presence of bradycardia There may be a palpable pulse with each beat, but poor cardiac output associated with slow heart rate do not defibrillate airway and breathing o bag and mask (as per basic life support) with high flow oxygen o or Laryngeal Mask Airway (LMA) vascular access o insert IV cannula In a child with bradycardia – it is almost always a pre-terminal event. Airway, breathing and circulation should always be assessed and treated if needed before pharmacological management of bradycardia is given [1] drugs o child - Atropine 0.02 mg/kg IV (RN only) (MO must order) o adult - Atropine 0.5mg – 0.6mg IV (RN only) (MO must order) o can be repeated every 3 minutes on MO’s orders to a maximum of 3 mg (adult) If still no response, but alive when evacuating/attending MO arrives, will require external cardiac pacing (adult) 5. Follow up: Provide support for family members 6. Referral / Consultation: Always contact MO as soon as circumstances allow in cardiac arrest File 15 Cardiorespiratory arrest (adult and child) 1. Advanced Life Support Group, Advanced Paediatric Life Support - The Practical Approach. 4th ed. 2003: Blackwell Publishing. File 15 Cardiorespiratory arrest (adult and child) The unconscious patient (or patient with altered level of consciousness) Recommend Never leave an unconscious patient alone The Glasgow coma scale or AVPU is a measure of consciousness, always act: on Glasgow coma score less than 14 escalate immediately a drop of 2 or more in Glasgow coma score since the last assessment interval notify MO immediately of a score of 13 or less in a child consider intubation less than 8 Background There are many causes of altered level or loss of consciousness Most clues to the cause will be gained through taking a thorough history from friends or relatives Related topics: DRABC resuscitation / the collapsed patient, page 35 Collapsed patient (adult and child) summary, page 34 Fits / convulsions / seizures, page 63 Cardiac arrest, page 40 Poisoning / overdose, page 182. Bites and stings, page 201 Severe injury / head injury, pages 95, 107 TIA / Stroke, page, page 235 Meningitis, page 524 Hypoglycaemia, page 68 1. May present with: Confused, drowsy, unconscious, not breathing, of unknown cause As part of clinical picture of most conditions that can be regarded as emergencies 2. Immediate management: DRABC resuscitation / the collapsed patient Primary survey Take emergency patient history from relatives / friends, if present A. Assess airway patency (look, listen, feel) Give high flow oxygen-see O2 Delivery systems to maintain O2 saturation >94%. If >94% not maintained, consult MO If possibility of cervical spine injury - maintain cervical spine in line and if available have 2 people apply Stiff neck collar (appropriate to size) B. Assess if breathing effectively Check respiratory rate, effort, O2 saturation C. Insert large bore IV cannula (14 g or 16 g, if possible). Insert the largest you can in the circumstances Check BP, heart rate, capillary refill D. Dysfunction of the central nervous system = conscious state Check Glasgow coma scale or AVPU, pupil size and reaction, BGL, temperature Consult MO as soon as circumstances allow Maintain temperature File 15 Cardiorespiratory arrest (adult and child) 3. 4. Clinical assessment: Obtain a history from friend or relative including circumstances leading to unconscious state. Look for clues which may indicate reason for unconscious state e.g. medications taken E. Expose and examine the patient systematically starting at the head and progressing downwards to the toes. Remove all clothing as you move down, maintaining privacy. Do not let the patient get cold, cover with a blanket after examination. Whilst performing examination look for clinical signs which point to reason for altered level of consciousness or unconsciousness (use diagram to help with systematic approach) Management: Consult MO who will advise further assessment and management depending on clinical circumstances If BGL less than 3 mmol/L see Hypoglycaemia Use diagram to help with systematic approach to possible causes of unconsciousness: poisoning – deliberate or accidental, including alcohol hypoglycaemia, see Hypoglycaemia post-ictal (after fit). See Fit / convulsions / seizures stroke. See TIA / stroke head injury. See Head Injuries subarachnoid haemorrhage respiratory failure acute cardiac arrhythmia / arrest Less common: meningitis or encephalitis. See Meningitis liver or kidney failure septicaemia subdural haematoma hyperglycaemia (high capillary BGL) hypothermia File 15 Cardiorespiratory arrest (adult and child) 5. Follow up: According to possible cause for unconsciousness Patient will need evacuation / hospitalisation in suitably equipped facility 6. Referral / Consultation: Always Contact MO as soon as possible if patient presents with altered level of consciousness or unconscious or this occurs during the course of care act on Glasgow coma score less than 14 escalate immediately a drop of 2 or more in Glasgow coma score since the last assessment interval notify MO immediately of a score of 13 or less in a child remember less than 8 consider intubation File 15 Cardiorespiratory arrest (adult and child) Shock Recommend The aim