* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download This Item - Kettering General Hospital
Survey
Document related concepts
Transcript
Affiliated Teaching Hospital Index No: MM0000 MEDICINES CODE Version: 1 Date ratified: 14 September 2016 Ratified by: (Name of Committee) Name of originator/author, job title and department: Medicines Management Committee Director Lead (Trust-wide policies) Associate Medical Director (local Policies) Clinical Management Team / Directorate Applicable to Name of responsible committee for the policy: Date issued for publication: Duane McLean Chief Pharmacist and Accountable Officer for Controlled Drugs Medical Director Trustwide Medicines Management Committee September 2016 Review date: June 2019 Expiry date: (Date 3 months following review date) Equality impact assessed by: (name, job title and department) Date impact assessed: September 2019 CQC Fundamental Standards Regulation 12: Safe Care and Treatment MM0000 Medicines Code v1 Page 1 of 113 Duane McLean, Chief Pharmacist August 2016 Chairman: Graham Foster JP 1 Chief Executive: David Sissling CONTRIBUTION LIST Individuals involved in developing the document Name Duane McLean Karen Favell Sue Hussain Designation Chief Pharmacist Deputy Chief Pharmacist - Clinical Excellence Deputy Chief Pharmacist - QIPP Circulated to the following individuals for consultation Name Dhiren Bharkhada Karen Moody Naomi Fleming Anthony Bartlett Anusha Patel Scott Hillery Janice Wright Robin Lee Beverley Bone Eilish Crowson Designation Pharmacist Advanced Cancer Services Pharmacist Team Manager Medicine Pharmacist Advanced Micro and Infectious Diseases Pharmacist Advanced Informatics/Medicines Information Pharmacist Advanced Pharmacist Technician Team Manager Production Technician Team Manager Dispensary and Stores Consultant ENT Surgeon and Chair of MMC Acute Pain Service Matron Head of Midwifery and Business Unit Director, Women & Children Marie Sharpe Lead Nurse – Practice Development Diane Postle Deputy Director of Nursing Senior Nurse representatives via Matrons’ Forum Consultant members of the Medicines Management Committee, New Medicines Group and Medication Safety Group MM0000 Medicines Code Page 2 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling MM0000 Index No. Approval and Authorisation Completion of the following signature blocks signifies the review and approval of this process. Name Job Title Mr Robin Lee Chair of MMC Signature Date 14 September 2016 Local Committee approval (where applicable) Name of Committee Name of Chairperson Date of Approval Medicines Management Mr Robin Lee 14 September 2016 Change History Version Date Author Reason 1 September 2016 Duane McLean Amalgamation of several Trust policies into one overarching Medicines Code* *Trust policies superseded by the introduction of Medicines Code: MM5 Patient Self-Administration of Medicines Policy MM11 Policy for Use of Unlicensed and ‘Off Label’ Medicines for Adults and Children MM14 Medicines Reconciliation Policy for Adults MM16 Intravenous Medication Preparation and Administration MM19 Prescribing Medicines Policy MM28 Controlled Drugs Policy MM29 Secure management of FP10s in clinics, wards and departments MM32 Procedure for the Disposal of Medicines in Clinical Areas MM36 The Security and Storage of Medicines in Clinical Areas MM49 Preparation and Administration of Medicines in Clinical Areas MM50 Procedures for the Development, Authorisation, Use and Review of Patient Group Directions MM0000 Medicines Code Page 3 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling Impact Assessment Undertaken by Date Duane McLean, Chief Pharmacist August 2016 A translation service is available for this policy. The Interpretation/Translation Policy, Guidance for Staff (I55) is located on the library intranet under Trust wide policies. MM0000 Medicines Code Page 4 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling CONTENTS PAGE 1. INTRODUCTION 9 2. SCOPE 10 3. AIM 10 4. RESPONSIBILITIES 11 5. DEFINITIONS 12 6. DOCUMENT CONTENT - MEDICINES CODE 1. ORDERING AND RECEIPT OF MEDICINES 18 1.1 Key principles 1.2 Responsibilities 1.3 Risk assessment 1.4 Components of safety 1.5 Ordering of medicines 1.6 Unlicensed medicines 1.7 Home delivered medicines 1.8 Receipt of medicines into Pharmacy 1.9 Receipt of unlicensed medicines into Pharmacy 1.10 Receipt of home delivered medicines 1.11 Receipt of medicines into clinical areas from Pharmacy 2. STORAGE AND SECURITY OF MEDICINES 23 2.1 Key principles 2.2 Responsibilities 2.3 Medicines keys 2.4 Storage locations 2.5 Fluid warmers 2.6 Temperature monitoring 2.7 Refrigerated storage 2.8 Stock maintenance 2.9 Return of medicines 2.10 Disposal of medicines 2.11 Ward and department closures MM0000 Medicines Code Page 5 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 2.12 Audit, assurance and accountability 3. MEDICINES RECONCILIATION 34 3.1 Medicines reconciliation checklist 3.2 Medicines reconciliation process 4. PRESCRIBING 37 4.1 Who can prescribe 4.2 General principles of prescribing 4.3 Range of medicines to prescribe 4.4 Verbal orders 4.5 Inpatient prescribing 4.6 Allergies or sensitivities 4.7 Prescribing for all medicines 4.8 Prescribing for intravenous medicines 5. PREPARATION OF MEDICINES 49 5.1 Responsibilities 5.2 Key principles 5.3 General principles 5.4 Ward preparation 5.5 Use of oral syringes 5.6 Insulin syringes 6. CHECKING OF MEDICINES 55 6.1 Key principles 6.2 General procedures 6.3 Prescription validation and optimisation 7. ADMINISTRATION OF MEDICINES 59 7.1 Key principles 7.2 When administering medicines steps to follow 7.3 Patients’ own medicines 7.4 Delay or omission of medicines 7.5 Omission codes 8. SELF-ADMINISTRATION OF MEDICINES 67 8.1 Who can self-administer 8.2 Assessment of patients MM0000 Medicines Code Page 6 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 9. SUPPLY OF MEDICINES TO PATIENTS 70 9.1 Key principles 9.2 Key standards 9.3 General procedures 10. DISPOSAL OF PHARMACEUTICAL WASTE 71 10.1 Key principles 10.2 General procedures 11. PATIENT GROUP DIRECTIONS 74 11.1 Key principles 11.2 Development, authorisation and review 11.3 Using a PGD 12. CONTROLLED DRUGS 77 12.1 Key principles 12.2 Key standards 12.3 Accountability for CDs 12.4 Ordering of CDs 12.5 Receipt of CDs 12.6 Obtaining CDs out-of-hours 12.7 Transport of CDs 12.8 Transfer of CDs 12.9 Storage and security of CDs 12.10 Storage and security of TTAs including CDs 12.11 Loss of CD cupboard keys/replacement lock 12.12 Patients’ own CDs 12.13 Prescribing of CDs 12.14 Preparation and administration of CDs 12.15 CDs issued directly to medical staff 12.16 Documentation and record keeping for CDs 12.17 Disposal or return of CDs 12.18 Stock checks of CDs 12.19 Abusable medicines 12.20 Illicit substances 12.21 CD stationery MM0000 Medicines Code Page 7 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 13. UNLICENSED AND OFF LABEL MEDICINES 104 13.1 When can unlicensed medicines to used 13.2 Unlicensed prescribing for children 13.3 Prescribing in Critical Care 13.4 Prescribing in Haematology or Oncology 13.5 Prescribers 14. FP10 PRESCRIPTION FORMS 108 14.1 Key principles 14.2 Ordering FP10 prescription forms from Pharmacy 14.3 Returning FP10 forms 14.4 Secure storage and safekeeping of FP10 prescription forms when not in use 14.5 Secure management of FP10 prescription forms ‘in-use’ 14.6 Unused and/or ‘spoilt’ FP10 prescription forms 14.7 Procedure for missing or unaccounted-for FP10 prescription forms 14.8 Prescribing on FP10 prescription pads 14.9 Monitoring, compliance and effectiveness 7. TRAINING 15 8. MONITORING COMPLIANCE AND EFFECTIVENESS 16 9. PROCESS FOR IMPLEMENTATION AND DISSEMINATION 16 10. DOCUMENT REVIEWS AND UPDATES 16 11. REFERENCES 16 12. EQUALITY IMPACT ASSESSMENT 16 13. APPENDICES 16 MM0000 Medicines Code Page 8 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 1.0 INTRODUCTION Medicines management encompasses a range of activities intended to improve the way that medicines are selected, procured, prescribed, dispensed, and administered. The Royal Pharmaceutical Society Professional Standards for Hospital Pharmacy Services requires hospitals to have a policy, procedures and guidelines to ensure the safe use of medicines across the organisation. It is a requirement for Registration by the Care Quality Commission (CQC) that registered staff protect patients against the risks associated with unsafe use of medicines. Appropriate arrangements should be in place for obtaining, recording, handling, using, safe keeping, safe administration and disposal of medicines used for regulated activity. This policy lays out the key principles for the control of medicines to be followed at every stage of the medicines use process (procurement, storage, prescribing, preparation, dispensing, administration and disposal). Finally it includes the roles of the medicines management committees including the Northamptonshire Prescribing Advisory Group. Clinical Business Units may then develop local policies within this framework in consultation with the Medicines Management Groups for Kettering General Hospital (KGH). The local policy should be approved by the Medicines Management Committee, Associate Medical Director and Head of Nursing or other suitable group. KGH NHS Foundation Trust endeavours to reflect the needs and preferences of patients, their families and their carers. Patients, with their families and carers, where appropriate, will be involved in and consulted on all decisions about their care and treatment. KGH NHS Foundation Trust also commits to: MM0000 Medicines Code Page 9 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling Make decisions in a clear and transparent way, so that patients and the public can understand how services are planned and delivered. Make the transition as smooth as possible when patients are referred between services, and to include patients in relevant discussions. Patients have the right to medicines and treatments that have been recommended by the National Institute for Clinical Excellence for use in the NHS, provided that the prescriber considers that they are clinically appropriate, and the patient meets the criteria specified. Patients have the right to be involved in discussions and decisions about their healthcare and to be given information to enable them to do this. 2.0 SCOPE This document applies to all areas of the Trust where medicines are used and to all employees involved in the medicines use process. Employees include those who are employed through external agencies, students, locums and bank staff. 3.0 AIM Medicines are the most frequent therapeutic intervention made within the NHS with potential for error at every stage of the medicines use process. Errors in medicines management expose patients to unnecessary risk and harm, poor patient experience, unnecessary expenditure and loss of reputation. The aim of this policy and procedures is to define safe, high quality processes for medicines use. Through following these processes and learning from mistakes, patient safety will be improved. The Medicines Code is presented as a series of chapters covering all aspects of the medicines use process and applies to all medical, nursing, pharmacy and allied health professions involved in medicines management activities. It applies to all staff employed by the Kettering General Hospital NHS Foundation Trust and those contracted to work on a sessional basis. MM0000 Medicines Code Page 10 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 4.0 RESPONSIBILITIES Integrated Governance Committee is responsible for assuring the Trust Board that policy and procedures meet statutory and best practice requirements, to safeguard patient care. Quality Governance Steering Group is responsible for ensuring prescribing and medicines management are evidence-based and relevant policy and procedures are consistently applied across the organisation to deliver high standards of care. Any risks identified, which cannot be mitigated will be owned by this committee and documented on the Risk Register. Medicines Management Committee is responsible for the safe, clinical and costeffective use of medicines in the Trust. This multi-disciplinary committee promotes evidence based prescribing, is responsible for development and audit of policy and procedures for the safe use of medicines. New Medicines Group this multi-disciplinary committee promotes evidence based prescribing, reviews requests for new medicines and manages the hospital and joint area prescribing formularies. Medication Safety Group this multi-disciplinary committee reviews medication incidents and develops action plans to improve medicines use within the Trust. Clinical Business Units have responsibility in managing performance related to all aspects of medicines use within their areas. The Medical Director and Director of Nursing have overall responsibility for ensuring adherence to this policy and procedures. The Chief Pharmacist is accountable for ensuring the requisite processes are in place and for monitoring overall compliance with this policy. MM0000 Medicines Code Page 11 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling The Chief Pharmacist is accountable to the Department of Health, with the Chief Executive, Medical Director and Director of Nursing and Midwifery for the safe, appropriate and effective use of medicines within the Trust. The Chief Pharmacist provides specialist expertise and, delegated from the Chief Executive, has corporate responsibility across the Trust for all aspects of medicines management including associated controls assurance standards and other DoH and SHA performance management arrangements that are applicable. Heads of Nursing are responsible for medicines practice in within their area Matrons are accountable for ensuring that the systems associated with medicines management are followed and that the security of medicines on the ward is maintained. Clinicians and Practitioners All clinicians and practitioners (of all health professions) are responsible for following these legislative and best practice standards for medicines use in order to deliver safe and effective patient care. 5.0 DEFINITIONS 5.1 Staff Definitions Accountable Officer Officer in a health care organisation who is responsible for the safe management of controlled drugs, as required by Controlled Drugs (Supervision and Management of Use) Regulations 2006. Appointed Practitioner The senior registered practitioner with overall responsibility for the safe and secure handling of medicines for a ward or department e.g. Lead Nurse, Theatre Manager or their deputy. Assigned Practitioner A healthcare practitioner assigned to a particular task. Assistant Practitioner A non-registered healthcare practitioner with specific extended roles and competencies MM0000 Medicines Code Page 12 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling Designated Practitioner The senior registered practitioner in charge of a ward or department at a particular time/shift. Medical Practitioner Any doctor registered to practice in the UK as an independent medical prescriber. Non-Medical Prescriber A registered non-medical practitioner who has completed the necessary training and registration to prescribe medicines: Supplementary A member of an approved healthcare profession who can prescribe medicines for a named patient as part of a written clinical management plan, agreed with the patient and an independent medical prescriber. Independent A nurse or pharmacist who has undertaken formal non-medical prescribing training and assessment and is registered as a prescriber with their professional body. Physicians Associate Registered practitioner Physician associates are dependent practitioners with a generalist medical education, who work alongside doctors.. A state regulated and registered practitioner who is listed on a professional practice register. This does NOT include voluntary registration. Responsible Pharmacist The lead pharmacist for a Clinical Business Unit or Department, or their deputy, who is responsible for the safe preparation and supply of a pharmaceutical product. Responsible Officer The person accountable for medication homecare for Homecare services. 5.2 Process Definitions Administer To introduce a medicine into a patient by means of enteral (oral) or parenteral (injection) route or by external application. Controlled Drug (CD) The drugs listed in schedules 1-5 of the Misuse of Drugs Regulations 2001 (as amended, which are subject to varying controls on prescribing, storage, handling and disposal). MM0000 Medicines Code Page 13 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling Dispense To make up or supply a medicine for a patient (usually a prescription only medicine) together will all the necessary technical, clinical and professional checks. Medicines are dispensed under the supervision of a pharmacist. Homecare Medicines Homecare medicine delivery service can be described as being a service that delivers ongoing medicine supplies and, where necessary, associated care, initiated by the hospital prescriber, direct to the patient’s home with their consent. Licensed Medicine A medicine that has been granted a marketing authorisation (MA) (previously known as a product licence PL), and can be ‘placed on the market’ in the UK for the treatment of medical conditions as defined in its MA or PL (i.e. its licensed indications). Medicine Any substance or combination of substances administered to human beings for the purpose of investigating or treating disease. Medicines Code Kettering General Hospital Policy and Procedures for medicines Medicines Management A broad term describing activities that promote the safe, clinical and cost-effective use of medicines. Medicines use process The process of procuring, storing, prescribing, dispensing, preparing and administering medicines and disposing of pharmaceutical waste. Medicines Reconciliation The process of identifying an accurate list of a person's current medicines and comparing them with the current list in use, recognising any discrepancies, and documenting any changes Off Label Use Use of a medicine for a clinical indication or in a way that is not covered by the licence. Patient Group Direction Specific written instruction for supply & administration of a named medicine in a defined clinical situation signed by a doctor or MM0000 Medicines Code Page 14 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling dentist and authorised by an appropriate healthcare body. Pharmacy Validation The clinical pharmacy process of reviewing a prescribed medicine for clinical appropriateness in terms of drug, dose and frequency as well as for prescription clarity, completeness and safety. Prescribe To authorise in writing the supply of a medicine. Prescription only medicines (POM) can only be prescribed by a registered medical or non-medical prescriber. Prescription A written authorisation to supply or administer a medicine. POM A medicine included in the Prescription Only Medicines (Human Use) Order 1997 of the Medicines Act. Registered A health professional who is part of state regulated profession and named on the designated register. Supply To provide a medicine to a patient or carer for the purpose of administration or selfadministration. Unlicensed Medicine A medicine is one that does not have a MA and therefore does not have a licence for use in the UK. This may be because the product is awaiting the granting of a licence in the UK, or it is undergoing clinical trials, or is only manufactured for export or has been withdrawn from the UK market. 6.0 DOCUMENT CONTENT - see from p18 to end 7.0 TRAINING All clinical staff will have medicines management training at induction. Assessments of competence to prepare and administer medications are required. MM0000 Medicines Code Page 15 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 8.0 MONITORING COMPLIANCE AND EFFECTIVENESS Audit Schedule: Prescribing standards (3 per year) Controlled drugs storage (quarterly) Medicines security (quarterly) Patient Group Directions (annually) Unlicensed medicines (annually) Medicines Safety Thermometer (monthly) 9.0 PROCESS FOR IMPLEMENTATION AND DISSEMINATION Dissemination and implementation will be through the Quality Governance Steering Group and Medicines Management representatives, Lead Nursing structure, Matrons Forum, CBU governance structures and ward meetings. Further communications will be issued through the Leadership Brief and Pharmacy Matters publication. 10.0 DOCUMENT REVIEWS AND UPDATES This document will be reviewed every three years at a minimum. 11.0 REFERENCES Royal Pharmaceutical Society of Great Britain, “The Safe and Secure Handling of Medicines: A Team Approach,” Royal Pharmaceutical Society of Great Britain, 2005. 12.0 EQUALITY IMPACT ASSESSMENT The Trust takes its obligations under Equality Legislation very seriously and aims to provide fair and equitable treatment to, and value diversity in, its staff, patients and visitors. In doing so it aims to ensure that its actions and working practices comply with both the spirit and intention of the Human Rights Act (1998) and the Equality Act (2010) which relates to the protected characteristics of age, disability, gender reassignment, marriage & civil partnerships, pregnancy & maternity, race, religion or belief, sex and sexual orientation. The Trust will also carry out its functions in a manner that reduce the inequalities of outcome, which may result from socioeconomic disadvantage. 13.0 APPENDICES 1. 2. 3. Prescribing Audit Tool Self Administration of Medicines Assessment Tool Self Administration of Medicines Consent Form MM0000 Medicines Code Page 16 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. Patient Group Directions (PGD) Proposal Patient Group Directions (PGD) Proposal Form Patient Group Directions (PGD) Development and Submission Patient Group Directions (PGD) Pre-Approval Form Controlled drug cupboard lock/key replacement Controlled drug TTA prescription Controlled drug returns/destruction Sample Ward CD Record Book Sample Theatre CD Record Book Request to use an unlicensed or off-label medicine 'Special' medicines patient information leaflet‘ KGH FP10 Prescription Order Form http://www.nhsbsa.nhs.uk/Documents/SecurityManagement/Security_of_pre scription_forms_guidance_Updated_August_2013.pdf MM0000 Medicines Code Page 17 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 1. ORDERING AND RECEIPT OF MEDICINES Medicines must be procured to ensure that the right medicine is available in the right quantity and quality, at the right time for the right patient. In order to achieve this, medicines must be ordered and received through the Pharmacy Department. 