* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Chapter 11—Blood. I. Functions of Blood. a. Transportation of: i
Blood transfusion wikipedia , lookup
Jehovah's Witnesses and blood transfusions wikipedia , lookup
Hemolytic-uremic syndrome wikipedia , lookup
Blood donation wikipedia , lookup
Autotransfusion wikipedia , lookup
Men who have sex with men blood donor controversy wikipedia , lookup
Hemorheology wikipedia , lookup
Plateletpheresis wikipedia , lookup
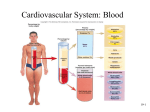
Chapter 11—Blood. I. II. Functions of Blood. a. Transportation of: i. Gasses—oxygen, carbon dioxide, carbon monoxide, nitrogen, etc. ii. Formed elements (blood cells). iii. Ions of calcium, phosphorus, potassium, sodium, chlorine, etc. iv. Complex organic molecules—hormones, proteins, lipoproteins, glucose, glycoproteins, antibodies, etc. b. Protection, in the form of: i. White blood cells and antibodies, which function in immunity. ii. Clotting reactions that seal breaks in blood vessels. iii. Buffers in the blood that help maintain acid-base balance. iv. Regulation of body temperature. Composition of Blood—a fluid CT composed of plasma (a liquid CT matrix), red blood cells (RBCs), white blood cells (WBCs), and platelets (thrombocytes). The average adult has 4-5 L of blood (6-8% of body weight). A drop of blood has ~250 million blood cells in it. Figure 11.1. a. Plasma. i. Makes up about 55% of whole blood. ii. Serves as the transport medium for the blood cells, platelets, ions, gasses, wastes, plasma proteins, etc. 1. Plasma proteins (7-8% of plasma) help keep water in the plasma from moving into body cells; because the interior of cells contain many proteins, water would enter cells via osmosis if the plasma proteins were not present. a. Albumins are the most important plasma proteins in regulating water balance in the plasma. b. Globins are a diverse group of plasma proteins; some transport lipids, or fat-soluble vitamins. Others are antibodies. c. Clotting proteins, like fibrinogen, seal breaks in blood vessels. b. Formed elements—red blood cells, white blood cells, and platelets. Production of these cells begins in the red bone marrow from blood stem cells. Figure 11.2. Makes up about 45% of whole blood. Table 11.1 provided a summary of the formed elements. i. Platelets (thrombocytes)—derived from cells called megakaryocytes that then fragment to become the platelets. 1. About 200 billion platelets form every day; they mature in a week, and circulate in the blood for 5-10 days. 2. Cause blood clotting to occur (hemostasis). ii. White blood cells (leukocytes)—make up less than 1% of whole blood. Figure 11.3. 1. Scavenge tissue debris. 2. Function in immunity to destroy invading bacteria and other pathogens. 3. Circulate in the blood, but most migrate out of the vessels and enter the tissues. 4. There are five types of WBC’s in two groups: a. Granulocytes have large granules in their cytoplasm. (The granules include lysosomes and structures that contain hydrolytic enzymes). i. Neutrophils—find and destroy damaged tissue and invading microorganisms via phagocytosis. First type of WBC to arrive at a site of infection. Die after engulfing about a dozen bacteria, but release chemicals that attract other neutrophils as they die. ii. Eosinophils—take part in allergic reactions and attacks on parasitic worms. Lessen the severity of allergic reactions by engulfing antigen-antibody complexes via phagocytosis and inactivating inflammatory chemicals. iii. Basophils—take part in inflammation and allergic reactions by releasing histamine, which attracts other white blood cells and causes vasodilation, to increase blood flow. b. Agranulocytes do not have large granules in their cytoplasm. i. Monocytes—differentiate into macrophages that migrate through body tissues and engulf microbes & cellular debris. ii. Lymphocytes—participate in specific immune responses. 1. B lymphocytes give rise to plasma cells, which produce antibodies. a. A specific antibody will attach to a specific antigen to help limit the spread of a pathogen/foreign cell. 2. T lymphocytes destroy foreign cells and tissues. 3. Natural killer cells detect and destroy abnormal tissue cells. iii. Red blood cells (erythrocytes)—make up about 45% of whole blood. Figure 11.4. 1. Bi-concave disk; maximizes surface area to volume. No nucleus, very few organelles. 2. Extremely flexible; can squeeze through capillaries smaller than itself. 3. Transports oxygen, which binds to the protein hemoglobin (iron, red). Figure 11.5. a. Each RBC contains ~280 million hemoglobin molecules. b. Hemoglobin gives blood its red color. c. Each hemoglobin molecule consists of four polypeptide chains, each of which contains a heme group. The iron within the heme binds to a molecule of oxygen (O2). i. Molecular oxygen + hemoglobin = oxyhemoglobin. ii. Hemoglobin’s ability to bind oxygen depends on: 1. Relative concentrations of oxygen and CO2. 2. Ph (~neutral). 3. Temperature (cooler is better). iii. Hemoglobin transports H+ to help control pH of body fluids. iv. When oxygen binds to the heme group, it is bright red in color; hemoglobin depleted of oxygen has a bluer color. d. Carbon monoxide binds 200 times more readily to hemoglobin than oxygen does; carbon monoxide poisoning can result… 4. RBCs transport ~23% of blood’s total carbon dioxide load, which binds to hemoglobin at a different location compared to where oxygen binds. The rest of the carbon dioxide is transported by the plasma. III. Life cycle of RBCs. a. RBC’s are derived from stem (progenitor) cells in the red bone marrow. b. As the RBC matures, it loses its nucleus, ribosomes, and other structures. c. Production of a new RBC takes about 6 days. d. Mature RBCs do not divide or synthesize new proteins, but do contain enzymes and other proteins. e. RBCs function for about 120 days. f. As RBCs die, macrophages destroy them, with many components (amino acids and iron) being recycled by the body. Leftovers that aren’t recycled (portions of heme groups) are converted to bilirubin (a pigment) which is picked up by the liver, and mixed with bile. i. Bilirubin broken down by intestinal bacteria is partly responsible for the color of feces. ii. A bruise forms when capillaries rupture, releasing RBCs into the tissue; as they become depleted of oxygen, a black-and-blue bruise forms; as they break down, heme gives the bruise a yellowish color. IV. V. g. Erythropoietin (a hormone produced by the kidneys) can stimulate stem cells to produce RBCs. Figure. 