of management for someone in shock is to replace lost fluid to achieve systolic BP > 100mm Hg and treat cause O2 saturation readings in shock can be unreliable due to peripheral shut down Background Shock is a clinical state in which hypotension occurs due to haemorrhage / cardiac failure or vascular tone and / or inadequate tissue perfusion. The patient in shock looks pale and the body tries to make sure enough blood reaches vital organs such as the brain, heart, and liver by diverting it from e.g. the skin and the kidneys. Many organs can stop working There are different types of shock hypovolaemic shock - due to a large amount of blood or fluid loss from the circulation eg from blood loss, late stages of dehydration in gastroenteritis [9] cardiogenic shock - following heart pump failure after a massive heart attack septic shock – when the body is overwhelmed by infection the vessels dilate and lose tone obstructive shock - occurs with tension pneumothorax, massive pulmonary embolism and pericardial tamponade anaphylactic shock – caused by allergic reaction spinal shock – follows transection of the spinal cord (warm shock) Related topics: DRABC resuscitation / the collapsed patient, page 35 Cardiac arrest, cardiorespiratory arrest, adult / child, pages 40 - 44 Severe injuries, chest injuries, abdominal injuries, spinal injuries, pages 95 - 113 Burns, page 147 Fractures, page 116 Acute wounds, page 131 Nosebleed, page 162 Upper gastrointestinal bleeding, page 171 Anaphylaxis, page 60 Heart attack, page 79 Tubal / ectopic pregnancy, page 406 Gastroenteritis, page 565 1. May present with: Increased heart rate (tachycardia) Increased respiration rate (tachypnoea) – “air hunger” Poor capillary refill Very low or high temperature Low blood pressure (the level will vary) Skin – pale and clammy (cool, moist) – in hypovolaemic shock, capillary return > 2 seconds Warm peripheries (hands and feet) – in septic shock Decreased urine output Anxious, confused, drowsy, unconscious File 15 Cardiorespiratory arrest (adult and child) 2. As part of clinical picture of most conditions that can be regarded as emergencies e.g. Severe Injuries, Burns, Fractures, Acute Wounds, Nosebleed, Upper Gastrointestinal Bleeding, Septicaemia, Heart Attack, Tubal/Ectopic Pregnancy Immediate management: Call for help if available Manage DRABC resuscitation / the collapsed patient Take emergency history from patient, relatives / friends, if present Give high flow oxygen (see O2 Delivery systems) to maintain O2 saturation >94%. If >94% not maintained consult MO In case of fracture or bleeding wound, stop any external bleeding by direct pressure and pressure bandaging Check and monitor BP and heart rate, respirations, O 2 saturation, BGL, temperature Check and monitor conscious state - Glasgow coma scale or AVPU Insert large bore IV cannula (14 g or 16 g, if possible). See diagram for veins most easily found and cannulated. Insert the largest IV cannula you can in the circumstances, which may not be very big, as the patient is often shut down with veins hard to find. If intravenous access is unable to be established or is likely to be difficult and time consuming, intraosseous infusion provides a route for the administration of parenteral fluids and drugs in life threatening situations. This technique is applicable to both adults and children. See Intraosseous infusion If unable to access IV or intraosseous route consult MO immediately For all causes of shock except for cardiogenic shock it is usual to start with IV Normal Saline or Hartmann’s. MO will advise quantities and rate. The aim is to keep: Adults Heart Rate <120/min Systolic BP >90 - 100 mm Hg Urine Output >0.5 ml/kg/hr Children compensate very well in the early stages of shock, but can decompensate rapidly Consult MO as soon as possible 3. Clinical assessment: Obtain patient history including circumstances that may suggest the cause of shock Perform standard clinical observations with particular attention on BP, urine output, temperature, Glasgow coma scale or AVPU, capillary refill 4. Management: Consult MO as soon as possible, who will organise evacuation / hospitalisation Monitor clinical status and response to intervention - BP and heart rate, respirations, O2 saturation, BGL, temperature, Glasgow coma scale or AVPU If injured and shocked and not obvious where blood has been lost, suspect internal bleeding: chest (haemothorax), see Chest injuries abdomen (ruptured spleen/liver/kidneys, fractured pelvis) see Abdominal injuries fractured humerus (forearm) or femur (thigh), pelvis, see Fractures File 15 Cardiorespiratory arrest (adult and child) Manage in consultation with MO as per: severe injuries, chest injuries, abdominal injuries, spinal injuries burns fractures, acute wounds nosebleed, upper gastrointestinal bleeding anaphylaxis heart attack tubal / ectopic pregnancy acute gastroenteritis 5. Follow up: According to possible cause for shock Patient will need evacuation / hospitalisation in suitable equipped facility 6. Referral / consultation: Consult MO on all occasions of shock File 15 Cardiorespiratory arrest (adult and child) File 15 Cardiorespiratory arrest (adult and child) File 15 Cardiorespiratory arrest (adult and child)