1.1. Key Principles 1.1.1. The use of all medicines carries the risk of a patient safety incident (such as inappropriate reconstitution or administration) as well as the more usually considered adverse events such as side effects. 1.1.2. These risks can and should be minimised. To enable this it is essential that all risks are identified and assessed and action taken to minimise the possibility of a patient safety incident. 1.1.3. Part of this process is to ensure that the procurement of medicines provides so far as is possible medicines which are of suitable quality, and are safe in use i.e. prescribing, dispensing, preparation, administration and disposal. Moreover it is essential that the procurement process assesses the capabilities of the upstream supply chain to ensure products are genuine, stored correctly and available when required. 1.1.4. Licensed medicines should be used in preference to unlicensed medication, however there maybe circumstances where the licensed product is deemed to present a significant clinical risk and it may be safer to use and unlicensed product or formulations. 1.2. Responsibilities 1.2.1. The Trust Chief Pharmacist has the delegated responsibility for the procurement of medicines. 1.2.2. Authority to procure certain specific products may be delegated elsewhere (e.g. medical gases, which may be purchased by Estates/Facilities). MM0000 Medicines Code Page 18 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 1.3. Risk Assessment 1.3.1. Where new medicines, presentations of formulations of medicines are added to the Trust medicines formulary, a risk assessment should be undertaken by staff with a full understanding of the purpose and end use of the product being procured. 1.3.2. Risks should be identified and minimised, reporting systems should be available and acted upon, and if normal sources are not available (e.g. in a shortage situation) then alternatives need to be assessed in the light of the increased risk they may present to patients. 1.3.3. If a product is assessed locally as a high risk of causing a patient safety incident this should be reported to regional Quality Assurance (QA) and procurement specialists. These lists can then form the basis of discussion with the manufacturers about possible changes in presentation. 1.4. Components of Safety 1.4.1. Risk assessment should take account of the following factors. 1.4.1.1. Quality of Products. 1.4.1.2. Design and Use of Products (e.g. ready-to-use and ready-toadminister products). 1.5. 1.4.1.3. Labelling and Packaging of Products. 1.4.1.4. Source of Products and Materials. 1.4.1.5. Treatment of Product within Supply Chain. Ordering of medicines 1.5.1. Ordering of medicines is carried out by the Pharmacy Purchasing Office (during office hours). 1.5.2. Orders for medicines should be transmitted to suppliers electronically to reduce the risk of errors. 1.5.3. Out of hours, in cases of emergency, where a medicine is required that is not available in the Pharmacy Department, the MM0000 Medicines Code Page 19 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling oncall pharmacist may order the medicine from a wholesaler or another hospital or other usual supplier. In this case, the order will be placed by telephone and the details passed to the Pharmacy Purchasing Office on the next working day. 1.6. Unlicensed Medicines 1.6.1. Unlicensed medicines should be procured in accordance with the Unlicensed Medicines Policy. 1.6.2. The Pharmacy Department is responsible for the specification of an unlicensed medicine, and with ensuring that the product supplied meets the specification and is of acceptable quality. 1.7. Home Delivered Medicines 1.7.1. All supplies of home delivered medicines should be ordered in conjunction with the Pharmacy Department. 1.7.2. The prescription for a home delivered medicine constitutes an order. 1.7.3. All homecare prescriptions require a professional check by a registered member of the pharmacy team, initial prescriptions or where doses and frequency have been amended should, whenever possible be professionally checked by a pharmacist. 1.7.3.1. Where the prescription is a continuation of a previously commenced therapy and which remains unchanged for dose, frequency and duration a competent registered pharmacy technician may provide the clinical screen. 1.8. Receipt of Medicines into Pharmacy 1.8.1. All medicines received into stock in the Pharmacy Department must be recorded on the pharmacy computer system. 1.8.2. The receipt process involves the following checks: 1.8.2.1. The physical condition of the packs supplied is checked, including the temperature at which they are delivered. MM0000 Medicines Code Page 20 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 1.8.2.2. The quantity supplied is checked. 1.8.2.3. The expiry dates are checked. 1.8.2.4. The product received is checked against the delivery note supplied with it to ensure that the supplier has correctly described what has been supplied. 1.8.3. Medicines received are placed into secure storage within the Pharmacy Department. 1.9. Receipt of Unlicensed Medicines into Pharmacy 1.9.1. Upon receipt, unlicensed medicines are put into bonded storage. 1.9.2. Following the checks listed above, and a further check to ensure that the product received meets the original specification, the product is approved for release by a suitably trained and designated person. 1.10. Receipt of Home Delivered Medicines 1.10.1. Patients receiving their medicines by home delivery should be asked to sign the delivery note supplied with their medicines. 1.10.2. A copy of the signed delivery note is then sent to the Pharmacy Department by the homecare company (the supplier). 1.10.3. It should be a condition of contract with a homecare company that no payments will be made for home delivered medicines unless a signed delivery note is received for them. 1.11. Receipt of medicines in clinical areas from pharmacy 1.11.1. Member(s) of staff receiving sealed bags or boxes of medicines from pharmacy or the pharmacy porter will be required to show a KGH photo identity badge. 1.11.2. All sealed units MUST be signed for, if being collected by a nonregistered member of healthcare staff the name of the appointed practitioner for the clinical area MUST be provided. MM0000 Medicines Code Page 21 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 1.11.3. A delivery note shall accompany each delivery of stock medicines. 1.11.4. Discrepancies shall be notified to the pharmacy department as soon as possible. 1.11.5. Medicines should be unpacked as soon as possible after delivery and stored in the appropriate location, ensuring the stock is rotated to use the shortest dated stock first. 1.11.6. Staff in receipt of drugs requiring refrigeration must ensure that they are placed immediately into the medicines fridge to maintain the cold chain. 1.11.7. For the receipt of controlled drugs refer to section 12.5. MM0000 Medicines Code Page 22 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 2. STORAGE AND SECURITY OF MEDICINES The safe and secure storage of medicines is a statutory requirement under the Medicines Act, and requires a team approach to ensure this and reduce the risk of misuse, tampering or diversion. Medicines MUST always be locked away when not in use and responsibility for this, and their safe and appropriate use, is the responsibility of the registered practitioner in charge of a ward or department during each shift who holds the medicines keys. Stock medicines MUST be stored in their original container for easy identification, at the correct storage temperature. Controlled Drugs are subject to additional specific security requirements (refer to section on Controlled Drugs). 2.1. Key Principles ALWAYS… Ensure medicines are locked away when not in use for safety and security. Keep medicines in their original labelled container (for easier identification). Segregate different strengths of the same medicine to prevent misselection. Store medicines (including vaccines) at the correct temperature; check fridge temperatures are in normal range 2-8°C daily; take action if out of range. Reorder stock medicines (during day-time hours) before you run out. Lock away medicines as soon as these are received from Pharmacy or patients. Use the oldest (short expiry date) stock first. Return medicines to Pharmacy that you will not use (only part-used, damaged or expired items should be put in the pharmacy returns box). Ensure the treatment room door is kept closed and locked when not in use. MM0000 Medicines Code Page 23 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling Store concentrated potassium solutions (e.g. strong potassium chloride injection) in the Controlled Drug cupboard; dilute before administration. NEVER… Leave medicines unattended in patient/public areas e.g. at nursing station, or when the patient is absent, or incapable of managing their medicines. Throw away a patient’s own medicines unless these are no longer required. Put refrigerated stock in the Pharmacy returns box (leave these in the fridge). Mix different packs of medicines together even if they look the same. Throw away external packaging or information leaflets, until finished. Keep excess stock (leads to increased wastage and risk of mis-selection). Remove labels from dispensed medicines. Supply stock or unlabelled (or incompletely labelled) medicines on discharge. WHERE POSSIBLE… Use up one container or strip of medicines first, before starting another. Store patient’s named medicines in their bedside locker for selfadministration. Regularly check stock to ensure it is in date, and rotate older stock to the front of the cupboard. 2.2. Responsibilities 2.2.1. The Chief Pharmacist, in consultation with appropriate medical and senior nursing staff, is responsible for establishing and maintaining a system for the secure storage of medicines in all clinical areas at Kettering General Hospital NHS Foundation Trust. MM0000 Medicines Code Page 24 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 2.2.2. The appointed Nurse-in-Charge/Matron shall be accountable for ensuring that the system is followed and that the security of medicines on the ward is maintained. 2.2.3. The accountability for the security of the medicines cupboard keys, and all the medicines held on the ward, remains with the Nurse–in-Charge/Matron even if he/she delegates this responsibility. 2.2.4. Responsibility for the security and safe use of medicines lies with the registered practitioner in charge of a ward or department during each shift. 2.2.5. The registered practitioner in charge of a ward or department must satisfy themselves that medicines are secured and used appropriately during their shift. 2.2.6. The appointed practitioner in charge of a ward or department, in conjunction with the Pharmacy team are responsible for ensuring stock levels and demand for medicines reflect normal clinical practice. 2.2.7. Excessive use of medicines must be investigated promptly; any suspicion of tampering, misuse or diversion of medicines must be reported to the Chief Pharmacist or their deputy immediately. 2.3. Medicine Keys 2.3.1. Ward and clinical areas will be issued with a maximum of 3 sets of keys. 2.3.2. Additional sets of keys over and above the standard can be obtained by agreement of the Medicines Management Committee upon demonstration of clinical need and risk management processes to ensure medicine security. 2.3.3. Medicine keys MUST be held by the registered practitioner working on the ward or department for each shift. 2.3.4. The registered practitioner in charge may only assign keys to another registered practitioner for the purpose of supplying a medicine to fulfil a prescription, or for stock management. MM0000 Medicines Code Page 25 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 2.3.5. A system of signing for the keys at handover must be adhered to. A log book must be maintained in the clinical area containing the date, the time and the signature of the nurse accepting the keys. 2.3.6. ALWAYS confirm staff identity and NEVER give keys to unauthorised staff. 2.3.7. Medicine keys MUST be kept separate from other ward or personal keys. 2.3.8. Controlled Drug keys MUST be kept separate from all other medicine keys and only given to registered staff who are authorised and have legitimate reason to access the CD cupboard (see section on Controlled Drugs). 2.3.9. Three sets of medicines keys may be held by ward or department teams on duty. 2.3.9.1. Spare keys will be retained securely within the Pharmacy Department. 2.3.9.2. Additional sets of keys over and above the standard can be obtained by agreement of the Medicines Management Committee upon demonstration of clinical need and risk management processes to ensure medicine security. 2.3.10. If keys cannot be found, it is the responsibility of the ‘nurse in charge’ to make every effort to find them as soon as possible, including contacting staff who have just gone off duty and arranging returns of any keys they have inadvertently taken home, as a matter of urgency. 2.3.11. Ensure all stock is secured and access to the clinical room is restricted. 2.3.12. In the event the keys cannot be found, the nurse in charge must contact the Pharmacy Department and seek authorisation from the Chief Pharmacist (or nominated deputy) for a replacement key and to consider the need to replace locks. 2.3.12.1. In out of hours situations contact the oncall pharmacist. 2.3.13. All incidents involving lost keys should be reported on Datix. 2.3.14. Loss of Controlled Drug Cupboard Keys should be managed as described in section 12.11. MM0000 Medicines Code Page 26 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 2.4. Storage Locations 2.4.1. Medicines MUST always be locked away. 2.4.2. Storage locations, racking, cupboards and security must meet the requirements of BS 2881:1989 (security level 1) for medicines and be approved by the Chief Pharmacist or their deputy. 2.4.3. Medicine should be stored within a secure clinical room in general wards and departments, the door MUST be closed and locked at all times when not in use; ALL staff have a responsibility for ensuring this. 2.4.4. Internal Medicines (tablets, capsules, liquid medicines and injections) MUST be stored separately from external medicines (topical creams etc). 2.4.5. Schedule 2 (and some schedule 3) Controlled Drugs MUST always be locked in a separate Controlled Drug Cabinet (see section 12 Controlled Drugs). 2.4.6. Intravenous fluids and diluents for injection (including plastic ampoules of water for injections and Sodium Chloride 0.9%w/v injection) MUST be stored off of the floor and may be stored on clean open racking or shelving within a locked clinical room. 2.4.7. Reagents, disinfectants and antiseptic preparations should be stored in a separate cupboard which meets of BS 2881:1989 (security level 1) specifications. 2.4.8. Volatile substances including flammable liquids, gases and aerosols must be stored in a separate locked cabinet that has been certified for this use by a Fire Safety Officer. 2.4.9. If drug trolleys are used for medicine administration rounds these MUST be locked when not in use and stored in a locked clinical room. 2.4.10. Small bedside cabinets may be used to lock away patient’s own medicines on wards (see section 8 on self-administration of medicines). MM0000 Medicines Code Page 27 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 2.4.11. Medicines for clinical emergencies (e.g. CPR boxes) should be stored on the resuscitation trolley where they are readily accessible. They are held in a tamper evident box (the seal should be checked daily), and once used returned to Pharmacy for immediate replacement. Outside of Pharmacy hours replacement boxes/rolls can be found in the emergency drug cupboards. 2.5. Fluid warmers 2.5.1. It is recognised practice for certain intravenous fluids to be warmed to body temperature prior to administration in designated fluid warming devices. 2.5.2. Intravenous infusion bags (e.g. sodium chloride 0.9%, glucose 5%, Hartmann’s, Gelofusine®) may be stored in a fluid warmer for up to 20 days (bag size 500mL and above) or 10 days (bag size less than 500mL). The outer protective layer should not be removed. 2.5.3. Intravenous fluids must only be warmed in designated fluid warming equipment. 2.5.4. Once removed from the warmer, bags may be used within the normal shelf life of the product, however they must not be returned to the warmer. 2.5.5. Infusion bags that have had medicines added to them must not be warmed. 2.6. Temperature Monitoring 2.6.1. Where medicines are stored the temperature should not exceed 25°C. 2.6.2. For all medicine storage areas, the ambient room temperature should be recorded daily using a maximum/minimum thermometer (these are available from Pharmacy Stores, with instructions for use). MM0000 Medicines Code Page 28 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 2.6.3. If in areas where medicines are stored the temperature exceeds 25°C, medicines issued as ward stock will have a reduced expiry date in line with NHS Quality Control recommendations. These will be: - 2.6.3.1. 12 months for storage in areas up to temperatures of 30°C 2.6.3.2. 6 months for storage in areas up to temperatures of 35°C. 2.6.4. Where the temperature rises above 35°C for longer than 24 hours, contact Pharmacy Medicines Information for further advice. 2.7. Refrigerated storage 2.7.1. A locked, pharmaceutical grade refrigerator must be used for medicines that require storage between 2-8 degrees centigrade, with an integral digital temperature display and audible alarm for high/low temperature. 2.7.2. Food or specimens must NEVER be stored in the medicines refrigerator. 2.7.3. The temperature of medicines refrigerators MUST be checked daily and recorded on the ‘temperature monitoring chart’. 2.7.4. Where temperatures fall outside of the specified temperature range the following actions MUST be taken:- 2.7.4.1. Contact Estates to check the integrity of the refrigerator. 2.7.4.2. Contact the Pharmacy Medicines Information to ensure that medicines remain fit for use (in out of hours contact the oncall pharmacist.) 2.7.5. Refrigerators should be kept clean, tidy, frost-free and not overfilled. Particular care should be taken to ensure temperature labile products such as vaccines are not frozen. 2.7.6. Where a product has been stored incorrectly, do not use until advice has been obtained from the Pharmacy Department to ensure it remains fit for use. MM0000 Medicines Code Page 29 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 2.8. Stock Maintenance 2.8.1. Common medicines, as well as those required for urgent or emergency treatment are stocked in wards and departments throughout the hospital. 2.8.2. Medicines MUST be retained in their original packaging to help with positive identification; do not remove blister strips from outer packaging. 2.8.3. Different strengths of the same medicine MUST be separated to reduce the risk of mis-selection. NEVER mix different packs of medicines together, even if they look the same. 2.8.4. The registered practitioner in charge of a ward or department is responsible for the safe use and security of stock medicines during a shift. 2.8.5. Stock usage should be checked regularly during shifts and at handover. 2.8.6. Rotate stock to ensure the oldest stock is used first and only one strip or pack is used at a time to facilitate recycling of unused stock. 2.8.7. Regular stock maintenance and top-ups are conducted by pharmacy staff. 2.8.8. Always reorder stock before you run out and in normal working hours. 2.8.9. Stock medicines received from Pharmacy MUST be signed for, and locked away, as soon as possible, by a registered practitioner on the ward or department. The registered practitioner takes responsibility for the secure storage of medicines. 2.8.10. Excessive stock usage or ad-hoc orders must be reported to the registered practitioner in charge of the ward and department, and senior pharmacy logistics manager, to investigate. 2.8.11. Stock lists are reviewed annually by the appointed practitioner in charge and the CBU lead pharmacist to ensure stock medicines and demand reflect normal clinical practice. MM0000 Medicines Code Page 30 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 2.8.12. Any changes in clinical practice must be notified to the responsible pharmacist so that stock levels of relevant medicines can be adjusted. 2.8.13. Stock levels of Controlled Drugs and other potentially abusable medicines are reviewed quarterly, and regular reports of medicines use provided to the appointed practitioner in charge, and the responsible pharmacist, to confirm that use reflects legitimate clinical practice. 2.8.14. Registered practitioners should satisfy themselves that stock is only used for the purpose intended and should report any suspicious behaviour or loss of medicines to the appointed practitioner in charge and complete a datix incident report. 2.8.15. Any suspicion of tampering, misuse or diversion of medicines must be reported to the Chief Pharmacist or their deputy immediately. 2.9. Return of medicines 2.9.1. Excessive medicines stock or medicines that are no longer required should be returned to Pharmacy for recycling or safe disposal (as below). 2.9.2. Unwanted solid dose medicines (e.g. tablets and capsules) should be returned in their original packaging, by placing these in the green pharmacy bins within the locked clinical room. 2.9.3. Refrigerated items for return, should be left within the locked medicine fridge, but separated from stock that is in date and being used. Pharmacy should be notified on the next working that items require removal, using the pharmacy communication diary. 2.9.4. Controlled Drugs for return MUST be left locked in the CD cupboard. Refer to Section 12.17 on Controlled Drugs for secure return to Pharmacy. 2.9.5. Patients’ own medicines that are no longer required should be disposed of with the patient’s permission (see section 7.3 on Patients’ own medicines). MM0000 Medicines Code Page 31 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 2.10. Disposal of medicines 2.10.1. Some part-used or expired aqueous (water-based) medicines, in normal clinical quantities, may be disposed of in wards and departments. 2.10.2. Small quantities (e.g. part-used ampoule or syringe) may be placed in a clinical sharps bin. 2.10.3. Larger quantities (e.g. part-used infusion bag) should be emptied down the foul sewer with plenty of water. 2.10.4. Controlled drugs must NOT be disposed of down the foul sewer, refer to section 12.17Error! Reference source not found. on Controlled Drugs for specific guidance for safe ward disposal. 2.10.5. Medicines returned to Pharmacy for destruction will be disposed of in accordance with current Trust waste management policy and procedures. 