11.6. i. Normally the production of RBCs matches that of their destruction. ii. If the kidneys detect a reduction in the amount of oxygen reaching them, they release erythropoietin into the blood. iii. Erythropoietin stimulates stem cells in the red bone marrow to produce more RBCs. 1. Production can increase up to 10 times normal; this equates to about 20 million new red blood cells being formed every second. iv. As the additional RBCs enter circulation, more oxygen makes it to the kidneys, causing a decrease in the secretion of erythropoietin. v. This process represents a homeostatic mechanism regulated by negative feedback. Blood Cell Disorders. You will not be tested on this material. Blood Types. a. The surfaces of all cells (including those in your body) are covered by proteins called antigens that identify them. i. Your immune system recognizes your cell’s antigens as belonging there; these are sometimes referred to as “self” cells. b. Immune system proteins called antibodies can tell the difference between self and non-self cells based on the surface proteins (antigens) of the cells. c. Any non-self cell is attacked by the antibodies in an attempt to destroy it. d. Human blood types can be differentiated by the antigens present on the surface of RBCs. e. Human RBCs have antigens that are designated as A, B, or O. (Genetically determined). f. If incompatible blood types are mixed, a severe immune response occurs (agglutination = clotting). Figure 11.7. g. See the table I have included below and Table 11.2 in your textbook. Red blood cell antigens and plasma antibodies by blood type. Blood Type Surface Proteins Antibodies Present (In Plasma) (Antigens) Present A A Anti-B antibodies (can receive type A or O blood) B B Anti-A antibodies (can receive type B or O blood) AB A and B None (this person is a “universal recipient”) O None Anti-A and Anti-B antibodies (this person is a “universal donor” but can only receive type O blood) h. i. j. k. RBCs may or may not have an Rh protein (antigen) on their surfaces. If you are Rh+, you have this antigen, and if you are Rh-, you don’t have this antigen. Normally, people don’t have antibodies to Rh antigens. If an Rh- person receives blood from an Rh+ person, the Rh- person becomes sensitized to the Rh antigen and begins to produce Anti-Rh antibodies. l. On subsequent exposure to Rh+ blood, agglutination will occur. m. Hemolytic disease of the newborn can occur when a mother is Rh- and the fetus is Rh+. Figure 11.8. i. Maternal and fetal blood do not normally mix, but during birth or if a miscarriage occurs, the two blood supplies can come into contact with each other. ii. This can cause the mother to produce anti-Rh antibodies. iii. If a second pregnancy with an Rh+ fetus occurs, anti-Rh antibodies from the maternal bloodstream will cross the placenta and attach the RBCs of the fetus. Death or severe anemia in the child can result. iv. To prevent this from happening, RhoGAM, a serum with antibodies against the Rh antigen, is injected into the mother during the 7th month of pregnancy and shortly after VI. delivery if the child is Rh+. This prevents the mother’s immune system from producing anti-Rh antibodies. Blood Clotting (Hemostasis). a. Hemostasis—mechanisms through which damage to a small blood vessel is repaired, and associated bleeding is stopped. Figure 11.9. i. When a vessel is damaged, smooth muscle in the vessel wall spasms and constricts the vessel (vasoconstriction), reducing blood flow through it or stopping it. ii. Platelets clump together, attaching to exposed collagen fibers of the damaged vessel, to form a temporary plug. iii. Platelets already present release chemicals that prolong the spasm, attract more platelets, and causes them to stick together even more. 1. Aspirin prevents the manufacture of this chemical… iv. Plasma proteins become activated, that through a series or reactions, causes a network of insoluble threads of fibrin to form around the damaged area. 1. When a tissue is injured, it releases “clotting factors”. 2. Clotting factors convert an inactive blood protein to prothrombinase, which is an enzyme. 3. Prothrombinase converts prothrombin to thrombin. 4. Thrombin acts on the plasma protein fibrinogen, to form fibrin. v. This net of fibrin traps RBCs and platelets, which forms a clot. vi. The clot shrinks with time, sealing the breach in the vessel. 1. When the wound is healed, the enzyme plasmin dissolves the clot by breaking down the fibrin. b. Hemophilia—an inherited genetic disorder that involves mutation of genes responsible for the production of clotting factors. c. Thrombus—clot lodges in an unbroken blood vessel. d. Embolus—clot that drifts through the circulatory system. Study suggestions for this chapter: In the textbook at the end of the chapter, the sections entitled 1) Highlighting the Concepts, 2) Recognizing Key Terms, and 3) Reviewing the Concepts are all good for you to gauge your comprehension and focus your study efforts.