2.11. Ward and department closures 2.11.1. The safe and secure storage of medicines must be maintained even when wards or departments are closed, and remain the responsibility of the appointed practitioner in charge. 2.11.2. Where wards or departments are routinely closed for short periods (e.g. weekends), medicines stock (including controlled drugs) may be retained. 2.11.3. The keys for all medicine cupboards MUST be stored securely in a designated area within a locked key safe during periods of routine closure. 2.11.4. Where wards or departments are closed for longer periods (greater than 2 weeks) then all medicines stock MUST be returned to Pharmacy, by arrangement. 2.11.5. Medicine keys will be retained by the appointed practitioner in charge. MM0000 Medicines Code Page 32 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 2.12. Audit, Assurance and Accountability 2.12.1. The Appointed practitioner in charge of a ward or department should satisfy themselves that medicines are stored securely and used safely. 2.12.2. Compliance with standards for medicines security (doors to clinical rooms, medicine cupboards and medicine fridges are locked when not in use) are reported monthly using the Trust Ward Assurance tool. Note ALL medicine cupboards, medicine fridges and the clinical room door must be locked to meet the standard. 2.12.3. Pharmacy undertakes a rolling audit of compliance against standards, providing regular assurance reports to Medicines Management, CBU Governance and Trust Governance Committees. 2.12.4. Where standards are not met, registered staff in charge of wards and departments will be held to account by Professional Leads/ Managers within their Division. 2.12.5. Where failure to secure medicines results in misuse or diversion, staff involved may be subject to professional or Trust disciplinary action. Where misuse or diversion involves Controlled Drugs, this could result in criminal prosecution. MM0000 Medicines Code Page 33 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 3. MEDICINES RECONCILIATION Medicines reconciliation (MR), as defined by the Institute for Healthcare Improvement, is the process of identifying an accurate list of a person's current medicines and comparing them with the current list in use, recognising any discrepancies, and documenting any changes, The term 'medicines' also includes over‑the‑counter or complementary medicines, and any discrepancies should be resolved with all reasons documented within the medical notes. It encompasses two elements, firstly obtaining an accurate medication history and secondly reconciling the history with the in-patient prescription ensuring all differences are intended: Collection of the medication history from a variety of sources – This involves taking a medication history and gathering relevant information about the patient’s medicines. The medication history should be collected from the most recent and reliable sources, ideally this will be the patient’s summary care record. Where possible, information should be cross-checked and verified. The person recording the information should always record the date that the information was obtained and the source of the information. Checking that medicines prescribed on admission for the patient are correct – This involves ensuring that the medicines, doses and formulations that are prescribed for the patient are correct and that discrepancies are identified and understood as intentional or unintentional. Discrepancies need to be communicated and unintentional changes addressed. MM0000 Medicines Code Page 34 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 3.1. Medicines Reconciliation Checklist This checklist may be used as a guide when taking and documenting a patient’s medication history. 1. Any known allergies or drug intolerances and nature of the reaction. 2. A complete list of all of the medicines currently being taken by the patient. 3. Dose, frequency, formulation and route of all the medicines listed. 4. 5. Specific medication you may want to ask about include:Inhalers Eye drops Topical Preparations Once weekly medications Injections OTC medicines Oral contraceptives Hormone replacement therapy Nebulisers Home oxygen Herbal remedies Insulin, including the type of device Any medicines delivered to the home Any medicines which have recently started or been stopped Additional information for specific drugs e.g. indication for warfarin or corticosteroids, day of week of administration for once weekly medication (bisphosphonates, methotrexate). 6. Medication management in own home e.g. Dosette® boxes, district nurses, family support. 7. Source/s used to obtain full medicines reconciliation. 8. Name, signature and date of practitioner carrying out medicines reconciliation. 3.2. Medicines Reconciliation Process 3.2.1. Medicines reconciliation should be carried out for all patients by the admitting practitioner as part of the clerking process within 6 hours of admission. 3.2.2. Documentation of medication history should always be made in the patient medical record, noting sources used and dated and signed by the admitting healthcare professional. MM0000 Medicines Code Page 35 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 3.2.3. This information may be obtained from multiple sources including the patient/carer, their labelled medicines (patient’s own drugs), the GP admission letter, a repeat prescription slip, Medicines Administration Records or following discussion with the GP practice, or nursing/care home. 3.2.4. Where possible two or more sources should be used to verify the information, and MUST be used where the patient or their carers have communication difficulties (e.g. language, cognitive difficulties). 3.2.5. A prescription chart (a list of medicines to be administered) should be written for the patient by the admitting healthcare professional. 3.2.6. Intentional medication changes should always be documented in the patient’s medical record giving reasons for the change. These can also be documented in the appropriate section of the prescription chart. 3.2.7. Unintentional discrepancies highlighted by other healthcare professionals or the patient, should be appropriately prioritised and resolved. 3.2.8. A member of the Pharmacy team should be involved in MR as soon as possible after the admission of an adult patient. 3.2.9. The prescription chart should be signed and dated by the member of the Pharmacy team to confirm completion of medication history; this includes pharmacists, accredited pharmacy technicians and accredited pre-registration pharmacists. 3.2.10. Reconciliation of this medication history with the prescription chart should ideally be completed by a pharmacist within 24 hours of the patient’s admission and will be completed within 72 hours for patients admitted at the weekend. 3.2.11. If there are concerns about the reliability or accuracy of the medication history, a member of the Pharmacy team should be contacted to help resolve these. 3.2.12. All medication changes and reasons for the changes should be documented on the discharge or transfer letter. MM0000 Medicines Code Page 36 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 4. PRESCRIBING In this section “prescriber” means any practitioner legally authorised to prescribe under the Medicines Act 1968 or subsequent amendments. Thus this policy applies equally and fully to both medical and non-medical practitioner prescribing. All KGH prescribers have a responsibility to ensure that a copy of their usual signature is held in the Pharmacy Record of Prescribers’ Signatures. KGH assures accuracy and appropriateness of prescribing via the various staffing (prescribing, nursing, pharmacy) involved in the management of patients. The clinical pharmacy services assess the accuracy of all prescribing documentation through regular prescription review. Assurance on prescribing accuracy is provided through regular audit (Appendix 1) from the Pharmacy team. 4.1. Who can Prescribe There are two categories of prescribers within KGH. These are: 4.1.1. Independent prescribers - professionals who are responsible for the initial assessment of the patient and for devising the broad treatment plan, with the authority to prescribe the medicines required as part of that plan. This includes medical staff, dentists and authorised nurse and pharmacist prescribers who have successfully completed an independent prescribing course. 4.1.1.1. nurse and pharmacist independent prescribers are able to prescribe any medicine for any medical condition within their competence, including any controlled drug in Schedule 2, 3, 4 or 5 of the MDR 2002 Regulations, as amended. MM0000 Medicines Code Page 37 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 4.1.1.2. optometrist Independent Prescribers can prescribe any licensed medicine for ocular conditions affecting the eye and surrounding tissue, but cannot prescribe any controlled drugs. 4.1.1.3. physiotherapists and podiatrists or chiropodists can prescribe any licensed medicine provided it falls within their individual area of competence and respective scope of practice as independent prescribers, but cannot prescribe any controlled drugs. 4.1.2. Supplementary prescribers - professionals who are authorised to prescribe certain medicines for patients whose condition has been diagnosed or assessed by an independent prescriber, which in this situation must be a medical practitioner, within an agreed clinical management plan (CMP). Professionals who can undertake supplementary prescribing are nurses, pharmacists and certain allied health professionals (chiropodists/podiatrists, physiotherapists, optometrists and radiographers). Supplementary and Independent prescribers must be registered as such with the relevant regulatory body and any activity carried out by them must have Trust approval and authorisation. Where a nurse or a pharmacist is the supplementary prescriber, a CMP may include any medicine prescribable at NHS expense, this includes controlled drugs, unlicensed and off label medicines. The use of a medicine off label must have the joint agreement of both prescribers and the status of the medicines should be recorded in the CMP. Allied health professional supplementary prescribers are not allowed to prescribe controlled drugs. 4.1.3. The Trust considers the following as a guide to good practice for non-medical prescribers: MM0000 Medicines Code Page 38 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 4.1.3.1. Ensure you have notified your professional registration body about your prescribing qualification. 4.1.3.2. Ensure your job description includes a reference to nonmedical prescribing in your role. 4.1.3.3. Adhere to the principles of good prescribing in the policy for prescribing medicines. 4.1.3.4. Use the appropriate approved stationary for prescribing. This could be KGH internal prescribing forms and charts or FP10 (HNC) forms which patients may choose to have dispensed at a community pharmacy or the hospital pharmacy. 4.1.3.5. 4.2. Never prescribe for someone who is not one of your patients. General Prescribing Principles 4.2.1. The Trust does not support prescribers prescribing for themselves (privately or otherwise) or for family/friends to which the prescriber may have close personal contact Ref: GMC Guidance for Doctors - Prescribing Guidance - Need and Objectivity: http://www.gmc-uk.org/guidance/ethical_guidance/14318.asp 4.2.2. Registered medical and non-medical prescribers are permitted to prescribe within their scope of competence and current legislation. 4.2.3. The person who signs a prescription is responsible for its accuracy and the appropriateness for the patient it is prescribed for. 4.2.4. Prescribers must make themselves familiar with the BNF and the processes involved in writing a legally correct prescription. All non-medical prescribers are required to follow the relevant NonMedical Prescribing Policy. 4.2.5. Medicines must be prescribed on official Trust prescription stationary. MM0000 Medicines Code Page 39 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 4.2.6. Medicines should be prescribed only when they are necessary, and in all cases the benefit of administering the medicine should be considered in relation to the risk involved. 4.2.7. Treatment options must be carefully discussed with the patient to ensure that the patient is willing and able to take the medicine as prescribed. In particular, the patient should be helped to distinguish the possible adverse effects of prescribed drugs from the likely outcomes of the untreated medical disorder. 4.2.8. If the beneficial effects of the medicine are likely to be delayed, the patient should be advised of this. 4.2.9. Prescribers must listen to patients, take account of their views, and respond honestly to any questions asked. Information must be presented in a format that can be understood. 4.2.10. Treatment and care should take into account a patient’s individual needs and preferences. 4.2.11. Good communication, supported by evidence-based information, is essential. 4.2.12. Healthcare professionals have a duty under the Disability Discrimination Act (2005) to make adjustments to ensure that all people have the same opportunity for good health. 4.2.13. Healthcare professionals should follow the code of practice that accompanies the Mental Capacity Act (2005) if concerned about patient capacity. 4.3. Range of Medicines to Prescribe 4.3.1. Only medicines that have been approved for use by the New Medicines Group in the Trust prescribing formulary, Northamptonshire Prescribing Advisory Group, or within an Individual Funding Request may be prescribed. 4.3.2. KGH and Nene CCG will ensure that all prescribing clinicians are aware of the Trust formulary and the Northamptonshire Medicines Formulary and Traffic Light system. MM0000 Medicines Code Page 40 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 4.3.3. The Traffic light system provides a framework for defining where clinical and therefore prescribing responsibility should lie through categorisation of individual drugs (http://nww.pathfinderrf.northants.nhs.uk/nene/therapeutics/traffic-light-drugs/). 4.3.4. Medicines that are classified as 'red' on the Traffic Light list are considered not suitable for prescribing in primary care and so clinicians should not approach primary care prescribers to prescribe these. 4.3.5. This also applies to “double red” as these medicines are not recommended for use in the Northamptonshire Health Community because of lack of evidence of clinical effectiveness, cost prioritisation or concerns over safety. 4.3.6. “Amber” medicines are initiated in secondary care with the potential to transfer to the GP, with their prior agreement, under a shared care agreement. Care should only be transferred when all of the approved shared care agreement requirements for that medicine have been met. Documents associated with shared care can be found http://nww.pathfinderrf.northants.nhs.uk/nene/therapeutics/traffic-light-drugs/ 4.3.7. If hospital clinicians wish to prescribe medicines that are not currently included on the formulary or supported for specialist prescribing by the New Medicines Group (NMG) they should submit a request to the New Medicines Group (NMG) for evaluation and possible inclusion in the formulary. 4.4. Verbal Orders 4.4.1. Verbal orders are not acceptable at KGH with the exception of those drugs used in life threatening situations such as cardiac arrest or where the prescriber is scrubbed for an aseptic procedure (e.g. in theatre). 4.4.2. Verbal orders are given to a registered nurse by a medical practitioner when they are in the same room. MM0000 Medicines Code Page 41 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 4.4.3. Verbal orders must be restricted to medicines commonly prescribed on the ward/department and be used only in an emergency situation. 4.4.4. The person accepting a verbal order must repeat the name of the patient and prescription back to the prescriber and get a second person who is present to confirm the details of the verbal instruction with the prescriber. 4.4.5. The instruction is entered on to the “once only” section of the prescription. It is identified as a verbal instruction and the name of the doctor/bleep entered into the signatory box or added as a note to the electronic prescription the identity of the person making the entry should also be made apparent on the prescription chart. 4.4.6. The medical practitioner must countersign any verbal instruction within 12 hours and cannot delegate this to another individual. 4.4.7. Controlled drugs must never be given or prescribed as a verbal order. 4.4.8. A Pharmacist may receive verbal authority from the original prescriber to alter or rectify a prescription item for example, following an intervention. If using paper charts all alterations must be endorsed “PC” and the name of the prescriber stated and the prescription should be signed and dated by the Pharmacist. The Pharmacist must read the alteration or addition back to the prescriber who must then confirm it. 4.5. Inpatient Prescribing 4.5.1. The inpatient prescribing documentation 4.5.1.1. The standard prescribing documentation must be used for all inpatients across the Trust unless there is an authorised alternative in use, such as the surgical short stay chart. 4.5.1.2. Authorised alternatives are only valid for use in the clinical area specified on the document. When patients are transferred to another clinical area with an authorised alternative in use (e.g. ward to intensive care), prescriptions MM0000 Medicines Code Page 42 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling must be rewritten onto the prescribing documentation in use for that particular clinical area. 4.5.1.3. The registered prescriber must complete all the required details, sign and date for the prescription to be valid. The prescriber should make every effort to check other records before adding new medicines (eg A&E ‘cas card’) to prevent inadvertent overdose. 4.5.1.4. Where additional specialised documents are used to support the prescribing of specific drugs (e.g. aminophylline, insulin or warfarin) these should be referred to on the inpatient prescription chart. 4.5.2. General Instructions for prescribers who must 4.5.2.1. Write in Black indelible ink if prescribing on paper prescriptions. 4.5.2.2. Complete all patient identifiable information, to include name, address, date of birth, hospital and NHS numbers. (Preprinted labels are encouraged). 4.5.2.3. Document patient’s current drug history in the patient’s casenotes. 4.5.2.4. Document known drug hypersensitivities in the section allocated for Drug Allergy/Sensitivities. 4.5.2.5. Document the weight (in kilograms) of the patient on the prescription. 4.5.2.6. Inform the registered nurse-in-charge whenever new prescriptions are written, in order that supplies can be obtained at appropriate times. 4.5.2.7. Specify the indication for any antimicrobial prescribed. 4.5.2.8. Specify course length/ finish date on the prescription where required. 4.5.2.9. Sign and date all prescriptions THE PRESCRIBER MUST SIGN THE PRESCRIPTION LEGIBLY i.e. it should be recognisable to pharmacy staff and the health professional responsible for administering the MM0000 Medicines Code Page 43 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling medicine to the patient. The prescriber should print his/her name and bleep number at least once on the prescription, to facilitate ease of contact if a query arises. 4.6. Allergies or Sensitivities 4.6.1. All prescribers are responsible for entering/checking any known allergy information, including complementary/alternative medicines and latex, in the allergy section of the prescription before prescribing any medications on the prescription chart. 4.6.2. This information must be transferred to subsequent prescription charts. 4.6.3. It is not acceptable to leave the allergy box blank. State “None Known” or “NKA” or “NKDA” if there is no known (drug) allergy 4.6.4. Where the patient has identified an allergy, the nature of this allergy must be ascertained and documented in the allergy box. i.e. Penicillin – anaphylaxis. 4.6.5. Whether an allergy has been identified or not, the allergy box must be initialled and dated by the prescriber. The information must also be clearly stated in the patient’s notes. 4.6.6. Registered nurses, midwives, pharmacists and pharmacy technicians are authorised to complete the allergy box of a prescription chart but should state qualifications after their signature. This is not just the responsibility of medical staff. 4.6.7. All staff MUST always clarify the allergy status of the patient before dispensing or administering a medicine. The registered prescriber must enter all known allergies/sensitivities in the relevant section of the prescribing documentation before prescribing any medicines. MM0000 Medicines Code Page 44 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 4.7. Prescribing for All Medicines 4.7.1. Name and form of medication 4.7.1.1. The name of the medicine must be written in block capitals. Abbreviations (e.g. ISMN) and chemical formulae (e.g. FeSO4) are not acceptable. Approved names must be used. This will normally be the generic name except for: 4.7.1.2. a compound preparation, e.g. Seretide. 4.7.1.3. a preparation with specific pharmacokinetic properties, e.g. a specific slow release preparation where the BNF states that prescribing should be by brand. 4.7.1.4. Solid dose oral forms of medication will be given unless another form or route is indicated. For liquids and topical preparations the strength and form must be stated, wherever possible. 4.7.2. Dose of Medicine 4.7.2.1. The dose must be expressed in metric units avoiding decimal places. 4.7.2.2. Do not use decimal points that are unnecessary e.g. 3mg not 3.0mg. 4.7.2.3. Where use of a decimal point is unavoidable a zero should be written in front of the decimal point where there is no other figure e.g. 0.5ml not .5ml. 4.7.2.4. The word “micrograms” and “nanograms” must be written in full and not abbreviated to mcg or μg or ng to avoid confusion with milligrams (mg). 4.7.2.5. “g” is a permitted abbreviation for gram. 4.7.2.6. “mg “ is a permitted abbreviation for milligram. 4.7.2.7. Only standard liquid preparations that cannot be expressed by concentration e.g. 5mg in 5ml, should be prescribed as volume alone e.g. lactulose. Other preparations must be prescribed by weight or units e.g. amoxicillin syrup 500mg or colecalciferol 1000units. MM0000 Medicines Code Page 45 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 4.7.2.8. The word unit must be written in full rather than abbreviated to “U” or “IU”. 4.7.2.9. The blood unit symbol ּסmust not be used as an abbreviation for prescribing units of medicines as it can frequently be confused with a “0” (zero) and may lead to 10 times the dose of insulin or heparin being administered in error. 4.7.2.10. Roman numerals or other symbols, for example ”ii” are also the cause of medication errors and must not be used. If there is no obvious or practical tablet/capsule strength e.g. senna, the number of tablets to be administered should be expressed in numbers e.g. “2” tabs not “ii”. 4.7.3. Route of Administration 4.7.3.1. The route must be specified. The following abbreviations are permitted: IV Intravenous PR Per Rectum IM Intramuscular PV Per Vagina INH Inhalation ID Intradermal SC Subcutaneous ORAL, O or By Mouth PO SL Sublingual TOP Topical NG Nasogastric NJ Nasojejunal tube PEG Percutaneous PEJ Percutaneous NEB 4.7.3.2. endoscopic endoscopic gastrostomy jejunostomy tube tube Nedbulised Buccal Buccal Other instructions must be written in full to avoid confusion e.g. intrathecal preparations used for the eye, ear and nose indications must state in full the intended site of application i.e. “Right Eye”. MM0000 Medicines Code Page 46 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 4.7.3.3. The practice of writing more than one route of administration, for example “O/IM” in the same box should be avoided and separate prescriptions should be written out for each route stating either/or. This is because there are a number of medicines that have very different pharmacokinetic profiles and hence doses and routes are not always safely interchangeably and can lead to over or under dosing. In addition there is the risk that both routes may be used simultaneously. The registered prescriber must specify the time of medicine administration. 4.7.4. Times of Administration. 4.7.4.1. The Prescriber must specify the time at which the medicines is to be administered. 4.7.4.2. If the medicine is to be administered at non-standard times or is a once only dose the prescriber should communicate this to the registered nurse-in charge for the shift. 4.7.5. Duration of Treatment 4.7.5.1. Where a defined course is required the length of course must be indicated at the time of prescribing. 4.7.5.2. Prescriptions for antibiotics should normally be written for a limited period with an automatic stop on the prescription made 5 days after initiation of therapy. (please refer to the Trust Antimicrobial Policy). 4.8. Prescribing for Intravenous Medicines 4.8.1. Intravenous fluids must be prescribed on the IV fluid chart or appropriate section of the prescription. The prescription must state the name, strength and volume of the fluid, any additives required, the duration or rate of administration and should be signed by the prescriber. All additions to fluids other than electrolytes must also be prescribed on the prescription chart. MM0000 Medicines Code Page 47 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 4.8.2. Medicines to be given intravenously as discrete bolus injections must be prescribed on the standard prescription chart following the requirements in Section 4.8. 4.8.3. Medicines to be given by intravenous infusion or as additives to intravenous fluids must be prescribed on the appropriate section of the prescription chart stating in addition in the ‘medicine’ box, the infusion fluid, volume and duration of administration. 4.8.4. Where specialist prescription forms are used, e.g. gentamicin, reference should be made to this in the main inpatient prescription chart. MM0000 Medicines Code Page 48 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 5. PREPARATION OF MEDICINES The preparation and administration of medicines is a high risk activity and prone to error. Over 60% of errors reported to the National Patient Safety Agency occur during preparation and administration. Kettering General Hospital promotes the principles outlined by the National Patient Safety Agency 2007 Promoting safer use of injectable medicines, with the aim of reducing the risk to patients, and enhancing patient safety. If in doubt, do not proceed; check with another member of the medical, nursing or Pharmacy team. Where possible and practicable practitioners should use the online injectable medicines guide MEDUSA resource as the primary source of injectable medicines information. The Trust Pharmacy Department, current BNF, UCL Injectable Drug Administration Guide, Electronic Database (where available) and medicine information leaflet may also be used to provide this information. 5.1. Responsibilities 5.1.1. The practitioner in charge of the clinical area is responsible for ensuring that standards for medicines preparation fall within the requirements of this code. 5.1.2. The suitably qualified health professional carrying out the medicine preparation should understand the prescription and should have knowledge of the common indications, side-effects and dosages of the medicine prescribed. 5.1.3. They should also be aware if there are any risks in handling or administration of the medicine and whether any specific equipment is required. Local procedures for handling high risk/hazardous material should be referred to where appropriate. MM0000 Medicines Code Page 49 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 5.1.4. It is the practitioner’s responsibility to ensure that information sources used are current. If hard copies of information contained on the electronic database are stored in files these should be up to date and include published references. 5.1.5. The Healthcare professional administering the medication will be accountable for his/her practice in accordance with their professional code of conduct and standards for administration of medicines. 5.2. Key Principles 5.2.1. A Designated registered practitioner MUST prepare, check and administer medicines to patients. 5.2.2. Students (nurses, midwives and medical students) or other professionals in training who are not yet registered must be under the direct supervision of a registered practitioner who is then responsible for the preparation, administration and documentation. 5.2.3. Advice MUST be sought by a practitioner if they are unsure about any aspect of medicine preparation. 5.2.4. Always check that medicines containers, outer wrappers and seals are intact, and show no signs of damage or tampering, before use. 5.2.5. It is essential to ensure that the medicine to be administered is compatible and stable within the diluent or intravenous fluid being used. 5.2.6. IV syringes must NOT be used to measure or administer oral medicines. 5.2.7. IV syringes must NOT be used to measure insulin doses. 5.2.8. Medicines Must Never be added to: Blood Plasma Blood products MM0000 Medicines Code Page 50 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 5.3. Total Parental Nutrition (TPN) Mannitol Sodium Bicarbonate Gelofusin General Principles 5.3.1. Only medicines that have been supplied by the Trust Pharmacy service or patient’s own medicines that have been approved for use should be administered to patients. 5.3.2. Medicines MUST only be prepared, checked and administered to a patient by a designated registered Practitioner. This includes: 5.3.2.1. A practitioner in training, but only when under the direct supervision of a Designated Practitioner who remains responsible for ensuring that the correct procedure takes place. 5.3.2.2. It is acceptable to continue an already established infusion, which has been instigated by another practitioner following the principles, within this document, or medication prepared within a pharmacy aseptic unit and clearly labelled for that patient. 5.3.3. Prescribed medicines should be administered within 60 minutes either side of the prescribed time. 5.3.4. Clinically urgent medicines (such as intravenous antibiotics) should be prepared and administered within 30 minutes of the prescribed time. 5.3.5. Where urgently required medicines are not stocked in the pharmacy, the prescriber should discuss the prescription directly with a member of the Pharmacy team to confirm the prescription and supply arrangements. 5.3.6. All medicines must be labelled. Where a medicine is prepared in a clinical area the prepared dose must also be labelled. MM0000 Medicines Code Page 51 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 5.4. Ward Preparation 5.4.1. Wherever possible medicines should be supplied from Pharmacy in a ‘ready to administer form’, requiring no further manipulation, calculation or dilution, prior to administration. 5.4.2. In most cases, where more than three dosage units (i.e. three tablets, ampoules, and vials) have to be administered as one dose, this should be checked using the current BNF, and /or confirmation should be sought from a Pharmacist. (This is not always required where low strength dose units are commonly used e.g. warfarin 1mg or prednisolone 5mg tablets.) 5.4.3. Where medicine preparation is performed outside of the Pharmacy Department, the following points must be observed: 5.4.3.1. Read the prescription carefully. Determine the medicine name, dose, diluent, route for administration and expiry date. 5.4.3.2. If a dosage calculation is required, this information should be included as part of the prescription either by the Prescriber or the Pharmacist, or within an approved protocol/standard operating procedure, so that the practitioner administering the dose is clear about the actual amount to administer. 5.4.3.3. Where a dose calculation is involved or where the medicine is intended for intravenous administration, a second registered practitioner MUST check the medicine preparation (and administration see section 6.2 5.4.3.4. If the Designated practitioner is unclear as to the correct diluent or precise method for preparation, they MUST obtain this information using an appropriate reference source or discuss with a member of the Pharmacy team. 5.4.3.5. An appropriate area should be identified where intravenous medicines are to be prepared; where possible this area should be separated from direct patient areas and enclosed (all doors and windows should be closed). These precautions reduce the risk of microbial contamination and interruptions, which can lead to medication errors. MM0000 Medicines Code Page 52 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 5.4.4. Intravenous medicines MUST be prepared using Aseptic NoTouch Technique (ANTT) in accordance with Trust policy and procedures. 5.4.4.1. ALWAYS CHECK that medicinal products are suitable for use, have been stored correctly and show no evidence of damage BEFORE use: 5.4.4.2. Check packaging and seals have not been damaged and show no sign of tampering. If in doubt, do NOT use and return to pharmacy immediately. 5.4.4.3. Check the product label is clear, within expiry date, and the container and contents show no signs of decomposition (e.g. colour change/precipitate in liquid injections). 5.4.4.4. Check that any flexible plastic containers (e.g. infusions and plastic ampoules) are not leaking by squeezing them. If leaking, they must NOT be used and MUST be returned to pharmacy immediately. 5.4.5. All medicines MUST be labelled to identify the medicine, and where appropriate the strength and total dose. Where medicines are prepared outside Pharmacy: 5.4.5.1. In critical care areas the Royal College of Anaesthetists (RCOA) critical care labelling system is used to differentiate products. 5.4.5.2. In other areas, pre-printed syringe labels or blank labels for infusions MUST be completed and applied during preparation to differentiate products and prevent medication errors. 5.4.5.3. The only exception to this is where a medicine is drawn up and immediately administered to a patient by the same member of staff, without putting down the product. 5.4.6. Medicines prepared outside of pharmacy are for immediate use and administration should commence as soon as practicable after preparation has been completed, this should not exceed 60 minutes in advance of the anticipated time of requirement. MM0000 Medicines Code Page 53 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 5.5. Use of oral syringes 5.5.1. IV syringes MUST NOT be used to measure or administer oral liquid medicines by mouth or enteral feeding tube. 5.5.2. A medicine cup or 5ml spoon should be used to measure and administer oral liquid medication except in the following situations where a PURPLE oral/enteral syringe should be used: The dose cannot be accurately measured using a 5ml spoon. Administration via an enteral feeding tube. Administration from a medicine cup or spoon is unsuitable e.g. babies and young children. 5.5.3. ‘Press-in bungs’ are available for liquid medicine bottles to allow easy removal of the dose using a PURPLE oral syringe. 5.5.4. Once an oral syringe has been used to administer medication directly to a patient or via an enteral feeding tube, it must NOT be used to withdraw further doses of that or any other medication from an original container, to reduce risk of cross-contamination. 5.5.5. Used oral syringes that are contaminated with medicines must be disposed of immediately, in a clinical sharps bin in accordance with Trust waste disposal policy. 5.6. Insulin syringes 5.6.1. Patient doses of insulin must NEVER be measured using an Intravenous syringe, which can lead to medication errors. 5.6.2. Bespoke insulin syringes or insulin ‘pen’ devices MUST always be used to measure insulin doses. 5.6.3. Where appropriate diabetic patients should be encouraged to manage and self-administer their own insulin, as part of the Trust self-administration policy (see section 8). 5.6.4. Insulin products MUST always be locked away in the patient’s bedside locker and stock vials in a locked refrigerator. MM0000 Medicines Code Page 54 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 6. CHECKING OF MEDICINES Checking is essential at all stages of the medicines use process. This involves scrutiny and reconciliation of available information, to verify that the intended medicine is prescribed, prepared and administered correctly. The multi-professional hospital environment lends itself to second checking, which is recommended for all medicines and considered essential for complex medicines (including intravenous preparations and all medicines for children), to safeguard patient care. Assumptions must NOT be made; factual information MUST be used and all checks made on an individual patient basis. 6.1. Key Principles 6.1.1. Practitioners MUST check any medicine activity that they undertake. 6.1.2. An accurate medication history MUST be recorded in the health record. 6.1.3. A second independent check MUST be made before the administration of high risk medicines or medicines for children. 6.1.4. ‘Clinical’ checks MUST be carried out by competent registered staff. 6.1.5. Checkers MUST alert a designated practitioner if they are concerned about correct identification, preparation or administration of a medicine. 6.1.6. Two sources MUST be used to reconcile medicines where patients or their carers have communication difficulties. 6.1.7. Appropriate checks are made for preparation and administration of high risk medicines (e.g. IV medicines, cytotoxic chemotherapy etc.) MM0000 Medicines Code Page 55 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 6.2. General Procedures 6.2.1. Checks should be carried out by a registered practitioner undertaking any medicine activity, who is professionally responsible for their own actions. 6.2.2. It is considered best practice that a second independent check occurs for all preparation and administration of all medicines. Second independent checks MUST be undertaken for: 6.2.2.1. Controlled drugs (Schedule 2) 6.2.2.2. Paediatric medicines 6.2.2.3. Intravenous medicines 6.2.2.4. Cytotoxic chemotherapy 6.2.2.5. Complex calculations for preparation or administration 6.2.2.6. Epidural and intrathecal medications 6.2.3. Checking should be undertaken in an unhurried manner, and wherever possible in a calm environment, without interruptions. 6.2.4. Checking involves careful triangulation of information from the prescription, the product to be administered, with positive patient identification, and should be carried out at the patient bedside wherever possible. 6.2.5. A systematic process should be adopted to allow independent checking, avoiding use of verbal cues or prompts. The second checker should independently check the prescription, product and patient identification. 6.2.6. Second checking may be conducted at two levels: 6.2.6.1. A basic identification check, confirming the medicine, dose and directions against those prescribed, and confirming patient identify. This is the usual check performed, and patients/carers, where appropriate, may participate in this type of check. 6.2.6.2. A ‘clinical’ second check confirming that the medicine, dose and route are clinically appropriate for the patient, as well as correctly identified. A ‘clinical’ second check can only be carried out by another competent registered health MM0000 Medicines Code Page 56 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling professional. This is suitable for high risk medicines with a wide dose range e.g. insulin, anticoagulants, opioid analgesics. 6.2.6.3. At Kettering General Hospital, second checks for preparation and administration of all Intravenous medicines, Controlled Drugs (Schedule 2), Paediatric or Cytotoxic drugs MUST be completed by another competent registered health professional. 6.2.7. In all cases the registered practitioner who initiated the prescription, preparation or administration of the medicine remains professionally responsible and accountable for the activity. 6.2.8. Where a checker has concerns about the prescription, product or patient identification they must STOP the medicine activity until clarification can be sought; where necessary this should be escalated to a more senior member of staff. 6.3. Prescription Validation and Optimisation 6.3.1. Prescription validation and optimisation involves medicines review to ensure that all prescribed medicines are safe, clinically appropriate for the patient and cost-effective, and that medicines are available in a form and at the time they are needed. 6.3.2. Medicines documented on admission should be compared with those prescribed on the prescription chart, and any deviations investigated to ensure these are clinically appropriate; reasons for change should be documented in the health record. 6.3.3. Pharmacists will routinely perform a clinical pharmacy validation of new prescriptions to ensure these are clinically appropriate for the patient, and will initial and date the prescription to demonstrate this. 6.3.4. Special emphasis will be placed on validating complex, high risk and potentially toxic medicines that require higher levels of MM0000 Medicines Code Page 57 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling monitoring; continuing medicine treatment will be reviewed as necessary. 6.3.5. Recommendations to change prescribed medicines (medicine, dose, route, frequency) will be documented on the prescription chart or in the health record in addition to verbal communication with the prescriber. 6.3.6. Pharmacy staff will annotate prescriptions for clarity, and that patient’s medicines are appropriate for use or have been ordered. 6.3.7. Minor modification of a prescription to ensure that this can be administered safely (e.g. appropriate form, route) will be documented on the prescription chart, in accordance with the pharmacy enabling policy.. 6.3.8. Prescriptions for high risk medicines should not be administered until validated by a pharmacist e.g. cytotoxic chemotherapy, including low dose methotrexate used in non-cancer indications e.g. Rheumatology. 6.3.9. Where medicines are given as a once weekly dose (such as low dose methotrexate), this MUST be clearly specified in the special directions box, on the medicine label, and in the administration record, where the administration boxes MUST be crossed out between doses that are due. MM0000 Medicines Code Page 58 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 7. ADMINISTRATION OF MEDICINES The practitioner in charge of the clinical area is responsible for ensuring that standards for medicines administration fall within the requirements of this code. The suitably qualified health professional carrying out the medicine administration check should understand the prescription and should have knowledge of the common indications, side-effects and dosages of the medicine prescribed. They should also be aware if there are any risks in handling or administration of the medicine and whether any specific equipment is required. Local procedures for handling high risk/hazardous material should be referred to where appropriate. The Healthcare professional administering the medication will be accountable for his/her practice in accordance with their professional code of conduct and standards for administration of medicines and should hold a certificate of competency from KGH in relation to the preparation and administration of parenteral therapies. 7.1. Key Principles ALWAYS… Ensure that written prescriptions are unambiguous, legible and complete (if in doubt do not proceed until you have confirmed the prescription). Check medicines prior to administration to ensure they are correct, are administered to the right patient and at the right time. Avoid delays. Witness administration of medicines where patients lack mental capacity. Wear ‘do not disturb’ tabard when undertaking medicines administration round. Confirm the identity of the patient prior to administration of a medicine. Check the patient does not have any documented allergy to the medicine. Check that medicines are in date and have been stored correctly. Ensure that medicines contained in a patient’s bedside medicines locker are correctly labelled, and only used for the current ‘named’ patient. Document the administration of a medicine on the prescription chart. MM0000 Medicines Code Page 59 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling Document the reason a medicine is omitted in the health record and take action to obtain the medicine and/or escalate to a prescriber or pharmacist. NEVER… Administer medicines that you are unfamiliar with (ALWAYS check first). Administer medicines that have NOT been authorised by a prescriber as a written patient specific prescription, or under a Patient Group Direction. Administer medicines on a verbal order (except in a medical emergency). Omit medicines unless you are authorised to do so by a prescriber or pharmacist (always document the reason clearly in the health record). Administer medicines labelled for a named patient to another patient. Sign for administering medicines prior to the patient taking the medicine. Administer unlabelled IV medicines (unless you have just drawn these up). WHERE POSSIBLE… Administer urgent medicines (e.g. IV antibiotics) as soon as possible. Involve patients in self-administering their own medicines. Regularly reassess them during their stay and support them to take their medicines safely. Avoid disturbing staff when administering medicines. Provide, or ask a member of the ward pharmacy team to provide, further information to the patient about their medicines or common side-effects. 7.2. When administering medicines the following steps should be followed 7.2.1. Check the patient name and unique identifying number on the prescription chart matches the patient’s wristband. 7.2.2. Check administration is required and has not been previously completed for this administration. 7.2.3. Check the patient does not have a known allergy or contraindications to the medicine. MM0000 Medicines Code Page 60 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 7.2.4. Check you have the right drug, right dose, right time and right indication. 7.2.4.1. Look up any unfamiliar medicines in the BNF and ensure you know the reason for giving the medicine, its usual dose and any likely side-effects. If you are in doubt as to the suitability check with the prescriber. 7.2.4.2. Check the route is prescribed and correct. 7.2.4.3. Check what is required - tablet/liquid/injection/inhaler. 7.2.4.4. Check the strength of the medicine for administration matches that prescribed. 7.2.4.5. If the medicine has required preparation, check that it has been prepared according to the SPC. 7.2.4.6. 7.2.5. Check the expiry date of the medicine has not passed. Documenting medicines administration 7.2.5.1. The practitioner must sign or initial the appropriate box on the prescription. 7.2.5.2. Where a second checker has been required they must also sign the prescription. 7.2.5.3. Where additional information is required such as batch numbers these must also be recorded on the prescription sheet. 7.3. Patients’ Own Medicines 7.3.1. Wherever possible patients’ own medicines, including Controlled Drugs, should be used during their stay in hospital, to facilitate continuity of care, self-administration (where appropriate) and to reduce waste. 7.3.2. A patient’s medicines that have been prescribed should be stored in the patient’s locked medicines cabinet on the ward, along with other named patient medicines supplied from Pharmacy for the same patient. MM0000 Medicines Code Page 61 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 7.3.2.1. Always ensure a patient’s medicines are transferred with the patient and the bedside medicine cabinet is empty, before putting in another patient’s medicines. 7.3.3. Before a patient’s own medicines can be used in the hospital they should be checked to ensure that they are clearly labelled and of sufficient quality to be safely administered. 7.3.4. Where labelled, medicines should include the following information: 7.3.4.1. The name of the patient. 7.3.4.2. Name and strength of the medicine. 7.3.4.3. Method and frequency of administration. 7.3.4.4. Date dispensed. 7.3.4.5. Name and address of supplier. 7.3.5. Where a brand name is used on the label, a member of Pharmacy staff should annotate this against the approved name on the prescription chart. 7.3.6. The directions on the label MUST match those on the prescription sheet (‘as directed’ is acceptable). If necessary these may be relabelled by Pharmacy. 7.3.7. If the medicine has no label, it must NOT be used unless it is clearly identifiable and is within its expiry date (in practice usually within a ‘blister strip’); such medicines should be relabelled by the Pharmacy before use. 7.3.8. Overall appearance of bottle, label and medicine MUST be acceptable; the container MUST be intact and clean, and the medicine must NOT show any visible sign of deterioration, and be of uniform appearance. 7.3.9. Confirmation that the medicines have been stored correctly should be checked before use. 7.3.10. Sealed compliance aids (blister packs) may be used if they are clearly labelled (or accompanied by a completed medicines administration record (MAR) sheet). Before use, staff should satisfy themselves that: MM0000 Medicines Code Page 62 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 7.3.10.1. All the medicines are prescribed. Where medicines have been stopped or changed the sealed compliance aid must NOT be used, and the medicines redispensed by Pharmacy. 7.3.10.2. Includes the patient’s name, date of birth (or alternative ID), details of the medicine and strength, and name and address of the pharmacy supplier. 7.3.10.3. The medicines appear to be in good condition, with no signs of degradation. 7.3.11. Compliance aids that are not sealed (i.e. have a removable lid covering medicine compartments) and that can be filled by relatives and carers must NOT be used. 7.3.12. Where a compliance aid is required to assist a patient to take their medicines this must be assessed by the ward pharmacy team and at least 24 hours’ notice provided before discharge. 7.3.13. Patients’ own medicines that do not meet these requirements, or are no longer required, should usually be destroyed with the patient’s permission. 7.3.13.1. Routine analgesics and other general sales medicines that are not required in hospital e.g. paracetamol may be sent home with the patient’s relatives, but patient’s prescription only medicines that have been discontinued should be returned to Pharmacy for destruction. 7.4. Delay or Omission of Medicines 7.4.1. All drugs should be given as soon as possible after administration time. Due to risk of serious patient harm, prescribing, administration and dispensing of critical medicines must never be unintentionally omitted or delayed. 7.4.1.1. Critical medicines include those used for resuscitation, anaphylaxis, antidotes for reversal of drug toxicity (e.g. naloxone), systemic therapy for prophylaxis or treatment (e.g. antimicrobials, anticoagulants), and therapy for long-term MM0000 Medicines Code Page 63 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling conditions (e.g. insulin, anticonvulsants) or symptom management (e.g. strong analgesia). 7.4.2. Delay is defined as failure to administer a medicine within 60 minutes of the specified time. Critical medicines MUST be administered within 30 minutes of prescribed time. 7.4.3. Omission is defined as failure to prescribe a critical medicine in a timely manner, failure to administer a dose before the next dose is due, or failure to administer ‘once only’ medication, within 2 hours of the prescribed time. 7.4.4. Unintentional omission or delay of any critical medicines should be reported as a medication error and recorded on DATIX. 7.4.5. Prescribers MUST inform nursing staff when a ‘stat’ dose medicine has been prescribed. 7.4.6. For non-standard treatments, the prescriber should inform the pharmacist to ensure the medicine is appropriate, available and can be supplied in a timely manner. 7.4.7. Nursing staff MUST communicate any medication delays/omissions during patient handover/transfers of care. If a dose cannot be given due to an unclear/illegible prescription, the prescriber should be contacted to re-write the prescription/clarify instructions for administration. 7.4.8. Medical, nursing and pharmacy staff should routinely review the administration section of the prescription chart as part of their daily activities and query any omitted doses so these can be followed up and appropriate action taken. 7.4.9. If a medicine is not available on the ward ensure it is ordered from Pharmacy as soon as possible. 7.4.10. If Pharmacy is not open, refer to the medicines management website to identify areas in the hospital that hold stock of the required medicine. Should the medicine still not be available contact the oncall pharmacist for advice and inform the relevant doctor to ascertain whether any other action is required. MM0000 Medicines Code Page 64 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 7.4.11. For patients who have swallowing difficulties the prescription must be reviewed by a prescriber to identify alternative routes or medications, additional information can be found in the Nil by mouth and peri-operative medicines use guideline (MMG13). 7.5. Omission codes 7.5.1. If a medicine cannot be administered to the patient as prescribed, the registered nurse responsible for administration must record the time, the appropriate omission code and their initials on the administration record of the prescription chart. 7.5.2. An omission code should only be used ONCE per medicine by a nurse and appropriate action taken. When a prescribed medicine has not been given for two or more doses or when any dose of a critical medicine has been omitted or significantly delayed, this should be followed up. If necessary, the prescriber or pharmacist must be advised and asked for further instructions. 7.5.3. A record of action(s) undertaken for dose omissions must be documented in the appropriate section of the patient’s inpatient treatment chart. 7.5.4. Where a prescribers wishes to withhold a medication(s) they should mark a ‘X’ in the administration box for each dose they want to withhold and document the reason for omission in the notes so nursing staff have clear written instructions regarding any deviations to prescribed doses. 7.5.5. Omission codes used in Kettering General Hospital are shown in the table overleaf, along with definitions, examples and appropriate action(s) to be taken. MM0000 Medicines Code Page 65 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling Omission code Definition and action to be taken 1 Patient not on ward Give dose when patient returns to ward unless next dose is due. If unsure, ask pharmacist or prescriber for advice on timing of medication. Infusion therapy should normally be continued when patients are off the ward e.g. receiving a diagnostic test. Infusion therapy should only be temporarily discontinued on written instructions of a prescriber. Nursing staff to use this code when a medicine is omitted for clinical reasons e.g. contra-indicated, adverse drug reaction. Reason for omission must be documented and the prescriber informed so alternatives can be prescribed if necessary. For long term medicines or those continued on admission, always ask if the patient has their own supply or if a relative/carer can bring in their supply from home. If not, order medication from pharmacy (contact ward services for stock replenishment or ward pharmacist for non-stock items). Speak to patient and ensure they understand what the medicine is for and any implications of not taking the dose. (Contact medical/pharmacy staff for advice if further information needed). Where the patient is fully informed and has capacity to understand their actions, this should be respected and medicine should not be administered. Medication must not be disguised in food or drink as this constitutes ‘deception’ of the patient and breaches current NMC guidance. Document the reason for refusal in the notes and inform prescriber if a patient refuses a dose of a critical medicine or refuses multiple doses. Prescribers should review the need for medication that a patient is continually refusing and amend the prescription chart as appropriate. Discuss with the prescriber or ward pharmacist, to have the prescription clarified. Doses should be given as soon as possible after the prescription has been clarified unless the next dose is due. If unsure, ask pharmacist or prescriber for advice on timing of medication. Patients who are fasting prior to a diagnostic procedure or surgery should receive all of their usual medicines as prescribed with a small amount of water unless specifically informed to withhold by prescriber/anaesthetist. Use this omission code when the patient is unable to take the dose for other reasons e.g. if patient is too drowsy or is vomiting or has severe nausea. Refer to specific Trust guidelines for ‘nil by mouth’ patients. If patient has difficulty swallowing, contact Pharmacy for advice on alternative formulations. Medicines should not be crushed for ease of administration unless approved by Pharmacy. Examples for when this code should be used are cannula not in situ/not patent; NG tube is pulled out. IV route – contact prescriber/Night Nurse Practitioner to request cannula insertion. Contact the prescriber/pharmacist to consider alternative routes if necessary. Use this omission code if the reason does not fit within the above categories. Appropriate action should be taken to ensure medicines are given as soon as clinically appropriate and possible 2 Omitted for clinical reasons 3 Medicine not available 4 Patient refused 6 Incomplete or illegible prescription 7 Nil by Mouth 8 Route not available 9 Other documented reason MM0000 Medicines Code Page 66 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 8. SELF-ADMINISTRATION OF MEDICINES Self-administration of medicines (self-medication) occurs when an inpatient administers one or more of their own medicines. This does NOT remove the Trust’s duty of care to ensure medicines are stored and taken safely. Nursing staff should assure themselves on a regular basis that the patient is taking their medicines as prescribed. 8.1. Who can Self Administer 8.1.1. If a nurse or patient feels the patient/carer is suitable for selfadministration, then a SAM assessor or administrator should assess the patient’s ability to safely self-administer their medicines using the self-administration assessment tool (Appendix 2). 8.1.2. It is important that the trained SAM assessor/administrator recognise the limitations of the assessment (as patient competence may be affected by a change in their condition or mental status). 8.2. Assessment of Patients 8.2.1. When assessing a patient, should the trained SAM assessor/ administrator in his or her professional judgment be at all unhappy for a patient to self-administer then the patient will be excluded. The reasons for exclusion should be documented in the patient’s case notes. 8.2.2. Those not suitable for self-administration include: 8.2.2.1. Patients who are medically unstable. 8.2.2.2. Patients who are confused, disorientated or have a significant neurological deficit. 8.2.2.3. Patients who refuse to participate in the self-administration of medicines scheme. 8.2.2.4. Patients on a mental health section. 8.2.2.5. Patients expressing suicidal/self-harm feelings. 8.2.2.6. Patients known to have a current drug/alcohol abuse problem. MM0000 Medicines Code Page 67 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 8.2.3. Patients with a history of drug/alcohol abuse (but not a current issue) should not necessarily be excluded. Self-medication for these patients should be discussed with the medical team. 8.2.4. The SAM assessment form should be filed in the patient’s health record. 8.2.5. Patient consent should be obtained and documented using the form in Appendix 3. 8.2.6. Patients should be assigned the appropriate level (see section 6.2), and this should be re-assessed daily as the patient’s condition may change. 8.2.7. The SAM assessor or administrator must assess the patient’s ability to manage their medicines daily in line with the Mental Capacity Act 2005. 8.2.8. Patient’s own medicines that are suitable for use, or medicines that have been dispensed from the hospital, may be used for selfadministration. 8.2.9. All medicines used for self-administration MUST be clearly labelled. 8.2.10. If the prescription is altered the patient should be advised of the change and relevant medicines information provided. It may be necessary to re-label medicines and change the level of selfadministration for a period. 8.2.11. All medicines for self-administration MUST be locked in the individual patient’s bedside medicine cabinet. 8.2.12. When a patient is self-administering his or her own medicines, a record MUST be made in the administration section of the prescription sheet. 8.2.13. Nursing staff should document on the inpatient treatment chart that the patient is self-administering medications using the code 5. 8.2.14. On transfer or discharge, the patient’s medicines MUST be removed from the medicine cabinet and the key to the cabinet retained on the ward. MM0000 Medicines Code Page 68 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 8.2.15. Day case and outpatients can continue to take their medicines as they would at home without an assessment, as long as there is no clinical reason not to do so. 8.2.16. Patients self-administering their medicines should be given an information leaflet about the scheme and a ‘medicines Information card’ to record relevant information about their medicines. MM0000 Medicines Code Page 69 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 9. SUPPLY OF MEDICINES TO P ATIENTS 9.1. Key Principles 9.1.1. POMs (Prescription only Medicines) MUST only be supplied against a written prescription or PGD. 9.1.2. PGDs (Patient Group Directions) MUST be approved by the Medicines Management Group. 9.1.3. Only staff authorised in law may supply medicines against a PGD. 9.1.4. Supply and/or administration MUST be fully documented. 9.1.5. Prescriptions that are rewritten or transcribed MUST be authorised. 9.2. Key Standards 9.2.1. All POMs are supplied against a written prescription or PGD. 9.2.2. An approved PGD exists for all medicines supplied under PGD. 9.2.3. A training record is retained for staff authorised to use PGDs. 9.3. General Procedures 9.3.1. Prescription only Medicines are only supplied or administered against a valid written prescription (authorised by a registered medical or non-medical prescriber), or against an authorised Patient Group Direction. 9.3.2. Prescription only medicines are only supplied under the supervision of a registered doctor, nurse, midwife or pharmacist. 9.3.3. Stock medicines are only used to administer doses to patients while in hospital and must NOT be supplied to individual patients on discharge. 9.3.4. Medicines which the patient is to take home MUST be clearly labelled with the patient’s name and the directions for use. 9.3.5. Verbal messages must NOT be used to order or supply medicines except in medical emergencies (see section 4.4). 9.3.6. The sale and supply of medicines is subject to statutory requirements of the Medicines Act and statutory instruments. MM0000 Medicines Code Page 70 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 10. DISPOSAL OF PHARMACEUTICAL WASTE Pharmaceutical waste is classed as ‘special waste’. Healthcare professionals must never dispose of medicines into the mains sewerage system i.e. sink or toilet. 10.1. Key Principles 10.1.1. It must be disposed of by incineration, in approved containers, at high degree temperatures in order to completely destroy all potent substances. 10.1.2. Prosecution will occur if such waste is consigned as anything other than ‘special waste’ e.g. it is discovered in landfill tips, and it can be traced back to the user. 10.1.3. Cytotoxic and cytostatic medicines are classified as hazardous waste and must be segregated from other pharmaceutical waste and placed in the correct hazardous waste bin please refer to the Trust Cytotoxic Chemotherapy Policy MM25. 10.1.4. Disposal of controlled drugs is subject to special legislative controls and procedures please refer to section12.17. 10.1.5. Disposal of pharmaceutical waste must be in accordance with local waste management policy. Refer to the policy for further information. 10.1.6. A consignment note must accompany pharmaceutical waste removed for incineration. 10.2. General Procedures 10.2.1. Empty Containers 10.2.1.1. Empty medicine containers must be disposed of at ward / department level. These should be placed in the appropriate glass, plastic or household waste bin. 10.2.1.2. Liquid bottles must be rinsed with water, before placing into the glass bin. 10.2.1.3. Ensure that patient names are obliterated from empty containers before disposal MM0000 Medicines Code Page 71 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 10.2.2. Tablets and Capsules 10.2.2.1. Any table or capsule removed from its original packaging and not administered to the patient must be destroyed by placing it in the yellow sharps bin. 10.2.2.2. Full and part used boxes of medicines, including loose blister strips should be returned to pharmacy in the green Pharmacy bins for processing. 10.2.3. Glass vials and Pre-filled syringes 10.2.3.1. For part used ampoules the remaining drug should be emptied into the yellow sharps bin before disposing of the glass container in the same way. 10.2.3.2. Empty glass vials should be placed in the non-hazardous pharmaceutical waste bin (blue). 10.2.3.3. Part used vials or pre-filled syringe must be placed directly in the yellow sharps bin. 10.2.4. Mixtures and syrups 10.2.4.1. Full and part used bottles of syrups and mixtures should be returned to pharmacy in the green Pharmacy bin for processing. 10.2.5. Medicated plasters and patches 10.2.5.1. Patches or plasters which remain in their outer container should be returned to pharmacy in the green Pharmacy bin for processing 10.2.5.2. Plasters or patches which have been removed from the patient should be folded in half so any active surface is adhered to itself and place in the yellow sharps bin. 10.2.6. Inhalers and aerosols 10.2.6.1. Full and part used containers should be returned to pharmacy in the green Pharmacy bin for processing 10.2.7. Parenteral fluids and solutions for irrigation 10.2.7.1. Part used containers of simple fluids (sodium chloride, potassium containing solutions, hartmanns and glucose) should be emptied into a foul sewer and the outer container disposed of in the yellow sharps bin. MM0000 Medicines Code Page 72 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 10.2.7.2. Where a pharmaceutically active substance has been added to a fluid, the remainder should be disposed of in the yellow sharps bin. 10.2.7.3. Full containers should be returned to pharmacy in the green Pharmacy bin for processing. MM0000 Medicines Code Page 73 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 11. P ATIENT GROUP DIRECTIONS The preferred way for patients to receive the medicines they need is for a prescriber to provide care for an individual patient. PGDs provide a legal framework that allows the supply and/or administration of a specified medicine(s), by named, authorised, registered health professionals, to a predefined group of patients needing prophylaxis or treatment for a condition described in the PGD, without the need for a prescription or an instruction from a prescriber. Using a PGD is not a form of prescribing. Supplying and/or administering medicines under PGDs should be reserved for situations in which this offers an advantage for patient care, without compromising patient safety. The purpose of using a PGD is to: deliver effective patient care that is appropriate in a pre-defined clinical situation, without compromising patient safety. offer a significant advantage to patient care by improving access to appropriate medicines. provide equity in the availability and quality of services when other options for supplying and/or administering medicines are not available. provide a safe legal framework to protect patients. reduce delays in treatment. maximise the use of the skills of a range of health professionals. 11.1. Key Principles 11.1.1. The supply and/or administration of prescription-only medicines (POMs) to patients within a PDG framework MUST follow an assessment of patient need by an individual registered health professional who is authorised to perform such an activity within KGH. 11.1.2. Only named registered professions are authorised to supply medicines under PGD, these currently include nurses; midwives; MM0000 Medicines Code Page 74 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling health visitors; optometrists; pharmacists; chiropodists; radiographers; orthoptists; physiotherapists; ambulance paramedics; dieticians; occupational therapists; speech and language therapists; prosthetists; orthotists; dental hygienists and dental therapists. 11.1.3. PGDs are subject to legislation and the content must be prepared in an approved format and authorised by a senior medical practitioner, the Chief Pharmacist and approved by the Trust Medicines Management Group (MMC). 11.1.4. A PGD MUST include the following information: 11.1.4.1. Details of the condition and situation for which the PGD applies. 11.1.4.2. Details of any contra-indications or other exclusion criteria. 11.1.4.3. A description of the treatment available under the PGD. 11.1.4.4. Details of the staff authorised to take responsibility under the PGD. 11.1.4.5. The management and monitoring of the PGD including an annual audit of its use. 11.2. Development, Authorisation and Review of PGDs 11.2.1. Recommendations for good practice have been developed by the NICE Guidance Development Group (GDG), using relevant legislation and guidance as the foundation for good practice. 11.2.2. The procedure for considering the need for, and obtaining agreement to develop a PGD is described in Appendix 4. The template PGD Proposal Form (Appendix 5) must be completed and submitted to support each application. 11.2.3. The procedure for developing and submitting a PGD for approval and authorisation is described in Appendix 6. The template CBU preapproval Form (Appendix 7) must be completed and submitted to support each application. MM0000 Medicines Code Page 75 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 11.3. Using a PGD 11.3.1. Individual registered staff who supply or administer medicines against a PGD MUST be aware of the policy and procedures pertaining to PGDs. 11.3.2. The Appointed Practitioner in Charge of each ward or department is responsible for ensuring that medicines are administered against a written prescription or PGD, and for maintaining a record of signatures authorising individual registered staff to use the PGD. 11.3.3. A record of administration under PGD MUST be entered on the patient’s prescription chart or health records as described in the individual PGD and signed by the Designated Practitioner supplying or administering the medicines under the PGD. 11.3.4. Medicines must be supplied directly by the registered practitioner at the time they are using a PGD, and cannot be delegated to someone else. 11.3.5. The Appointed Practitioner in Charge should review PGDs annually to ensure these accurately reflect practice and are being used appropriately. 11.3.6. Staff using PGDs or protocols should have undertaken appropriate training to demonstrate understanding and competence and will at all times work within their scope of practice, professional guidance and Trust policy and procedures. MM0000 Medicines Code Page 76 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 12. CONTROLLED DRUGS The Misuse of Drugs Act, 1971 controls certain classes of dangerous drugs, which are listed and known as “Controlled Drugs”. Its main purpose is to prevent the misuse of these drugs by imposing a total ban on the possession, supply, manufacture or importation of Controlled Drugs, except as allowed by regulations. The use of Controlled Drugs in medicine is regulated by the Misuse of Drugs Regulations, 2001 (as amended). Separate regulations deal with the safe custody of Controlled Drugs and their supply to substance misusers. The 2001 Regulations set out a number of schedules, which classify Controlled Drugs (CDs) according to different levels of control. Storage and security requirements may be increased locally at the discretion and direction of the Nursing Management in discussion with the Accountable Officer or their nominated deputy. 12.1. Key Principles 12.1.1. Controlled drugs are an important therapeutic intervention e.g. for pain management, and, as such, must be readily accessible to patients who require strong analgesia. 12.1.2. Controlled drugs are subject to special legislative controls because there is a potential for them to be abused or diverted, causing possible harm. 12.1.3. Designated healthcare staff are authorised in law, to be in possession of controlled drugs for the purposes of supply, administration or disposal in accordance with the above principles 12.1.4. All preparation, administration and disposal of schedule 2 CDs MUST be directly witnessed by another register Practitioner. 12.1.5. Systematic documentation and checks MUST be maintained to ensure the secure management of controlled drugs and demonstrate this to the Accountable Officer. MM0000 Medicines Code Page 77 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 12.1.6. All incidents MUST be investigated and reported to the Accountable Officer or their deputy, and will be referred to the CD Intelligence network as appropriate. 12.1.7. Healthcare staff of all grades involved in the storage, prescribing, supply, administration and disposal of CDs MUST adhere to this policy. 12.1.8. Failure to comply with these good practice standards and legislative requirements could result in disciplinary action and / or criminal prosecution. 12.2. Key Standards 12.2.1. All Schedule 2 and some Schedule 3 CDs are locked in a CD cupboard 12.2.2. CDs subject to safe custody requirements must be physically checked every day against register balances 12.2.3. Prescriptions for CDs are prescribed on the correct KGH prescribing stationary and comply with handwriting requirements 12.2.4. Preparation and Administration of CDs that are subject to safe custody requirements must be checked by a second registered practitioner against a valid prescription 12.2.5. Quarterly checks of the safe and secure management of CDs are carried out by Pharmacy staff 12.2.6. All unresolved CD errors are reported on datix incident report and fully investigated 12.3. Accountability for CDs 12.3.1. The Accountable Officer (Chief Pharmacist) is responsible for the safe and secure management of CDs throughout the Trust, under statutory provisions of the Health Act 2006. 12.3.2. The appointed nurse, midwife or Operating Department Practitioner (ODP) in overall charge of a ward or department is responsible for the safe and appropriate management CDs in that area. MM0000 Medicines Code Page 78 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 12.3.3. The designated nurse, midwife or ODP in charge can delegate control of access (i.e. key-holding) to the CD cupboard to another Assigned Practitioner, such as a registered nurse or ODP. However, legal responsibility remains with the appointed nurse, midwife or ODP in charge. 12.3.4. All designated staff involved with the management of CDs (prescribing, ordering, preparation, administration and disposal) MUST submit a copy of their signature, area of work and professional registration number to pharmacy for confidential use in checking and validating written records. 12.4. Ordering of CDs 12.4.1. Each ward or department will hold a stock of CDs agreed by the designated nurse, midwife or ODP with the CBU Lead Pharmacist. The stock list will reflect current usage, whilst minimising risks associated with storage of multiple products and strengths. The stock list will define drug, form, strength and quantity held. 12.4.2. CDs may be ‘topped up’ against the defined stock list for each ward and department by a pharmacist or pharmacy technician, who is responsible for checking the stock balances in the Ward CD register against the levels in the agreed stock list. 12.4.3. Only one controlled drugs order book should be in use in a ward/clinical area at any one time, for requisitioning controlled drugs from pharmacy. 12.4.4. Under no circumstances can controlled drugs be requisitioned from another clinical area. Orders for controlled drugs must be written in ink in the controlled drugs order book and must include the following information: 12.4.4.1. hospital and ward/department 12.4.4.2. name of CD 12.4.4.3. strength or concentration 12.4.4.4. form (e.g. tablets, capsules, injection, ampoules) 12.4.4.5. total quantity required MM0000 Medicines Code Page 79 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 12.4.4.6. signature 12.4.4.7. printed name 12.4.4.8. designation 12.4.4.9. date 12.4.5. CD requisitions MUST be written in the CD ward order book and must be signed by a registered Nurse, Midwife or ODP who is an authorised CD signatory. 12.4.6. In certain circumstances, CD requisitions, for items other than those on the CD stock list, may be prepared by a pharmacist or pharmacy technician but MUST be signed by a registered Nurse, Midwife or ODP who is an authorised CD signatory. 12.4.7. Methadone for inpatient use is to be labelled with patient’s name. Other CDs dispensed for in-patient use only are labelled ‘Temporary Stock’ to differentiate these from patient’s own drugs / other stock items. 12.4.8. Stock CDs or those issued for inpatient use only must NEVER be given to patients on discharge. 12.4.9. CDs that may be taken home by the patient, must be supplied against a valid discharge or outpatient prescription [see section 12.13.2 on Prescribing CDs for discharge and section 12.13.3 Prescribing CDs for outpatients]. 12.4.10. A copy of the signature of each Designated Practitioner for the purposes of ordering CDs must be available in the pharmacy department for verification, and checked prior to the supply being made. 12.5. Receipt of CDs 12.5.1. Receipt of controlled drugs on to a ward/clinical area must be by a Designated Practitioner. 12.5.2. The Designated Practitioner must check that the numbered seal on the delivery bag is intact and the bag has not been tampered with. The entire contents of the delivery bag must immediately be MM0000 Medicines Code Page 80 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling checked, and signed as received, against the entry in the controlled drugs order book. 12.5.3. Although the quantity received should be checked, it is unnecessary to break a tamper evident seal on a pack in order to check the quantity. 12.5.4. Once checked, the registered staff member must immediately enter the received controlled drug(s) on to the appropriate page(s) of the controlled drugs register. 12.5.5. Any discrepancy should immediately be reported to Pharmacy. 12.6. Obtaining controlled drugs out-of-hours 12.6.1. It is vital to maintain a robust audit trail for controlled drugs. 12.6.2. During Pharmacy opening hours, controlled drugs must always be ordered from Pharmacy. 12.6.3. In exceptional circumstances when medication is required urgently and Pharmacy is closed, controlled drugs sufficient for a single dose only may be obtained from another ward. The registered staff member must contact other areas in the following order: - Another ward in their own CBU - Another ward in a different CBU - The Intensive Care Unit 12.6.4. The registered staff member must take the patient’s prescription chart to the area holding the required controlled drug and, with the assistance of the controlled drugs keyholder in that area, prepare and record a single dose for the patient. On return to the patient’s ward, an independent check must be obtained from a second registered nurse/midwife to ensure the controlled drug dose is administered to the correct patient. For all other supplies of controlled drugs, when Pharmacy is closed, the emergency duty Pharmacist should be contacted. MM0000 Medicines Code Page 81 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 12.7. Transport of CDs 12.7.1. A record of transport is required for Controlled Drugs. This should include signatures from the Assigned Practitioner issuing the CD, transporting the CD and receiving the CD in the ward or department. 12.7.2. CDs subject to safe custody requirements MUST be transported in a security sealed bag and Designated Practitioners are required to sign the duplicate copy of the requisition when receiving this onto the ward. These CDs must NOT be left unaccompanied and MUST be handed directly to a Designated Practitioner for immediate storage in the CD cupboard. 12.7.3. Where CDs are collected from the pharmacy department, an assigned practitioner will be required to sign for a sealed bag with numbered tag. 12.7.4. Positive ID and signature checks must be undertaken when Controlled Drugs are issued directly by Pharmacy to Trust staff. 12.7.5. Where an outpatient (or their relative or carer) collects CDs from the pharmacy department, they are required to show proof of identity. Where a healthcare professional, acting in their professional capacity on behalf of the patient, collects CDs, they MUST show proof of identity, and provide details of their name and address / place of work. 12.8. Transfer of CDs 12.8.1. A securely sealed CD transfer bag must be used to transport patient’s own controlled drugs between wards, and when they are discharged on transport e.g. by ambulance, and are unable to look after their medicines. 12.8.2. Where a patient is given their CDs directly on discharge and is able to manage these safely and securely, then these may be placed with other medicines in the patient’s medicines bag, which should not be left unattended and stored safely at all times. MM0000 Medicines Code Page 82 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 12.8.3. When a sealed CD transfer bag is used, the serial number must be recorded in the issuing CD register and patient’s name, ward, hospital (unit) number, and date of transfer should be completed on the tear-off section and signed by the Designated Practitioner issuing the CDs. 12.8.4. The Assigned practitioner (e.g. Hospital porter, Ambulance crew) must sign for receiving the sealed bag and transport this intact to the receiving ward or patient’s home. 12.8.5. The Designated Practitioner receiving the patient, checks the bag is intact, signs the tear-off record on the CD transfer bag and records the CDs and serial number in the ward CD register. The tear-off record is retained by the person transporting the patient, as proof of delivery. 12.8.6. Where a patient is transferred to a residential or domiciliary setting, the patient’s carer or adult representative receiving the sealed CD transfer bag, signs the tear–off record, confirming the bag is intact, and returns this to the person transporting the patient, as proof of delivery. 12.9. Storage and Security of CDs 12.9.1. Wards, Theatres or Departments must NOT store Controlled Drugs unless there is an Appointed Practitioner in Charge responsible for the secure storage and safe use of the Controlled Drugs. 12.9.2. Controlled drugs (including patients’ own controlled drugs) must be stored in a cupboard which conforms to British Standard reference BS2881, or in a cupboard individually approved in advance by Pharmacy. All cupboards for the storage of CDs MUST be secured to a wall or the floor. 12.9.3. The cupboard must be locked when not in active use. Access to the cupboard must be restricted to those staff who can lawfully be in possession of a controlled drug (e.g. registered nurse / midwife / ODP, pharmacist, doctor, or a person acting under their direct authority, e.g. pharmacy technician). MM0000 Medicines Code Page 83 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 12.9.4. Locks for CD cupboards must NOT be common to any other lock in the hospital. Two sets of keys should be held, one in use carried by the Designated Practitioner, and a spare set locked away in a secure key cabinet with access limited to the appointed nurse, midwife, or ODP in charge of an area. A third set will be retained securely within the Pharmacy Department. 12.9.5. An accurate and current record of the named keyholder must be maintained and updated at each shift change or other handover period. The controlled drug cupboard keys must be kept separate (or easily separable) from other drug cupboard keys. 12.9.6. Keys may be handed to a staff member authorised to access the controlled drug cupboard (as outlined above) but must be returned to the authorised keyholder immediately after use. 12.9.7. The controlled drug cupboard must only be used to store controlled drugs and medicines to which special arrangements are attached, e.g. midazolam, ketamine. 12.9.8. Controlled Drug Order Books and Registers must be kept either in the controlled drug cupboard or in an alternative secure storage area. 12.9.9. During any temporary closure of a ward/clinical area, arrangements must be made in advance with Pharmacy to cover security of controlled drug cupboard keys, and security arrangements for controlled drugs, either on the existing ward/clinical area or in an alternative location, during the period of the closure. 12.10. Storage and security of TTAs which include a controlled drug 12.10.1. There is no requirement to store in the controlled drug cupboard, or record in the controlled drugs register, a controlled drug supplied to a patient as part of their discharge medication (TTA), provided that the patient is being discharged immediately. 12.10.2. However, if there is any delay between the controlled drug TTA arriving on the ward and the patient leaving the ward, the nursing staff must store the dispensed controlled drug in the controlled drug MM0000 Medicines Code Page 84 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling cupboard. This must be appropriately recorded in the patient’s own controlled drugs register. 12.10.3. At the point of discharge, the controlled drug must be removed from the controlled drug cupboard and the removal recorded in the patient’s own controlled drugs register. 12.11. Loss of controlled drug cupboard keys/replacement controlled drugs cupboard lock. 12.11.1. If CD keys go missing, every effort should be made to find or retrieve the keys, as a matter of urgency e.g. by contacting staff who have just gone off duty. 12.11.2. If the keys cannot be found the keyholder must inform the Nurse in Charge, CBU Lead Nurse and the Controlled Drug Accountable Officer (CDAO) and Local Security Management Specialist (LSMS) as soon as possible. (If CDAO is unavailable, notify the Deputy Chief Pharmacist for QiPPs or Clinical Excellence during opening hours. For Out of hours notify Emergency Duty Pharmacist.) who will advise any action to secure the CD stock and arrange supply of CDs for urgent clinical use. 12.11.3. Out of Hours, a dose may be provided from another ward, as long as this is fully documented in that ward’s CD register for the specific patient and their location, and in accordance with a valid prescription for that patient. 12.11.4. Replacement of locks MUST only be on the authority of the CDAO (Chief Pharmacist) and the LSMS. Complete the ‘request form for replacement of a key or lock’ (Appendix 8). (If CDAO is unavailable, the Deputy Chief Pharmacist for QiPPs or Clinical Excellence during opening hours or the oncall Pharmacist out of hours have delegated authority to authorise this). 12.11.5. Both Pharmacy and Estates will maintain a log of all requests to include date, reason for request, nurse in charge making request and name of person/s authorising the replacement. MM0000 Medicines Code Page 85 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 12.11.6. Where access is restricted due to missing or lost keys a datix incident report MUST be completed and forwarded to the CDAO. 12.11.7. Loss or theft of any controlled stationery which may be used to order CDs should be reported immediately to the Responsible Pharmacist and Accountable Officer. This includes ward CD order books, registers, discharge and outpatient prescription forms, which MUST be stored securely when not in use to prevent fraudulent use. 12.12. Patients’ Own CDs 12.12.1. The Trust encourages the use of patient’s own medicines that are suitable for use, including controlled drugs. These remain the property of the patient, but their secure storage is the responsibility of the Trust. 12.12.2. Medicines labelled for a specific named patient must NOT be used to treat another patient, and MUST be stored separately from stock medicines. 12.12.3. Patients’ own CDs that are not prescribed during their stay should not routinely be stored on the ward, but sent to pharmacy for destruction, or returned home with a relative, where appropriate [see section Return and Disposal]. 12.12.4. For patients who have brought their own supply of CDs into hospital, a record of the patient’s own CDs retained on the ward MUST be entered into the ward Patient’s Own CD register and a record of doses administered and running balance kept [see section Documentation and Record Keeping]. 12.13. Prescribing of CDs The following registered staff are authorised to prescribe controlled drugs: Doctors (FY1) can prescribe controlled drugs for inpatients and for TTAs, but cannot prescribe controlled drugs for out-patients. Supplementary prescribers where the controlled drug is included in the clinical management plan. MM0000 Medicines Code Page 86 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling Independent non-medical prescribers can prescribe some controlled drugs within their competence. Controlled drugs cannot be supplied against a prescription signed by a prescriber whose signature is not already held in Pharmacy records. 12.13.1. Prescribing controlled drugs for in-patients There are no special requirements for prescribing controlled drugs for in-patients. Guidance provided in the Trust’s Prescribing Medicines Policy should be followed at all times. 12.13.2. Prescribing controlled drugs for patients to take home (TTAs) 12.13.2.1. Controlled drug TTAs must be prescribed on the standard Controlled Drugs TTA prescription form (Appendix 9). 12.13.2.2. Where different strengths or forms of the same controlled drug are required, these should be treated as different controlled drugs. 12.13.2.3. Prescriptions should be written for a maximum of 28 days’ supply. 12.13.2.4. Complete the minimum information required, detailed below, for each separate controlled drug: Patient name Home address Hospital number (a patient label is acceptable but must be signed by the prescriber, across the edge of the label and TTA form) Form (e.g. tablets, patch, liquid) even if only one form Drug name Drug strength, including the units of the strength Quantity, in both words and figures Drug dose and frequency (if prescribed ‘when required’ eg for breakthrough pain, a minimum interval for administration MM0000 Medicines Code Page 87 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling should be specified and a maximum total quantity to be administered in 24 hours). 12.13.2.5. To authorise the prescription the prescriber must sign and date the CD TTA prescription in the field provided, using their usual signature, which must match the signature held in Pharmacy. Whilst not a legal requirement, it may be helpful to include a bleep number/contact number. 12.13.3. Prescribing controlled drugs for out-patients 12.13.3.1. Prescribing controlled drugs for out-patients follows the same process as outlined above for the prescribing of controlled drugs as TTAs, except that controlled drugs for out-patients must be prescribed using one of the following prescribing documents: 12.13.3.2. F126 Out-Patient Prescription and Dietary Prescription Card. 12.13.3.3. KGH Controlled Drug Prescription Form for hospital dispensing only. 12.13.4. Doctors prescribing controlled drugs for themselves or someone close to them. Guidance issued by the GMC states: 12.13.4.1. Doctors should, wherever possible, avoid treating themselves or anyone with whom they have a close personal relationship and should be registered with a GP outside their family. 12.13.4.2. Controlled drugs can present particular problems, occasionally resulting in a loss of objectivity leading to drug misuse and misconduct. 12.13.4.3. Doctors should not prescribe a controlled drug for themselves or someone close to them unless: 12.13.4.3.1. No other person with the legal right to prescribe is available to assess the patient's clinical condition and to prescribe without a delay which would put the patient's life or health at risk, or cause the patient unacceptable pain, and MM0000 Medicines Code Page 88 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 12.13.4.3.2. That treatment is immediately necessary to: Save life Avoid serious deterioration in the patient's health, or Alleviate otherwise uncontrollable pain. 12.13.4.4. The Trust foresees no situation within the hospital environment where these are likely to occur, therefore doctors are not allowed to prescribe controlled drugs for themselves or someone close on FP10 forms. 12.13.4.5. If a pharmacist or doctor becomes aware of a practitioner prescribing controlled drugs for family, friends, or themselves, they must discuss the circumstances directly with the prescriber. 12.13.4.6. Prescribers who have issued such prescriptions should cooperate with enquiries made by other healthcare professionals who wish to discuss the treatment. 12.13.4.7. Where there remains any concern about a prescription, the person with the concern should make the Trust Accountable Officer and Medical Director aware of it as soon as possible. Ref: GMC Guidance for Doctors - Prescribing Guidance - Need and Objectivity: Prescribing guidance: Need and objectivity. 12.13.5. Prescribing private prescriptions for controlled drugs 12.13.5.1. Kettering General Hospital Trust do not hold FP10cd forms and hospital prescribers may not prescribe controlled drugs for private patients. 12.13.5.2. The Pharmacy Department at KGHFT do not dispense private prescriptions. 12.14. Preparation and Administration of CDs Kettering General Hospital NHS Foundation Trust sets a standard of two registered healthcare practitioners being involved in the administration of controlled drugs (except in an emergency situation) so that an independent check is made on administration. MM0000 Medicines Code Page 89 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 12.14.1. Controlled drugs can only be administered against a legal prescription (see section 4.1) by an authorised member of staff (see section 7 above). 12.14.2. The authorised staff member must be witnessed throughout the selection, preparation and administration process. 12.14.3. Destruction and disposal of any surplus controlled drug following administration, eg a part used ampoule, must also be witnessed. 12.14.4. An immediate record of the administration of the controlled drug must be made in the controlled drugs register. This entry must be made in indelible ink, must be chronological and must be countersigned by the witness. The following information must be included: date and time of administration name of patient quantity administered signature of person administering dose signature of witness to administration new stock balance 12.14.5. If a part vial or ampoule is administered, the amount administered and the amount destroyed must both be recorded in the controlled drug register. 12.14.6. In Critical Care, Theatre areas and Emergency Departments it may not always be possible to directly witness administration, where doses are administered incrementally by medical staff. Disposal of any remaining dose or the syringe, vial or ampoule MUST be witnessed (see section 12.15). 12.14.7. Failure to witness the administration and/or disposal of Controlled Drugs is considered a breach of procedure and could result in disciplinary action or criminal prosecution if evidence of theft or diversion occurs. Such incidents may be reported to the professional regulator. MM0000 Medicines Code Page 90 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 12.14.8. CDs will ONLY be booked out of the ward CD register for an individual patient, prepared and administered in accordance with the written authorisation of a qualified medical or non-medical prescriber [see section on record keeping]. 12.14.9. Registered healthcare practitioners may administer a CD as long as they are acting in accordance with the written directions of a registered prescriber. 12.14.10. If administration of a controlled drug given by infusion is not completed, the remainder should be destroyed on the ward/clinical area and a record made on the appropriate page of the controlled drugs register. (See section 12.17 disposal of controlled drugs on wards/clinical areas). If, for any reason, an individual dose of a prepared controlled drug cannot be administered, it should be immediately destroyed and an entry made in the controlled drugs register by the practitioner and witness. 12.14.10.1. Residual volumes of patient controlled analgesia (PCAs), maybe destroyed on the ward were the PCA is stopped which may not be the theatre were prepared and administration commenced. An appropriate record of witnessed destruction should be made in the ward CD register. 12.14.11. The reason for non-administration must be recorded (see section 7.5). 12.14.12. If any error is made in the controlled drugs register, the incorrect entry must be bracketed, leaving the original entry clearly legible. This must be signed, dated and witnessed by two registered members of staff. The reason for the error must be recorded. 12.14.13. Liquid paper correction fluid (eg Tippex®) must NEVER be used. 12.15. CDs issued directly to Medical Staff 12.15.1. In Critical Care, Theatre areas and the Emergency Department, CDs are routinely issued to medical staff who then administer these to a named patient in accordance with a written prescription. A bespoke MM0000 Medicines Code Page 91 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling CD register has been provided to record such issues, clearly identify accountability of staff involved and document return or destruction of remaining CDs. 12.15.2. It is the responsibility of the Designated Nurse or Operating Department Practitioner (ODP), when issuing a CD, to document the name of the Doctor / Anaesthetist and, where possible, the patient name, in section B of the CD register 12.15.3. It is recognised that administration cannot be routinely witnessed by a second practitioner in critical care areas. A record of administration should be recorded by medical staff and compared with the quantity remaining at the end of each patient procedure. 12.15.4. As staff may change over during a procedure or theatre session, the medical staff who complete administration MUST confirm the amount administered or to be destroyed, at the end of each patient procedure, and sign for this in section C. 12.15.5. A registered Nurse or ODP MUST witness the destruction of a partused ampoule or syringe containing Controlled Drug or return of an unused ampoule back into stock, and sign for this in section D. 12.15.6. Part-used quantities must be rendered irretrievable in accordance with the section on Returns and Disposal of CDs. 12.15.7. Disposal of ampoules that are found broken, or are accidentally dropped or spilled during a procedure MUST be documented AND witnessed. 12.15.8. Witnessed destruction can be done at the end of each patient procedure but MUST be completed at the end of each theatre session. 12.15.9. The stock balance must be checked and witnessed at the end of each theatre session, and at minimum once daily, and signed for in section E. 12.15.10. CDs should be issued for use in ONE patient only. National guidelines on Controlled Drugs discourage the practice of sharing an ampoule amongst several patients. MM0000 Medicines Code Page 92 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 12.15.11. Quantities administered and/or wasted MUST be clearly documented and signed by the Anaesthetist, at the end of each patient procedure, and signed for in section C. 12.15.12. Any part-used syringes or ampoules MUST be destroyed at the end of the theatre session, and witnessed and documented in section D of the register, before medical staff leave the theatre area or department. 12.16. Documentation and Record Keeping for CDs 12.16.1. Each ward or department that holds supplies of CDs MUST keep a record of schedule 2 CDs received and administered in a standard bound ward CD register. Separate registers are held for ward stock, syringe drivers, patients’ own CDs and CDs used in theatre or emergency departments; registers are supplied from pharmacy on written request via a requisition in the ward CD order book. 12.16.2. Ward and department CD registers MUST be kept locked away when not in use, either in the CD cupboard or another locked cupboard or drawer, to which access is restricted to the Designated Practitioner, who holds the CD keys. 12.16.3. The ward CD register has separate pages for each drug, form and strength, so that a running balance can be easily recorded. Entries should be made in chronological order, in indelible ink. 12.16.4. Non-stock items received only for administration to an individual inpatient should be entered on the appropriate page for that drug, form and strength, in the ward stock register. 12.16.5. All entries MUST be signed by the designated nurse, midwife or ODP and should be witnessed preferably by second registered nurse, midwife or ODP. If a second registered nurse, midwife or ODP is not available, then the transaction can be witnessed by another registered professional (e.g. doctor, pharmacist, pharmacy technician). MM0000 Medicines Code Page 93 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 12.16.6. On reaching the end of a page in the ward CD register, the balance should be transferred to another page. The new page number should be added to the bottom of the finished page and the index updated. As a matter of good practice this transfer may be witnessed. 12.16.7. If a mistake is made it should be bracketed so that the original entry is still clearly legible, and corrections made. These should be signed, dated and witnessed by a second registered nurse, midwife or other registered professional. 12.16.8. On receipt of all schedule 2 CDs, the following details should be recorded on the appropriate page in the relevant ward CD register: Date of entry Serial number of requisition Quantity received Name/signature of nurse/authorised person making entry Name/signature of witness Balance in stock [see sections on checking and reporting] 12.16.9. When recording CDs received from pharmacy, the number of units received should be recorded in words not figures (e.g. ten, not 10) to reduce the chance of entries being altered. 12.16.10. After every administration, the physical stock balance of an individual preparation should be confirmed to be correct and the balance recorded in the ward or department CD register. The entry should be signed and dated [see section 12.18 on checking and reporting]. 12.16.11. On administration of all schedule 2 CDs, the following details should be recorded on the appropriate page in the relevant ward CD register: MM0000 Medicines Code Page 94 of 113 Date and time when dose administered Name of patient Quantity administered Chairman: Graham Foster JP Chief Executive: David Sissling Name/signature of Designated Practitioner who administered the dose Name/signature of witness Balance in stock [see sections on checking and reporting] 12.16.12. Any medicine prepared and not used, or only partly used, MUST be destroyed in the presence of a second registered practitioner. An entry MUST be made in the ward CD register and signed by both parties [see next section on returns and disposal]. 12.16.13. CD records, including ward requisitions books and registers MUST be kept for a period of at least two years from the last entry being made. They should be securely stored in the ward or department, and made available in the event of an investigation. 12.17. Disposal or return of CDS 12.17.1. Expired controlled drug stock 12.17.1.1. Wherever possible, stock rotation should be used to avoid expiry dates being reached before use. However, if stock passes its expiry date, it should be returned to Pharmacy together with a completed Controlled Drug Returns/Destruction form (Appendix 10). 12.17.1.2. Expired stocks of controlled drugs must not be destroyed on the ward/clinical area, but placed in an ‘out of date CD return bag’ and returned to the CD cupboard for collection. 12.17.1.3. Expired controlled drug stock can be handed to a pharmacist or pharmacy technician for return to Pharmacy. 12.17.1.4. On receipt in Pharmacy, Section B of the Controlled Drug Returns/Destruction form will be completed and a copy returned to the relevant ward/clinical area. This document must be retained in a safe place (Appendix 10) 12.17.2. Disposal and destruction of patients’ own controlled drugs (see also Section 10.) MM0000 Medicines Code Page 95 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 12.17.2.1. Patients’ own controlled drugs are the personal property of the patient. If a decision is taken that these controlled drugs are no longer needed, consent must be obtained from the patient to send the unwanted controlled drug to Pharmacy for destruction. If consent is not forthcoming, the issue should be discussed with the ward pharmacist. 12.17.2.2. The Trust reserves the right, for purposes of safeguard and public interest, to retain such controlled drugs where the original prescription has been cancelled or superseded. 12.17.2.3. Once consent has been obtained from the patient, the registered staff member must complete the Controlled Drug Returns/Destruction form (Appendix 10). 12.17.2.4. Patients’ own controlled drugs must not be destroyed on the ward/clinical area, with the exception of part used vials, ampoules or infusion bags or used patches, lozenges or other novel delivery devices. 12.17.2.5. Patients’ own controlled drugs can be handed to a pharmacist or pharmacy technician for return to Pharmacy. 12.17.2.6. On receipt in Pharmacy, Section B of the Controlled Drug Returns/Destruction form will be completed and a copy returned to the relevant ward/clinical area. This document must be retained in a safe place. 12.17.3. Controlled drugs no longer required on the ward 12.17.3.1. If controlled drugs are no longer required on the ward (eg the patient’s drug treatment has changed, patient has been discharged or deceased), they should be returned to Pharmacy as soon as possible, together with a completed Controlled Drugs Destruction Form (Appendix 10). 12.17.3.2. For Wards or Departments who do not have a regular Pharmacist visit, a Pharmacist can be asked to attend or a Registered Nurse/Midwife, can complete the controlled drugs register, a Controlled Drug Returns/Destruction Form, as in 9.1 above. MM0000 Medicines Code Page 96 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 12.17.4. Disposal of controlled drugs on wards/clinical areas 12.17.4.1. Small amounts of controlled drugs can be destroyed on wards/clinical areas, including: Doses which have been prepared for administration but not administered Partly used doses, vials, ampoules or infusion bags Liquid preparations of controlled drugs, where less than a dose remains Disposal of broken/defective ampoules 12.17.4.2. All other controlled drugs must be returned to Pharmacy, (see section 12.17). 12.17.4.3. If a controlled drug is prepared for administration (e.g. removed from its original container in a way that it cannot be replaced) but is not administered, it must be disposed of into the CD waste bin (purple) in the presence of an authorised witness. The contents of any ampoule or infusion bag opened, and not required, must be emptied into the CD waste bin (purple). The drug must be rendered irretrievable using denaturing gel/granules. 12.17.4.4. Liquid preparations for controlled drugs where less than a dose remains this should be disposed of in the CD waste bin (purple), in the presence of an authorised witness. 12.17.4.5. The authorised witness MUST provide the second check. 12.17.4.6. The reason for disposal must be recorded in the register and the witness must only sign the register once the controlled drug has been disposed of as outlined above. 12.17.4.7. Accidental breakage of ampoules, and other fragile containers, has been known to occur from time to time. In this circumstance, the drug should be disposed of in the CD waste bin (purple), in the presence of an authorised witness. 12.17.4.8. The ampoule/s need to be accounted for so should be signed out of the ward controlled drugs record book by two registered practitioners, stating the reason. MM0000 Medicines Code Page 97 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 12.17.4.9. In cases of accidental breakage a datix incident should be completed and made reference to in the controlled drugs book. 12.17.4.10. If a CD medicine is found to be defective (e.g. ampoules cracked, appears cloudy), the item/s should be marked ‘do not use’ and retained in the controlled drugs cupboard and Pharmacy contacted. 12.17.4.11. Authorised witnesses MUST be involved in the disposal of controlled drugs, this will be either: A registered prescriber A registered nurse/midwife A registered pharmacist A registered operating department practitioner (ODP) A pharmacy technician 12.18. Stock checks of CDs in ward/clinical areas and theatres 12.18.1. Frequency of stock checks must be agreed in advance with Pharmacy and must be no less frequent than once daily. 12.18.2. Stock checks must be carried out by two registered healthcare practitioners (nurses, midwives, operating department practitioners, doctors, pharmacists, pharmacy technicians). 12.18.3. An effective stock check must include the removal of all the contents of the controlled drug cupboard with each controlled drug replaced in the controlled drug cupboard once it has been checked against the relevant entry in the controlled drugs register. 12.18.4. Unopened packs with tamper evident seals should be left intact during the stock checking process. 12.18.5. Stock balances of liquid controlled drugs should be checked by visual inspection only, with balances confirmed on the completion of each bottle. MM0000 Medicines Code Page 98 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 12.18.6. An end volume discrepancy greater than 5% must be reported to the controlled drug keyholder immediately, every possible step should be taken to identify the cause of the discrepancy. 12.18.7. As each controlled drug is checked, signatures of the primary checker and the witness must be made against the final entry on the relevant page in the controlled drugs Register. 12.18.8. It is permissible, but not mandatory, to record the date and time of stock checks, together with names and signatures of the two practitioners, in a separate record book. 12.18.9. Any discrepancies identified during the controlled drug stock check must be reported to the controlled drug keyholder immediately. 12.18.10. If any discrepancy in a Controlled Drug quantity is discovered, every possible step should be taken to identify the cause of the discrepancy and/or correct the errors/omission(s) in the Ward CDs Record Book (sample page shown in Appendix 11) or the Theatre CDs Record Book (sample page shown in Appendix 12). Flow diagram of the procedure to follow when a discrepancy is discovered in the Ward CDs Record Book. 12.18.11. If the discrepancy cannot be resolved and/or corrected during the shift having performed a preliminary investigation, the Clinical Ward/ Department Manager should be informed. Out of hours the Clinical Site Manager should be contacted and the matter reported to the Accountable Officer or their nominated deputy the next working day. 12.18.12. If the balance is adjusted in the CD Record Book, this should be carried out by making a separate entry. 12.18.13. There should be no unexplained gaps in the running balance. The corrected balance must be countersigned by a Pharmacist/Pharmacy Technician. 12.18.14. A datix report MUST be completed for each discrepancy with the incident report referenced in the CD record book. MM0000 Medicines Code Page 99 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 12.18.15. The Trust’s Accountable Officer for CDs should be informed in the case of all major incidents or those where there is suspicion of wider fraud/misuse. 12.18.16. The Police must be informed of major or suspicious CD Incidents at the discretion of the Accountable Officer in consultation with the Local Security Management Specialist (LSMS) and the Trust Policy for the Reporting and Management of Serious Incidents (S01) followed. 12.18.17. In addition, a quarterly controlled drug check must take place. This will be arranged by Pharmacy at a mutually convenient time and should be carried out jointly by a registered nurse/midwife/ODP and a Pharmacy technician/pharmacist. 12.19. Abusable Medicines 12.19.1. In addition to Controlled Drugs, a number of prescription only medicines are sometimes subject to misuse, abuse or diversion, including common analgesics and some anaesthetic agents. 12.19.2. Abusable medicines MUST be stored in a locked medicines cupboard, and key holders must satisfy themselves that these are secured, and that requests to access stock are legitimate. 12.19.3. Regular usage reports are supplied by pharmacy and must be reviewed by senior clinical staff in charge of wards and departments to confirm that usage is within normal limits, and reflects current clinical practice. 12.19.3.1. Pharmacy MUST be notified of any change in clinical practice so that stock levels can be adjusted. 12.19.3.2. Ward and department managers MUST investigate any deviation from expected use, and document the deviation and investigation on a datix incident report, where this is not adequately explained (e.g. by checking patient prescriptions) MM0000 Medicines Code Page 100 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 12.19.3.3. Unresolved deviations MUST be reported to the Responsible Pharmacist, and where diversion or misuse is suspected, to the Accountable Officer immediately. 12.19.3.4. Staff should be aware of the signs that might indicate abuse or diversion of medicines (e.g. changes in an individual’s behaviour such as lack of concentration, regular unexplained absences from the work area, a change in character, or other ‘odd’ behaviour) and take appropriate action. 12.20. Illicit Substances 12.20.1. Patients and visitors will sometimes bring suspected illicit or unknown substances into hospital. Staff are reminded to be vigilant and report any suspicion to the senior registered practitioner in charge. 12.20.2. Where these represent a small quantity ‘for personal use’, then the patient should be asked to surrender these for destruction. Staff have no automatic right to search a patient’s belongings and if considered necessary consent must be obtained. 12.20.3. The suspected illicit substance should be stored in the CD cupboard for retrieval by a pharmacist using the ‘Controlled Drug Return Form’ (Appendix 10), for subsequent witnessed destruction, by an authorised witness. 12.20.4. The identity of the patient should NOT be documented for confidentiality, but for documentation purposes, only the ward location, a brief description of the suspected illicit substance (e.g. small white tablets, off-white powder, ‘spliff’), and the names of the registered Nurse and Pharmacist‘ handling the substance for purpose of destruction’. 12.20.5. If a patient refuses to give up a suspected illicit substance, then staff should refer to Local Security Management Specialist and may be referred to the Police, as below. MM0000 Medicines Code Page 101 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 12.20.6. Where the quantity is large or there is evidence of a criminal act taking place e.g. dealing on premises, then the Police may be called to investigate. The Police must only be involved with the agreement of the treating Consultant in charge of the patient’s care, and express permission of the Trust Accountable Officer for Controlled Drugs (Chief Pharmacist). 12.20.7. Illicit substances must NEVER be given back to a patient or their carer, as this constitutes an act of criminal supply and may be prosecuted under the Misuse of Drugs Act. 12.21. Controlled drug stationery 12.21.1. Controlled drug stationery includes: controlled drug order books controlled drug registers controlled drug TTA prescription forms and returns paperwork 12.21.2. Controlled drug stationery must be stored in a locked cupboard or drawer at all times and access restricted to those authorised to use or check it. 12.21.3. The controlled drug cupboard may be used to store controlled drug stationery. 12.21.4. Controlled drug stationery may be ordered from Pharmacy using a controlled drug stationery order form signed by a nurse/midwife/operating department practitioner or pharmacist. 12.21.5. A record of signatures of staff authorised to order controlled drug stationery will be held by Pharmacy. 12.21.6. The controlled drug stationery order must include the following: MM0000 Medicines Code Page 102 of 113 date name of hospital and ward signature of person ordering stationery quantity and type of stationery ordered Chairman: Graham Foster JP Chief Executive: David Sissling 12.21.7. Loss or theft of any controlled drug stationery must be reported immediately to the Designated Practitioner and within one working day to the CMT Head of Nursing and Chief Pharmacist (who will report to the Accountable Officer). 12.21.8. Completed controlled drug order books and registers must be retained for at least two years after the date of the last entry. MM0000 Medicines Code Page 103 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 13. UNLICENSED AND O FF LABEL MEDICINES In order to ensure that medicines are safe, effective and of appropriate quality, their manufacture and sale or supply is controlled by national and EU legislation. Accordingly, no medicinal product may be “placed on the market” unless a marketing authorisation (formerly a product licence) has been granted. However, in order to preserve prescribers’ clinical freedom, the legislation gives some exemptions from full control. Thus, medicinal products that are not licensed may be prescribed in order to fulfil special needs in individual patients, however, the consequences of prescribing are the responsibility of the individual clinician. 13.1. When can unlicensed medicines be used within the Trust 13.1.1. It is preferable that prescribers prescribe licensed medicines in accordance with the terms of their licence, however it is recognised that there may be instances where for clinical reasons that an unlicensed medicine(s) are necessary to meet the needs of the patient. 13.1.2. Where a licensed medicine is available it is Trust policy to normally prefer it to be chosen over off-licence or unlicensed medicines in order to reduce risk to patients. 13.2. Unlicensed Prescribing for Children 13.2.1. Customised formulations for individual children should be used only when a patient has a clinical need that cannot be adequately met by a licensed medicine. 13.2.2. Guidance on unlicensed and off-label medicines use and doses in paediatrics which is available in best practice publications, notably the BNF for Children and other peer reviewed national or international guidelines. 13.2.3. Where doses prescribed do not correspond with the BNF for Children, prescribers are asked to endorse the prescription with the reference source used. MM0000 Medicines Code Page 104 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 13.2.4. Where an unlicensed medicine is required for the first time the Consultant requesting must complete a Declaration of Responsibility for Prescribing Unlicensed and Off Label Medicines form and a Formulary Application (Appendix 13) form unless the medicine is being used in accordance with best practice publications. 13.2.5. Following review by New Medicines Group, if the request is approved the medicines will be added to the ‘list of unlicensed medicines /medicines for unlicensed use approved within the trust’, which will be maintained by NMG 13.3. Prescribing in Critical Care 13.3.1. Prescribing medicines for ‘off-label’ use is not uncommon in critical care areas. 13.3.2. Where an unlicensed medicine is required for the first time the Consultant requesting must complete a Declaration of Responsibility for Prescribing Unlicensed and Off Label Medicines form and a Formulary Application form unless the medicine is being used in accordance with best practice publications. 13.3.3. Following review by NMG if the request is approved the medicines will be added to the ‘list of unlicensed medicines /medicines for unlicensed use approved within the trust which will be maintained by NMG 13.4. Prescribing in Haematology/oncology 13.4.1. Prescribing in advance of a product license is not uncommon within haematology/oncology specialties. 13.4.2. Where an unlicensed medicine is prescribed for the first time the consultant must complete a Declaration of Responsibility for Prescribing Unlicensed and Off-label Medicines form. 13.4.3. A full formulary application will be required unless the medicine is being used in accordance with best practice publications (i.e. guidelines/protocols approved by LNR cancer network). MM0000 Medicines Code Page 105 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 13.4.4. Following review by NMG, if the request is approved the medicines will be added to the ‘list of unlicensed medicines /medicines for unlicensed use approved within the Trust’, which will be maintained by NMG 13.4.5. On occasion a clinician may be unaware that their intended use is outside of the product license. This can happen frequently where a class of drugs does not have the same licensed range of indications e.g. the proton pump inhibitors, or in certain clinical conditions e.g. prescribing during pregnancy. In any case of liability assessment this would be the basis of defence i.e. that the peer group practice clearly supported the prescriber. 13.5. Prescribers 13.5.1. Prescribers should be current in their knowledge to be aware when they prescribe an unlicensed medicine/licensed medicine in an unlicensed way 13.5.2. The clinical pharmacy team will assist in identifying these situations where possible. 13.5.3. Only Consultant medical staff are permitted to initiate the prescribing of unlicensed or off-label medicines. 13.5.4. Consultant medical staff prescribing an unlicensed or off-label medicine which is already, or has previously been stocked within the Trust will use the Declaration of Responsibility for Prescribing Unlicensed and Off-Label Medicines form (Appendix 13) to confirm to the Pharmacist that they understand the responsibilities of such prescribing. 13.5.5. When prescribing an unlicensed or off-label medicine new to the Trust an application to use an unlicensed medicine/licensed medicine in an unlicensed way MUST be submitted by the prescriber to the New Medicines Group (Appendix 13). The application will be subject to the same processes as an application for a licensed medicine. 13.5.6. In cases of urgent clinical need should be discussed with pharmacy. MM0000 Medicines Code Page 106 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 13.5.7. Junior medical staff may only continue to prescribe unlicensed and off-label medicines previously initiated within the Trust by a member of the consultant medical staff. 13.5.8. A prescriber will, whenever possible, ensure at the time of prescribing, that the patient (or carer) knows that an unlicensed or off-label medicine will be prescribed for them. 13.5.9. It is important the patient understands what a ‘special’ medicine is and a patient information leaflet (Appendix 14) to be provided to assist with this. Please contact pharmacy for assistance if additional information is required for patients who have protected characteristics. 13.5.10. The prescriber MUST record this activity within the medical notes in accordance with the Policy 130 Consent for treatment and examination. 13.5.11. Where it is deemed appropriate for General Practitioners to assume prescribing responsibility on discharge of the patient, information must be provided regarding the licence status, prescribing advice including dose any special monitoring requirements, and information on availability and supply. Shared Care Agreements may be required. 13.5.12. The GP may decline to take over the prescribing it is felt that this is not in the best interest of the patient. MM0000 Medicines Code Page 107 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 14. FP10 PRESCRIPTION FORMS FP10 prescription forms are used to prescribe for patients, enabling the patient to take the prescription to a community pharmacy to be dispensed. Unused blank FP10 prescription forms are liable to fraudulent misuse if lost or stolen. These forms are, therefore, designated by the NHS as “Controlled Stationery” and, as such, are subject to close control to minimise the opportunity for misappropriation and misuse. FP10 prescription forms that cannot be accounted for must be investigated and reported to the Accountable Officer or their deputy, with possible referral to the Police A national procedure exists for the reporting of missing FP10 prescriptions (the Accountable Officer will initiate this - Appendix 16). 14.1. Key Principles 14.1.1. FP10 pads must be kept secure at all times. 14.1.2. Only designated clinical areas are permitted to hold and use FP10 prescription forms. 14.1.3. If a need to use this stationery is identified, approval must be sought from Pharmacy to become a designated clinical area. 14.1.4. The nurse/manager in charge of the clinical area is responsible for the secure storage and use of FP10 prescription forms although the day-to-day management of this task may be delegated with a record maintained. 14.2. Ordering FP10 prescription forms from Pharmacy 14.2.1 Only authorised staff, whose signatures are registered with the Pharmacy Department for the purpose are permitted to order FP10 prescription forms as follows: 14.2.1.1. FP10 prescription forms can only be ordered on the specific 3-section FP10 order form (Appendix 15), signed by an authorised member of staff. MM0000 Medicines Code Page 108 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 14.2.1.2. A minimum of five working days’ notice is required, as forms may need to be ordered from the supplier. 14.2.1.3. Pharmacy will supply the requested forms, completing section 2 of the order form with the serial number of the first and last form in each pad supplied. 14.2.1.4. Prepared orders must be collected in person from Pharmacy and signed for by an authorised member of staff as above. 14.2.1.5. Immediately upon receipt in the clinical area, the FP10 prescription pads should be entered into the FP10 log book and stored in an approved locked cupboard/drawer. 14.3. Returning FP10 prescription forms 14.3.1. FP10 prescription forms no longer required MUST be returned to Pharmacy for secure disposal/re-use. They must not be disposed of by wards/departments directly. 14.3.2. The nurse in charge or other authorised member of staff must contact the Pharmacy Department to make arrangements for the return of the prescription forms to Pharmacy with the log book. 14.3.3. A designated member of the Pharmacy staff and the designated returning nurse will jointly check the forms against the logbook and the logbook will be endorsed accordingly with both persons signing. 14.3.4. Pharmacy will dispose of the returned forms or return them to stock for re-issue. 14.4. Secure storage and safekeeping of FP10 prescription forms when not in use 14.4.1. FP10 prescription forms must be stored in a controlled drug cupboard or other designated lockable cabinet/drawer approved in writing by the Chief Pharmacist. 14.4.2. The keys to this cupboard/drawer must be held only by the designated FP10 keyholder when ‘in use’ (see 14.5), or by the nurse in charge at other times. MM0000 Medicines Code Page 109 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 14.4.3. The keys should not be passed to others when they request keys to obtain other medicines. For clinical areas with restricted opening hours, there must be designated storage for the medicines and controlled drug/FP10 cupboard (see 14.4.1) keys approved by the Chief Pharmacist. 14.4.4. A log-book must be maintained of all FP10 prescriptions, detailing each individual prescription form by serial number with space to record the following details (as a minimum) when used: 14.4.4.1. date used: patient number prescriber An A5 notebook is recommended for use as a log book. There is no specific pre-printed stationery available for this. 14.4.4.2. The last digit in the serial number is a check-digit. For the purposes of checking, if this digit is disregarded the forms within a pad are numbered sequentially. 14.4.5. During each working day, a reconciliation check of actual prescription forms held against the log book must be performed by two nurses to identify missing or unaccounted-for forms. 14.4.6. A record of this check, and the nurses involved, should be recorded in the log book. 14.4.7. Any discrepancies between actual stock and log book must be investigated immediately as detailed in 14.7 and reported via datix to the Accountable Officer or their Deputy. 14.4.8. Areas with high FP10 usage may find it necessary to perform this reconciliation more frequently such as at each shift or clinic change. 14.5. Secure management of FP10 prescription forms ‘in-use’ 14.5.1. The period for which FP10s will be considered to be in use is dependent on the clinical area and the nature of the activity performed. MM0000 Medicines Code Page 110 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 14.5.2. A designated nurse must be authorised to control access to the FP10 prescription forms during each shift/clinic, in the absence of identification of another individual this will be the nurse in charge. 14.5.3. At the start of the shift the designated nurse MUST sign the logbook to accept responsibility and keys for FP10 prescription forms. 14.5.4. At the start of the shift two nurses (one MUST be the authorised nurse) must undertake a reconciliation of prescription forms held against the log book. This replaces the daily check specified above and any discrepancies between actual stock and log book must be investigated immediately as detailed in 14.7. 14.5.5. Prescribers needing a FP10 prescription form will make a request to the designated nurse who will obtain a form from the FP10 cupboard/drawer and issue it to the prescriber. 14.5.6. FP10 prescription forms that are requested but subsequently not required must be returned to the designated nurse as soon as possible. Blank forms MUST NEVER be left unattended. 14.5.7. At the time of issue, the designated nurse will be responsible for recording the date, prescriber and patient details (as a minimum) in the log book. 14.5.8. At the end of the shift/clinic all FP10 forms must be returned to the FP10 cupboard/drawer and the actual stock of FP10 forms must be reconciled against the log book and any discrepancies investigated immediately as detailed in 14.6. 14.5.9. Handover of the FP10 keys to the nurse in charge or to the next designated nurse must be recorded in the log book. 14.6. Unused and/or ‘spoilt’ FP10 prescription forms 14.6.1. If a FP10 prescription form is returned to the designated nurse unused (ie no longer required) he/she should endorse the logbook appropriately and return the form to ‘stock’ for re-use. 14.6.2. If an FP10 prescription form is “spoilt” eg prescribed incorrectly or otherwise unintentionally made unusable: 14.6.2.1. The prescriber should return the form to the designated nurse after clearly writing “SPOILT” and signing diagonally across the MM0000 Medicines Code Page 111 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling prescribing section of the form, and tearing the form in two or otherwise rendering it irretrievable. 14.6.2.2. The designated nurse should endorse the logbook accordingly and retain the two halves in the FP10 cupboard/drawer for return to Pharmacy when FP10 forms are next ordered. 14.7. Procedure for missing or unaccounted-for FP10 prescription forms 14.7.1. FP10 prescription forms that cannot be accounted for must be investigated and reported to the Accountable Officer or their deputy, with possible referral to the Police. 14.7.2. The majority of ‘missing’ FP10 prescription forms are a result of omitted recording or mis-recording of their use. This is the responsibility of the designated keyholder at the time the discrepancy is identified. 14.7.3. The procedures detailed above are designed to ensure that unaccounted-for FP10 prescription forms are identified at the earliest opportunity. Increasing the likelihood of swift resolution of the issue, whilst minimising the work required to resolve. 14.7.4. All instances of missing/unaccounted-for FP10 forms must be investigated and reported via datix as soon as they are identified. 14.7.5. The ward/clinic manager should also be informed immediately, who will take charge of the investigation. 14.7.6. The Accountable Officer should be informed (via the on-call pharmacist if necessary) before investigation commences, with details of the loss, and may be able to offer advice to assist the investigation additional to that outlined below. 14.7.7. The investigation will vary according to clinical area but (until resolved) should involve activities similar to:- 14.7.7.1. Physical check of all areas where the prescription pad may have been in use, including clinic rooms, floors, desk drawers, relevant casenotes and wastepaper bins, etc; MM0000 Medicines Code Page 112 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling 14.7.7.2. Check for corroborating entries in other parts of the healthcare record e.g. relevant casenotes, to identify if usage has been omitted in the log book; 14.7.7.3. Discussion with all nursing and medical staff on duty to identify possible use or ’wasting’ of prescription forms unaccounted for in the log book. 14.7.8. If investigation resolves the issue, the logbook should be updated appropriately and the nurse in charge must inform the Accountable Officer (or on-call pharmacist if already informed of loss earlier) and ensure that the incident is recorded via the Trust’s Datix incident reporting system. 14.7.9. If required the Accountable Officer will consult with the Trust Security Officer in relation to police involvement who may commence their own investigation. 14.7.10. The Accountable Officer will initiate the NHS Protection procedure for missing FP10 prescription forms if required (Appendix 16). 14.7.11. Any further action will be led the Accountable Officer and/or Trust Security Officer, or as a result of any police investigation. 14.8. Prescribing on FP10 prescription pads 14.8.1 When prescribing using an FP10 prescription form, the prescriber should make a specific FP10 annotation in the patient’s case notes. This is good practice and will assist any investigation of ‘missing’ FP10 prescription forms. 14.8.2 For detailed prescribing guidance see Section 4. Prescribing. 14.9 Monitoring compliance and effectiveness 14.9.1 Monitoring compliance of the document will be the through the quarterly medicines safety and security audits. 14.9.2 Reports from these audits will be submitted to the Medicines Management Committee and subsequent action plans will be implemented. MM0000 Medicines Code Page 113 of 113 Chairman: Graham Foster JP Chief Executive: David Sissling




















































































































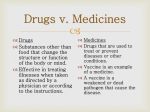

![My_Body[1] - Junior2TopicWiki](http://s1.studyres.com/store/data/008060165_1-be31cd2568d5e2c9fee6ce67732b07b4-150x150.png)



